You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Complete edentulism of either one or both arches in the oral cavity causes impaired mastication, and individuals who are afflicted with this condition are considered orally handicapped.1 To correct this disability, teeth can be replaced with a removable prosthesis (denture), or dental implants can be utilized to facilitate fabrication of a removable (overdenture) or fixed dental rehabilitation.
There are situations when specific criteria (eg, esthetics, phonetics, lip and facial support) dictate the type of prosthesis to use (Table 1 and Table 2).2 As indicated in these tables, a removable prosthesis can accommodate a range of anatomical variations that would be difficult to satisfy with a fixed prosthesis. Such variations may include a deformed ridge, a very large interarch space, or a Class III skeletal interarch relationship (Figure 1). Determining factors with respect to choosing a fixed or removable prosthesis are largely dependent on patient preference, anatomic considerations, choice of materials, and cost.1,3 For patients with considerable bone resorption who request a fixed prosthesis, either CAD/CAM titanium hybrid or monolithic zirconia represent fabrication methods that can be used to provide a fixed prosthesis when there is a large interarch space.
Potential disadvantages associated with fabrication of a removable appliance include patient non-acceptance; the size of the prosthesis, which often is bulky; and possible movement of an overdenture in the mandible if only two implants are used to retain the appliance. The latter can result in posterior bone loss due to denture base rotation.4
This article addresses management of the edentulous patient with a removable implant-supported prosthesis.
Chronological Perspective and Design Concepts
Historically, dental implants were first used to support fixed implant prostheses, and multiple implants (usually at least five implants) were employed to retain full-arch restorations.5-7 Cases were fabricated in a manner that left the prosthesis elevated above the gingiva and were referred to as being "high and dry" (Figure 2).8 These rehabilitations often were esthetically compromised, and food would frequently become trapped under the prosthesis. Subsequently, based on the success of dental implants, the concept of using them to retain a removable prosthesis was introduced.5 Pertinently, in 2002 the McGill Conference issued a consensus statement that concluded the use of mandibular overdentures retained by two dental implants is the preferred treatment when compared to conventional dentures for mandibular edentulous patients.7 Currently, implant-supported overdentures are predictable and commonly used prostheses.5,9-11
In the past, fixed prostheses were thought to be rigid (no rotation) and removable prostheses non-rigid (rotation). However, a removable implant overdenture can function either non-rigidly or rigidly.11 The difference between the two designs is determined by the number and distribution of inserted implants and jaw shape (eg, U-shaped jaw versus V-shaped).12 For example, three implants placed in a relatively straight line in a U-shaped jaw results in a non-rigid or rotational prosthesis (Figure 3). In contrast, if three implants are placed with wider distribution in a V-shaped jaw, the prosthesis will function rigidly or non-rotationally (Figure 3). In the mandible, a rigid or non-rigid design is acceptable; in the maxilla, however, only a rigid design should be used, because maxillary bone is 1.8 times less dense than mandibular bone and more susceptible to osseous resorption due to rotational movements.13
The projected anterior-posterior (A-P) spread of implants must also be assessed, as this will help determine acceptable cantilever length to be supported by retentive elements. A-P spread is the distance from the center of the most anterior implant(s) to the distal aspect of the most posterior implants in the arch. Cantilever length that can be created distal to implants bilaterally ideally is determined by assessing the A-P spread and multiplying it by 1.5 in the mandible and maxilla.14,15 However, these calculations are based on literature addressing cantilever length off fixed prostheses and represent a general guideline.14,15 Furthermore, other factors, such as the number and distribution of implants placed, need to be considered when planning cantilever length.
Interdisciplinary Algorithm for Full-Arch Treatment
After medical and dental histories are recorded, preliminary clinical and radiographic examinations are conducted; the patient needs to be interviewed. At this juncture, rather than telling patients what they need, clinicians should ask them what they want. A logical sequence of planning and therapy can then be initiated.
The first critical clinical step for treatment of an edentulous arch is determination of the final tooth position for the future prosthesis; the clinician should then work backwards to ascertain the needed restorative volume.16-19 To facilitate acquisition of this information, study casts are required and a diagnostic wax-up is appropriate after the casts are articulated and vertical dimension of occlusion (VDO) is established.20-22 Traditional prosthodontic techniques to establish VDO include subjective methods that evaluate esthetics (eg, facial and lip contours) and objective techniques, which assess interocclusal rest space pertaining to phonetics. Based on the wax-up, the definitive prosthesis can be designed and a surgical guide prepared.It should be noted that that this process can also be accomplished in a digital fashion instead of using articulated stone casts. Virtual smile designs, however, based on the authors' clinical experience, offer minimal value because they do not address 3-dimensional considerations or the impact of tooth position and flange on lip and facial tissue support.
An integral aspect of prosthesis design is measuring available vertical restorative space on a model and within the oral cavity. This distance is measured from the edentulous ridge (soft tissue or bone) to the opposing dentition; this measurement will dictate what type of removable prosthesis can be fabricated (Figure 4).23 Table 3 lists the minimum amount of vertical space required for different types of removable prostheses to accommodate restorative components and materials. If there is a lack of restorative space but adequate bone, an alveolectomy can be performed to create additional space and/or, if possible, the VDO can be increased prosthetically.24,25 If adequate restorative space is unavailable and cannot be created, the type of planned prosthesis must be altered to ensure good esthetics and phonetics and to avoid functional problems.
A cone-beam computed tomography (CBCT) analysis, which provides 3D imaging, is helpful to ensure that sites selected for implant placement have an adequate amount of bone vertically and horizontally. The scan also can be used to plan ridge augmentations at bone-deficient sites.
Before implants are placed, a definitive prosthesis needs to be designed based on the following concerns: esthetics, available restorative space, patient preferences, fixed or removable prosthesis design, cost of CAD/CAM splinted versus unsplinted implants, the patient's age, aftercare considerations, opposing arch, and choice of materials. Thought also needs to be given to options pertaining to provisionalization of the patient during the treatment phase.
The surgical treatment plan should be developed with respect to number of implants; their position, depth, and angulation; immediate versus delayed placement; and one- versus two-stage implant insertion. It must be emphasized that implant dentistry is a prosthetic endeavor with a surgical protocol, not a surgical protocol with a prosthetic adventure.
Treatment of the Mandibular Arch
To restore a fully edentulous mandible, three options may be available: denture, fixed implant prosthesis, or overdentures supported by two or more implants.26 If two implants are placed the prosthesis is referred to as an implant-retained overdenture; if three or more implants are placed with wide distribution it is denoted as an implant-retained and -supported overdenture because the prosthesis does not rest on the ridge.27 A two-implant mandibular overdenture is often constructed for elderly edentulous patients who are uncomfortable wearing a denture or have ridges that are resorbed thereby precluding the attainment of good retention. In such cases, implants are usually placed intraforaminally. Note that age is not a contraindication for osseointegration to occur,28 therefore elderly patients should not be dissuaded from having an implant-retained overdenture.
A two-implant overdenture can be constructed using a one- or two-stage protocol. Two-stage procedures entail submerging the implants at the time of surgery and uncovering them after 3 months so they can be restored. This is often done if a bone graft is placed or if implants lack good primary stability. A one-stage procedure consists of placing healing abutments at the time of implant placement, relieving and relining the denture over the implants, and then waiting 2 to 3 months before attempting to load the prosthesis. Other protocols have involved placing permanent attachments and immediately loading the implants.29 While this is possible, there is increased risk that not all of the implants will attain osseointegration.30 Regarding survival rates of implants that are splinted (use of a bar overdenture) versus unsplinted, a 10-year study indicated that the state of the connection did not influence clinical success of implants in the edentulous mandible.31
Unsplinted Implants to Retain or Retain and Support an Overdenture
Two unsplinted implants can be attached to a mandibular denture with Locator™ or other attachments to provide retention. Locator attachments allow a 20-degree per implant divergence before detrimental wear occurs on retentive elements.32 During the initial period after denture fabrication, the patient may experience some soft-tissue abrasion. After 5 years, 50% of such dentures may need to be relined.33 The attachments also will experience differential wear depending on the relative implant parallelism between implants, occlusal forces, and fit of the denture under-surface.34 In general, two-implant-retained overdentures are simple to fabricate, predictable, inexpensive, and a highly efficacious treatment for edentulous patients.10 Regardless of the type of implant overdenture (retained or supported), patient satisfaction is greater than with conventional dentures and patients experience enhanced quality of life.10,35
Three implants supporting an overdenture may include an implant in the middle of the anterior segment to prevent denture tipping.36,37 A third implant also may be utilized if there is a V-shaped arch and doing so will result in an increased A-P spread.37,38 Four implants supporting an overdenture provide retention and support, and the alveolar ridge may be protected from ridge atrophy caused by pressure applied to the bone by the denture.27
Generally, an increase in the number of implants does not facilitate a higher success rate for mandibular overdentures,39 but additional implants may increase retention and reduce tipping of the overdenture. Note, paradoxically, as few as one implant placed in the midline to retain an overdenture may provide improved oral function and comfort for individuals who cannot afford a second implant.40
Mandibular Bar Overdentures
Various clinical situations may be advantageous for the fabrication of a bar overdenture, including: when there is excessive loss of soft and hard tissues; when implants cannot be placed relatively parallel to each other (Figure 5); when implants cannot be inserted in ideal locations due to the presence of anatomic structures, poor A-P spread, a U-shaped jaw, or Class III occlusion; or when a large vertical or horizontal discrepancy exists between the maxillary and mandibular ridges.41 Patients who are sensitive to bulky flanges on a denture may also benefit from a bar overdenture because flanges can be reduced in size. It should be noted, however, that a bar overdenture is generally more costly than an unsplinted design and considerably more difficult to retrofit to an existing denture.
Bar overdentures may have a variety of designs and require more restorative space compared to unsplinted options (Table 3).42 The bar could extend the full length of the restored ridge (depending on number of implants) connecting all of the implants, or there may be several bars with cantilevers (Figure 5). Generally, single retentive elements offer only retention (resisting movement in a vertical plane), but bars also provide stability (resisting movement in a horizontal plane) and indirect retention (resisting movement in a rotational dimension). Usually, mastication is equally effective when a bar overdenture or fixed prosthesis is constructed.43 Similar to a fixed prosthesis, a bar overdenture functions rigidly. Milled bars require less maintenance than round bars and are usually the design of choice,40,44 because a milled bar (bar unit) affords only one path of insertion and a rigid design, whereas a round bar has several paths of insertions and rotational features. Typically, rotational designs induce increased replacement of retentive components compared to rigid options.44
Surgical Protocol for Implant Mandibular Overdentures
Clinical and radiographic assessments help ensure selected implant sites are suitable for implant placement. If two implants are to support a mandibular overdenture, ideally they should be placed in the canine area and be around 20 mm apart.10 In this regard, if a line is drawn between the two implants, it defines a line of rotation that the overdenture experiences. Implants can be placed in alternate sites that are not symmetrical. For instance, they can be inserted in the first bicuspid site on one side and a lateral incisor location on the contralateral side, depending on where adequate bone is present to retain an implant. Angulated locators are available that can compensate for implants that are placed more divergently than 20 degrees, or newer-designed straight overdenture abutments may be used that can treat up to 30 degrees between implants.32 If four implants are used to support an overdenture, having two on one side of the arch and two on the other side is preferred; however, they do not need to be placed symmetrically.
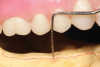
Several other aspects of the surgical protocol are worth noting. The surgical guide can be altered by eliminating the entire facial aspect of the guide (Figure 6), which allows improved visual access as opposed to taking a lingual approach where the facial aspect of the guide is left intact. For a two-implant overdenture, once the flap is reflected, the trajectory of the residual ridge should be evaluated. The first implant gets placed parallel to the residual ridge to facilitate a path of draw, and the second anterior implant gets placed parallel to the first implant. If four implants are to be placed, the posterior implants should be placed parallel to the anterior implants. For unsplinted implants, the initial osteotomy should be about 9 mm to 10 mm lingual to the facial tooth position if there is advanced alveolar ridge resorption. Another way of managing this situation is to use CBCT-based planning in conjunction with either static resin guided surgery or direct camera navigation or robotics to ensure parallelism of implant placement.45
When placing implants for a mandibular overdenture, circumstances may be encountered where the mandible is severely atrophied and the floor of the mouth is at the level of the height of the ridge. In these situations, after implant and abutment placement, the flaps upon suturing tend to ride over the healing abutment. Bone sutures can be used to ensure that tissues will be positioned snugly against the bone (Figure 7).
With respect to implant parallelism, unsplinted implant designs must have implants placed that are as parallel as possible to avoid retentive element wear; this is less important for splinted concepts, because a substructure bar can accommodate unparalleled implants. For an unsplinted design, there is no precise minimum or maximum distance between implants, but for implants retaining a bar, the recommended distance between implants is 10 mm (measured from center to center between two implants) to accommodate retentive elements (Figure 8). For example, Hader clips and most retentive elements require 5 mm of space and 2.5 mm of titanium on each side.23
Notably, different principles apply to implant distribution for mandibular and maxillary overdentures (Table 4). For example, in the mandible, implants can be positioned anterior to the mental foramen to retain a two-implant overdenture or four or more implants can be placed to fully support an overdenture. In contrast, maxillary overdentures always require a wider distribution of implants both anteriorly and posteriorly to avoid prosthesis tipping; thus, an anterior concentration of implants should be avoided for maxillary overdentures.
Clinicians need to avoid common mistakes associated with the fabrication of mandibular overdentures. Improper positioning of dental implants may occur if a surgical guide is not used. This can result in malposed implants that may be too facially positioned, and attachments may then encroach upon prosthetic teeth. If implants are placed too lingually, the plastic flange will need to be extended and could interfere with speech or cause tongue discomfort.
Treatment of the Maxillary Arch
Two implant prosthetic options are available for the edentulous maxilla: a fixed implant prosthesis or a multiple implant overdenture. The maxilla has unique requirements for restoration concerning esthetics, phonetics, and prosthesis design. Historically, compared to a fixed prosthesis, maxillary overdentures were considered a poor choice for rehabilitation because they demonstrated a high failure rate.46 However, the contemporary literature provides a different perspective based on improvements in implant surfaces and because modern maxillary overdentures are more like fixed prostheses; they are rigid, and rough surface implants provide greater stability.47
The minimum number of implants to support a maxillary overdenture is four, but equally important is a wide distribution of implants that will support a rigid design.48 Four implants are needed for an unsplinted implant overdenture that uses single retentive elements49 or a bar overdenture.48 The implants do not have to be placed symmetrically on both sides of the maxilla. Other recommendations are that six or eight implants should be used to support a maxillary overdenture if there is advanced alveolar resorption.50
Regarding survival of unsplinted implants in the maxilla supporting an overdenture, it was suggested that at least one implant should be placed in the premaxilla to prevent anterior tipping of the prosthesis.49 Several reports provided data that indicated high survival rates after 5 years51and after 7 to 73 months.32 However, there are only a few long-term evaluations of this prosthetic design. In contrast, numerous papers have reported high survival rates when a bar retainer is used.48,52 Notably, unsplinted designs should be used with caution, especially in the maxilla, when there is a large discrepancy horizontally between implant position and the facial aspect of prosthetic teeth, as this will create a large horizontal cantilever and result in the need for increased prosthetic aftercare (eg, increased wear of retentive elements). With respect to surgical protocol when inserting implants in the maxilla for an unsplinted design, the authors suggest that anterior implants (at least two) be placed first and parallel to the residual ridge to facilitate prosthetic draw, and then the posterior implants be placed parallel to the anterior implants. This is suggested because the average tooth trajectory of the central incisors is about 110 degrees and the ridge inclines buccally.53
When implants are splinted using a bar, it is critical that adequate restorative space is available to accommodate the larger prosthesis compared to an unsplinted supported implant overdenture. The minimum vertical restorative space needed for an implant-supported overdenture using an unsplinted design is 7 mm, whereas the smallest vertical space for a bar overdenture is 11 mm (Table 3).17 While these are minimum dimensions, additional restorative space may be desirable to facilitate the fabrication process. A bar overdenture needs about 2 mm of peri-implant sulcus depth, 1 mm of soft tissue under the bar, 5 mm for the bar and attachment, and 2.5 mm to 3 mm to accommodate the thickness of the acrylic.23 Similar to mandibular implant overdentures, usually the osteotomy position should be about 9 mm to 10 mm lingual to the facial tooth position when there is advanced alveolar ridge resorption; this will allow for space for the titanium bar, retentive elements, acrylic, and full-sized denture tooth. Other factors to consider when a bar overdenture is fabricated is increased cost and difficulty performing hygiene. Generally, unsplinted designs are recommended for cases of minimal ridge resorption, and bars are suggested when there is moderate to advanced resorption combined with aberrant ridge relationships. All bars need to be fabricated with CAD/CAM technologies and not cast.
Regarding bar design, a primary bar could act as the substructure with a secondary bar acting as a superstructure (suprastructure). Use of secondary bars is preferred for maxillary overdentures, because they provide a metal-to-metal frictional fit, determine a distinct path of draw, and facilitate decreased prosthetic aftercare (Figure 9).54-57 The bar enables the overdenture to function like a fixed prosthesis. With respect to angulation of the implants, the substructure that is screwed into the implants provides a method to accommodate nonparallel implants and provide ideal parallelism of the retentive elements irrespective of implant position or angulation (Figure 10). For maxillary bar overdentures, either an anterior single bar or two bars posteriorly can be effectively used (Figure 10). The substructure is often necessary in the edentulous maxilla when the ridges in the posterior quadrants are divergent relative to each other.
All maxillary implant prostheses (fixed or removable) alter phonetics, and clear speech is a major factor in patient satisfaction.58 Generally, patients have more difficulty adjusting to speech when transitioning from a removable to a fixed prosthesis and less difficulty when changing from a removable denture to a maxillary implant overdenture. Patients should be aware of these factors before treatment is started.
Overdentures can be removed for personal and professional oral hygiene maintenance. These prostheses can be constructed with full or partial palatal coverage. Patients often prefer partial palatal coverage because it allows them to feel their palatal tissues, and some patients claim they can taste food and feel temperature alterations better than when the palate is fully covered.59,60
Conclusion
Implant overdentures represent an important component to contemporary implant dentistry. This modality often is the treatment of choice after consideration is given to preoperative patient-specific criteria, patient expectations, and financial factors. Importantly, the surgical protocols for implant overdentures are different than for fixed implant-supported options. Overall, the data indicate that an implant overdenture prosthesis provides predictable implant and prosthesis survival, improved stability, good function, and high patient satisfaction compared to conventional removable dentures.
About the Authors
Joseph Carpentieri, DDS
Assistant Clinical Professor, Department of Prosthodontics, College of Dental Medicine, Columbia University, New York, New York; Director of Clinical Education, Dental365™, New Hyde Park, New York; Private Practice, Surgical Implantology and Prosthodontics, White Plains, New York
Gary Greenstein, DDS, MS
Clinical Professor, Department of Periodontics, College of Dental Medicine, Columbia University, New York, New York; Private Practice, Surgical Implantology and Periodontics, Freehold, New Jersey
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Drago C, Carpentieri J. Treatment of maxillary jaws with dental implants: guidelines for treatment. J Prosthodont. 2011;20(5):336-347.
2. Carpentieri J. Treatment options for the edentulous mandible: clinical application of the two-implant overdenture. Pract Proced Aesthet Dent. 2004;16(2):105-112.
3. Heydecke G, Boudrias P, Awad MA, et al. Within-subjective comparisons of maxillary fixed and removable implant prostheses: patient satisfaction and choice of prosthesis. Clin Oral Implants Res. 2003;14(1):125-130.
4. Greenstein G, Cavallaro J. Dental implants typically help retain peri-implant vertical bone height: evidence-based analysis. Compend Contin Educ Dent. 2013;34(7):502-511.
5. Schmitt A, Zarb GA. The notion of implant-supported overdentures. J Prosthet Dent. 1998;79(1):60-65.
6. Awad MA, Lund JP, Dufresne E, Feine JS. Comparing the efficacy of mandibular implant-retained overdentures and conventional dentures among middle-aged edentulous patients: satisfaction and functional assessment. Int J Prosthodont. 2003;16(2):117-122.
7. Feine JS, Carlsson GE, Awad, MA, et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 24-25, 2002. Int J Oral Maxillofac Implants. 2002;17(4):601-602.
8. Fixed Hybrid Dentures: What Is This? OsseoNews website. Updated November 10, 2015. https://www.osseonews.com/patient/fixed-hybrid-dentures-what-is-this/. Accessed January 11, 2021.
9. Zhang Q, Jin X, Yu M, et al. Economic evaluation of implant-supported overdentures in edentulous patients: a systematic review. Int J Prosthodont. 2017;30(4):321-326.
10. Gotfredsen K, Holm B. Implant-supported mandibular overdentures retained with ball or bar attachments: a randomized prospective 5-year study. Int J Prosthodont. 2000;13(2):125-130.
11. Carpentieri JR, Tarnow DP. The two-implant mandibular overdenture as first-choice treatment objective. Pract Proced Aesthet Dent. 2003;15(10):750-752.
12. Pietrokovski J, Sorin S, Hirschfeld Z. The residual ridge in partially edentulous patients. J Prosthet Dent. 1976;36(2):150-158.
13. Kim YJ, Henkin J. Micro-computed tomography assessment of human alveolar bone: bone density and three-dimensional micro-architecture. Clin Implant Dent Relat Res. 2015;17(2):307-313.
14. Kosinski TF. Overdenture design to maximize stability and function. Dent Today. 2017;36(2):108-112.
15. Taruna M, Chittaranjan B, Sudheer N, et al. Prosthodontic perspective to All-on-4® concept for dental implants. J Clin Diagn Res. 2014;8(10):ZE16-ZE19.
16. Silverman MM. The comparative accuracy of the closest-speaking-space and the freeway space in measuring vertical dimension. J Acad Gen Dent. 1974;22(5):34-36.
17. Spear F. The maxillary central incisal edge: a key to esthetic and functional treatment planning. Compend Contin Educ Dent. 1999;20(6):512-516.
18. Spear F. Too much tooth, not enough tooth: making decisions about anterior tooth position. J Am Dent Assoc. 2010;141(1):93-96.
19. Misch CE. Guidelines for maxillary incisal edge position-a pilot study: the key is the canine. J Prosthodont. 2008;17(2):130-134.
20. McGee GF. Use of facial measurements in determining vertical dimension. J Am Dent Assoc. 1947;35(5):342-350.
21. Mack MR. Facially generated occlusal vertical dimension. Compend Contin Educ Dent. 1997;18(12):1183-1190.
22. Pound E. Utilizing speech to simplify a personalized denture service. J Prosthet Dent. 1970;24(6):586-600.
23. Carpentieri J, Greenstein G, Cavallaro J. Hierarchy of restorative space required for different types of dental implant prostheses. J Am Dent Assoc. 2019;150(8):695-706.
24. Misch CE, Goodacre CJ, Finley JM, et al. Consensus conference panel report: crown-height space guidelines for implant dentistry-Part 2. Implant Dent. 2006;15(2):113-121.
25. Fabbri G, Sorrentino R, Cannistraro G, et al. Increasing the vertical dimension of occlusion: a multicenter retrospective clinical comparative study on 100 patients with fixed tooth-supported, mixed, and implant-supported full-arch rehabilitations. Int J Periodontics Restorative Dent. 2018;38(3):323-335.
26. Kutkut A, Bertoli E, Frazer R, et al. A systematic review of studies comparing conventional complete denture and implant retained overdenture. J Prosthodont Res. 2018;62(1):1-9.
27. Assaf A, Chidiac JJ, Daas M. Revisiting implant-retained mandibular overdentures: planning according to treatment needs. Gen Dent. 2014;62(4):60-64.
28. Koszuta P, Grafka A, Koszuta A, et al. Effects of selected factors on the osseointegration of dental implants. Prz Menopauzalny. 2015;14(3):184-187.
29. Chiapasco M, Gatti C. Implant-retained mandibular overdentures with immediate loading: a 3- to 8-year prospective study on 328 implants. Clin Implant Dent Relat Res. 2003;5(1):29-38.
30. Zhu Y, Zheng X, Zeng G, et al. Clinical efficacy of early loading versus conventional loading of dental implants. Sci Rep. 2015;5:15995. doi: 10.1038/srep15995.
31. Naert I, Alsaadi G, van Steenberghe D, Quirynen M. A 10-year randomized clinical trial on the influence of splinted and unsplinted oral implants retaining mandibular overdentures: peri-implant outcome. Int J Oral Maxillofac Implants. 2004;19(5):695-702.
32. Locator R-Tx® Removable Attachment System [product brochure]. Palm Beach Gardens, FL: Zimmer Biomet Dental; 2019.
33. Felton D, Cooper L, Duqum I, et al; American College of Prosthodontists. Evidence-based guidelines for the care and maintenance of complete dentures: a publication of the American College of Prosthodontists. J Prosthodont. 2011;20 suppl 1:S1-S12.
34. Gross MD. Occlusion in implant dentistry. A review of the literature of prosthetic determinants and current concepts. Aust Dent J. 2008;53 suppl 1:S60-S68.
35. Sivaramakrishnan G, Sridharan K. Comparison of implant supported mandibular overdentures and conventional dentures on quality of life: a systematic review and meta-analysis of randomized controlled studies. Aust Dent J. 2016;61(4):482-488.
36. De Kok IJ, Chang KH, Lu TS, Cooper LF. Comparison of three-implant-supported fixed dentures and two-implant-retained overdentures in the edentulous mandible: a pilot study of treatment efficacy and patient satisfaction. Int J Oral Maxillofac Implants. 2011;26(2):415-426.
37. Gowd MS, Shankar T, Ranjan R, Singh A. Prosthetic consideration in implant-supported prosthesis: a review of literature. J Int Soc Prev Community Dent. 2017;7(suppl 1):S1-S7.
38. Mericske-Stern RD, Taylor TD, Belser U. Management of the edentulous patient. Clin Oral Implants Res. 2000;11 suppl 1:108-125.
39. Lee JY, Kim HY, Shin SW, Bryant SR. Number of implants for mandibular implant overdentures: a systematic review. J Adv Prosthodont. 2012;4(4):204-209.
40. Cordioli G, Majzoub Z, Castagna S. Mandibular overdentures anchored to single implants: a five-year prospective study. J Prosthet Dent. 1997;78(2):159-165.
41. Bueno-Samper A, Hernández-Aliaga M, Calvo-Guirado JL. The implant-supported milled bar overdenture: a literature review. Med Oral Patol Oral Cir Bucal. 2010;15(2):e375-e378.
42. Rinke S, Rasing H, Gersdorff N, et al. Implant-supported overdentures with different bar designs: a retrospective evaluation after 5-19 years of clinical function. J Adv Prosthodont. 2015;7(4):338-343.
43. de Albuquerque Júnior RF, Lund JP, Tang L, et al. Within-subject comparison of maxillary long-bar implant-retained prostheses with and without palatal coverage: patient-based outcomes. Clin Oral Implants Res. 2000;11(6):555-565.
44. Krennmair G, Krainhöfner M, Piehslinger E. The influence of bar design (round versus milled bar) on prosthodontic maintenance of mandibular overdentures supported by 4 implants: a 5-year prospective study. Int J Prosthodont. 2008;21(6):514-520.
45. D'haese J, Ackhurst J, Wismeijer D, et al. Current state of the art of computer-guided implant surgery. Periodontol 2000. 2017;73(1):121-133.
46. Watson CJ, Tinsley D, Sharma S. Implant complications and failures: the complete overdenture. Dent Update. 2001;28(5):234-240.
47. Oue H, Doi K, Oki Y, et al. Influence of implant surface topography on primary stability in a standardized osteoporosis rabbit model study. J Funct Biomater. 2015;6(1):143-152.
48. Laurito D, Lamazza L, Spink MJ, De Biase A. Tissue-supported dental implant prosthesis (overdenture): the search for the ideal protocol. A literature review. Ann Stomatol (Roma). 2012;3(1):2-10.
49. Cavallaro JS Jr, Tarnow DP. Unsplinted implants retaining maxillary overdentures with partial palatal coverage: report of 5 consecutive cases. Int J Oral Maxillofac Implants. 2007;22(5):808-814.
50. Slot W, Raghoebar GM, Cune MS, et al. Maxillary overdentures supported by four or six implants in the anterior region: 5-year results from a randomized controlled trial. J Clin Periodontol. 2016;43(12):1180-1187.
51. Cavallaro J, Greenstein G. Unsplinted implants retaining maxillary removable overdentures with partial palatal coverage: lessons learned from 20 cases. Dental Resource Magazine. 2012;Winter/Spring:12-15,21.
52. Sangcharearn Y, Ho C. Maxillary incisor angulation and its effect on molar relationships. Angle Orthod. 2007;77(2):221-225.
53. Corsalini M, Di Venere D, Stefanachi G, et al. Maxillary overdenture retained with an implant support CAD-CAM bar: a 4 years follow up case. Open Dent J. 2017;11:247-256.
54. Zitzmann NU, Marinello CP. Treatment outcomes of fixed or removable implant-supported prostheses in the edentulous maxilla. Part I: patients' assessments. J Prosthet Dent. 2000;83(4):424-433.
55. Zitzmann NU, Marinello CP. Treatment outcomes of fixed or removable implant-supported prostheses in the edentulous maxilla. Part II: clinical findings. J Prosthet Dent. 2000;83(4):434-442.
56. Krennmair G, Piehslinger E. Removable implant-supported maxillary prostheses anchored on milled bars: a retrospective evaluation of two concepts. Int J Prosthodont. 2009;22(6):576-578.
57. Visser A, Raghoebar GM, Meijer HJ, Vissink A. Implant-retained maxillary overdentures on milled bar suprastructures: a 10-year follow-up of surgical and prosthetic care and aftercare. Int J Prosthodont. 2009;22(2):181-192.
58. Heydecke G, McFarland DH, Feine JS, Lund JP. Speech with maxillary implant prostheses: ratings of articulation. J Dent Res. 2004;83(3):236-240.
59. Ochiai KT, Williams BH, Hojo S, et al. Photoelastic analysis of the effect of palatal support on various implant-supported overdenture designs. J Prosthet Dent. 2004;91(5):421-427.
60. Misch CE. Partial and complete edentulous maxilla implant treatment plans: fixed and overdenture prostheses. In: Misch CE, ed. Dental Implant Prosthetics. St. Louis, MO: Mosby; 2005:281-294.