You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Provisional restorations are often thought of as interim, or "temporary," space holders placed over prepared teeth until the final restorations can be fabricated and inserted. In actuality, provisionals can provide a great deal of vital information for esthetic, phonetic, and functional determinants of a patient. Once the provisionals are placed in the mouth, a verification process can begin where the interaction of esthetic contours and lip dynamics may be analyzed. This is followed by ensuring the provisionals pose no speech impediment to the patient due to newly developed length and/or position of incisal edges. Lastly, the verification process entails confirming that the occlusion is even and balanced to minimize the chance of a lost or broken provisional that would require an emergency visit for re-cementation. Therefore, when the clinician envisions the final restoration throughout the process, a provisional restoration is more than just a "temporary"; it serves as a gateway to predictable esthetic results.
Prior to the Provisional Process
Several steps that contribute to the success of a restorative treatment plan should be carried out before the provisionalization process actually begins. First, the clinician should conduct a comprehensive assessment of the patient's needs and risk factors.1,2 This is followed by treatment planning and establishing a diagnostic wax-up that aids as a blueprint design for newly established contours.3 These new contours could be necessary for functional reasons associated with wear, or they may be needed to achieve esthetic changes that the patient desires. Regardless of the reasoning, the provisionals that will be duplicated from the wax-up are not an arbitrary guess but rather a calculated assessment established from the treatment planning process.4,5
Provisionals provide the dentist with a medium to test and verify the newly proposed contours from the diagnostic wax-up in the mouth. Once the provisionals are placed into the mouth the clinician needs to be able to assess and apply objective and subjective criteria to ensure success moving forward. A simple stepwise process can be established for refining provisional contours in the mouth that satisfy the elements of esthetics, phonetics, and function. This, in turn, allows for any needed refinements to be calculated and efficiently performed.
This article outlines a systematic process for establishing customized provisional contours to satisfy the functional esthetic matrix of a given patient for anterior restorations (Figure 1).6,7
The Provisional Process
Keeping in mind the adage "form follows function," the first step in the process (denoted by "1" in Figure 1) involves establishing a stable centric holding contact on the lingual aspect of the maxillary anterior teeth. This holding contact paired with both temporomandibular joints seated in centric relation allows for a stable functional starting point to propel the case forward.6 This contact is initially treatment planned using a diagnostic wax-up on a semiadjustable articulator, and refinements will be needed intraorally. The adjustments to be made will be to the lingual surface of the maxillary anterior teeth in conjunction with the leading edge of the mandibular incisors.
Once the stable stop is confirmed, attention can then be shifted to how the lips begin to interact with the facial surfaces of the teeth, ie, the second and third adjustment areas (denoted by "2" and "3" in Figure 1). Starting at the gingival one-third and then the middle one-third of the provisionals, the clinician's goal at this point is to create a smooth convex plane emerging from the gingival margin. Any overcontoured portion of the provisional should be removed to allow natural unimpeded movement of the upper lip.7 Preventing overcontoured provisionals also helps allow the patient to adequately clean the provisionals, which is paramount for gingival tissue health upon delivery of the final restorations.8
Transitioning coronally, the fourth adjustment involves determining the horizontal and vertical position of the incisal edges (denoted by "4" in Figure 1). As the lips come together the incisal edge should be tailored in a horizontal direction (ie, facial or lingual) toward the inner vermillion border of the lower lip. This enables the incisal edge to not impede the lower lip upon closing for swallowing or coming in close contact for speech.
Determining the vertical position of the incisal edge is crucial in customizing the functional esthetic matrix for the patient. This step can be done utilizing the repose (rest) position of a patient while taking into account the patient's age. The renowned Vig and Brundo study explained that in the repose position, younger patients tend to reveal more maxillary incisal edge while older patients tend to display more mandibular incisal edge.9 As the patient then transitions into a smile the convexity of the incisal edges should have a symmetrical balance with the lower lip.10
The testing of phonetics using the "F" and "V" sounds is critically important to analyze the horizontal and vertical positions of the incisal edge with lip dynamics during speech. The maxillary incisal edge should interact effortlessly with the inner vermillion border of the lower lip.11 In the author's experience, if the patient is straining to produce subtle "F" and "V" sounds, the error often is that the incisal edges are too long and too far facially. This can be remedied by making very minute adjustments to the labioincisal one-third of the provisional restorations.
Once the position of the incisal edge has been tested visually and phonetically, the fifth step is to begin marrying the functional and esthetic contours (denoted by "5" in Figure 1). This is done by establishing the anterior guidance in harmony with the envelope of function. By having the patient close to the stable centric stops the goal at this point is to allow for smooth excursive movements down the lingual surfaces of the teeth all the way to the incisal edge. This appears as a smooth contiguous line from the centric stop to the incisal edge. If there is a point in which the line terminates and starts again, posterior interference is a probable cause. With the clinician aiming to achieve smooth anterior guidance that allows for posterior disclusion and decreases muscle activity, posterior interference should be removed.12-14 After the inside-out path has been tested and confirmed, the patient is transitioned to an upright seated position. This is done to assess for whether there is a need for long centric and to harmonize the envelope of function, or outside-in, movement. Any noted interferences of the anterior teeth are removed to ensure that an uninhibited path to closure can be achieved.15
The sixth and final contour to be established is the defining of the cingulum area, ie, where the transition occurs from the stable centric stop to the gingival margin on the lingual surface (denoted by "6" in Figure 1). The intention is to create a smooth transition that is not too prominent so it does not impede the tongue during the making of the phonetic sounds of "S," "T," and "D."
Finally, the provisionals are detailed for further esthetic enhancements. This may include defining line angles, surface texture, incisal embrasures, etc. During this step it is important to allow patients to express their desires for the detailing. For example, a patient might prefer a more rounded tooth rather than sharp angles. This is a key consideration, because while the functional and phonetic components are objective factors, esthetics can be somewhat subjective, and the patient's preferences for final contours, shape, size, and shade must be taken into account.16,17
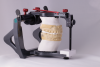
Once the provisionals have been verified in the mouth for esthetics, phonetics, and function following the stepwise process, the term "approved provisionals" can be applied. The newly approved contours need to be transferred to the laboratory for the fabrication of the final restorations in order to maintain predictability of the restorative process. This is done by taking a full series of photographs to demonstrate to the ceramist how the contours interact with the lip dynamics at rest and smiling. This is followed by taking an impression and facebow of the approved provisionals in the mouth.18,19 The maxillary cast of the approved provisionals can be facebow-mounted on a semiadjustable articulator and sent to the laboratory along with the photographs, bite registration, and mandibular cast.
Once the laboratory receives this information, the mandibular cast will be mounted to the approved provisionals, and then the maxillary master die cast will be cross-mounted to the mandibular opposing cast. Completing the mounting in this manner allows the lab to establish a relationship between the provisional contours and the preparations. The lab can then fabricate a facial reduction matrix along with a custom incisal guide table. These two key components provide the lab with a 3-dimensional (3D) relationship of the approved provisionals to the preparations, which is known as the functional esthetic matrix. The technician can then follow the contours provided by the facial matrix for esthetics and the custom incisal guide table for the functional requirements. Collaborating with a lab that understands the concepts of working within the 3D functional esthetic matrix is paramount to achieving the consistency and predictability needed for success.20 In essence, the final restorations are not a completely new design; they are simply a replication of the provisionals, but are now in porcelain rather than provisional bis-acryl material.
It is worth noting that while the use of current digital and CAD/CAM technologies continues to advance in dentistry and can be highly effective in duplicating provisional restorations, many practitioners still have yet to implement those capabilities in their offices-thus, the importance of this conventional process. Moreover, clinicians can benefit by knowing and understanding analog practices for common, everyday esthetic cases before transitioning to digital protocols. Clinicians should also realize that it is still very much possible to achieve accurate results without the use of digital technology.
The following case example illustrates this provisional process for obtaining appropriate esthetics, phonetics, and function.
Case Example
A 75-year-old man presented to the office with severe anterior tooth wear (Figure 2). After meticulous record-taking and thorough planning, a treatment plan was established to rehabilitate the patient to prevent further breakdown. The treatment plan consisted of crowns for teeth Nos. 4 through 13, 20, 21, 28, and 29 coupled with anterior incisal composites for teeth Nos. 22 through 27. Composites were utilized for cost savings to the patient and as a way to establish a more stable occlusion. It was explained to the patient that the composites could be transitioned to veneers at a later date if and when he desired to do so.
Once the crown preparations were complete and the provisionals were in place, the sequential adjustments outlined earlier were performed. The centric holding stops on the lingual surface of the provisional restorations of the maxillary anterior teeth were established in combination with defining the leading incisofacial surface of the mandibular incisors (Figure 3 and Figure 4).
Next, the lip support on the facial surface starting with the gingival and extending into the middle one-third of the provisional was contoured using a thin contouring and polishing disc (Figure 5 and Figure 6); the clinician checked to ensure the patient's upper lip did not catch on the facial surface when moving upward and downward. The facial contour was continued coronally on the facial surface of the tooth to ensure the lower lip closure path was not impeded at the labioincisal one-third (Figure 7). Should the patient appear to have difficulty closing his or her lips naturally, a clinician's first inclination might be to shorten the incisal edge vertically. However the first attempted solution should be to contour the labioincisal one-third of the tooth in a horizontal direction rather than shortening the length in a vertical direction. The overall goal, as it was in this case, is to have a contiguous convex facial surface of the provisional restorations (Figure 8).
After the horizontal position of the incisal edge has been set, the vertical position is analyzed using the rest position. Given the patient's age in this case, it was determined that more of the mandibular incisal edge would typically be on display (Figure 9).9 As the patient transitioned into a smile, the incisal edges displayed a convex smile arc and mimicked the symmetry of the lower lip (Figure 10) with the labioincisal one-third angling toward the inner vermillion border of the lower lip (Figure 11).
The horizontal and vertical positions of the incisal edge were tested phonetically with "F" and "V" sounds. The patient was instructed to count from 50 to 59 and monitored to see if any impediment was noticed. If an impediment is perceived, the labioincisal one-third may be reduced or the incisal edges shortened slightly. Once the patient feels comfortable the adjustment is complete.
Next, the functional and esthetic components are married together; the patient was instructed to bite to bring his upper and lower teeth together and then move his mandible to the right, to the left, and in protrusive movements. The anterior guidance should be a smooth contiguous path from the stable centric stop to the incisal edges of the teeth (Figure 12). Any and all posterior interferences get removed to create a more stable neuromuscular system (Figure 13 and Figure 14). This is followed by having the patient sit upright and checking the need for long centric and removing any envelope of function interferences during a chewing motion with full-arch articulating paper in the mouth.
The last contour to be developed is the cingulum from the stable centric stop to the gingival. This is done by creating a smooth contour that is bulky or overcontoured. It, too, is tested phonetically with "S," "T," and "D" sounds. After being released from the appointment, the patient tests the provisionals for 1 week. Follow-up adjustments can be made at the 1-week mark when the patient returns to the office for final record-taking.
The final records consist of a facebow that is taken along with an impression of the approved provisionals, a mandibular impression, a bite registration, and a full photographic series. The cross-mounting procedures are completed as previously mentioned. The process entails mounting the facebow cast of the approved provisionals, followed by mounting the mandibular opposing cast to the approved provisionals (Figure 15), and then mounting the maxillary master die cast to the mandibular opposing cast (Figure 16). The facial reduction matrix is then created along with a custom incisal guide table (Figure 17), which allows the ceramist to visualize the 3D functional esthetic matrix of the patient (Figure 18). It is paramount that the ceramist works within the confines of this functional esthetic matrix in order to replicate the esthetic, phonetic, and functional determinants verified in the provisionalization process. This is the key to producing predictable final restorations (Figure 19 and Figure 20).
Conclusion
Verification of provisional restorations is vital to attaining predictable esthetic results. Using meticulous testing and systematic refinements the clinician is able to communicate invaluable information to the ceramist with regard to the patient's lip dynamics and functional determinants. Although provisionals are considered interim restorations, their importance should not be diminished because their effects are not just "temporary" but impact the long-lasting functional and esthetic success of the final restorations.
Acknowledgment
The author thanks Shoji Suruga, CDT, AAACD, of Bay View Dental Laboratory, Chesapeake, Virginia, for his artistic work on the porcelain restorations in this case.
About the Author
Zachary S. Sisler, DDS, AAACD
Associate Faculty Member, The Dawson Academy, St. Petersburg, Florida;
Private Practice, Shippensburg, Pennsylvania
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Kois JC. New challenges in treatment planning - Part 2: incorporating the fundamentals of patient risk management. J Cosmetic Dentistry. 2011;27(1):110-123.
2. Hess L. The concept of the complete examination. Inside Dentistry. 2015;11(5):82-88.
3. Cobb AC. Complete treatment planning: meeting patients' needs. Inside Dentistry. 2015;11(8):66-70.
4. Dudney TE. Using diagnostic wax-ups and preparation guides to facilitate accurate and esthetic diastema closure and functional bite alteration. Inside Dentistry. 2008;4(7).
5. Saeidi Pour R, Pinheiro Dias Engler ML, Edelhoff D, et al. A patient-calibrated individual wax-up as an essential tool for planning and creating a patient-oriented treatment concept for pathological tooth wear. Int J Esthet Dent. 2018;13(4):476-492.
6. Dawson P. Functional smile design. In: Functional Occlusion: From TMJ to Smile Design. St. Louis, MO: Mosby; 2007:149-158.
7. Dawson P. Anterior guidance and its relationship to smile design. In: Functional Occlusion: From TMJ to Smile Design. St. Louis, MO: Mosby; 2007:159-175.
8. Spear FM, Cooney JP. Restorative interrelationships. In: Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds. Carranza's Clinical Periodontology. St. Louis, MO: Saunders Elsevier: 2006:1050-1069.
9. Vig RG, Brundo GC. The kinetics of anterior tooth display. J Prosthet Dent. 1978;39(5):502-504.
10. Passia N, Blatz M, Strub JR. Is the smile line a valid parameter for esthetic evaluation? A systematic literature review. Eur J Esthet Dent. 2011;6(3):314-327.
11. Fradeani M. Evaluation of dentolabial parameters as part of a comprehensive esthetic analysis. Eur J Esthet Dent. 2006;1(1):62-69.
12. Williamson EH, Lundquist DO. Anterior guidance: its effects on electromyographic activity of the temporal and masseter muscles. J Prosthet Dent. 1983;49(6):816-823.
13. Okano N, Baba K, Akishige S, Ohyama T. The influence of altered occlusal guidance on condylar displacement. J Oral Rehabil. 2002;29(11):1091-1098.
14. Darveniza M. Full occlusal protection-theory and practice of occlusal therapy. Aust Dent J. 2001;46(2):70-79.
15. Okeson JP. Criteria for optimal functional occlusion. In: Okeson JP, ed. Management of Temporomandibular Disorders and Occlusion. 5th ed. St. Louis, MO: Mosby; 2003:109-126.
16. Witt M, Flores-Mir C. Laypeople's preferences regarding frontal dentofacial esthetics: tooth-related factors. J Am Dent Assoc. 2011;142(6):635-645.
17. Kokich VO Jr, Kiyak HA, Shapiro PA. Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent. 1999;11(6):311-324.
18. Cranham J, Finlay S. Timeless principles in esthetic dentistry. J Cosmetic Dentistry. 2012;28:64-73.
19. Rosenstiel S, Land M, Fujimoto J. Interim fixed restorations. In: Contemporary Fixed Prosthodontics. 4th ed. St. Louis, MO: Mosby; 2006:466-504.
20. Sesemann M. Diagnostic full-coverage provisionals for accurately communicating esthetic and functional. Functional Esthetic Restorative Dentistry.2008;2(2):8-14.