You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
More than ever, dental patients search the Internet for treatment solutions for their compromised remaining teeth and edentulous spaces. What they often find is a suffocating amount of information that promises remarkable results no matter what their predicament. Nonetheless, dentists are challenged to correctly diagnose their patients' problems and provide realistic solutions that are carefully determined and that reflect the expectations of both patient and clinician. Treatment requires attention to a diversity of details that clinicians can compile and evaluate with extraordinary accuracy by assimilating data from software programs using a digital platform that can produce dynamic results that are dramatically precise or, in the least, help explain to the patient why certain outcomes are unrealistic. While the scientific evidence to support complete digital workflows in implant dentistry is limited, the efforts and progress of industry foster the increasing interest of practitioners to invest in these types of protocols and implement them into clinical practice.1
The digital components are collectively referred to as the "digital workflow" and include surgical blueprints derived from restoratively designed plans, which in turn can be tailored to clearly define procedures, such as orthodontic and orthognathic intervention, that are necessary to achieve the desired restorative result. Perhaps the greatest strength of the digital workflow lies in the ability for surgical clinicians, restoring dentists, other specialists, and technicians to collaborate in the treatment planning process to heighten treatment outcomes. The result is a truly prosthetically driven surgical procedure that produces the optimal functional and esthetic restorative design.2
Presently, the dental profession is divided between the perceived benefits of the digital process and the financial and time implications. The authors suggest that much of this divide has to do with misunderstanding of how the process or parts can fit together (Figure 1). The intent of this article is to clarify the flow of this process using examples and review additional software applications that can be implemented to strengthen the output of the workflow. It is important to stress that these applications are constantly being introduced to enhance the functional features of digitalized dentistry and help motivate practitioners. This type of process may very well become mainstream once the dental profession more fully understands the potential of these computer-directed methods.
Similar computer-aided workflows have been established in craniomaxillofacial reconstructive surgery, where the typical steps involve diagnosis, planning/simulation of surgery procedures, and validation. The diagnostic phase uses 3-dimensional (3D) imaging such as computed tomography (CT) scans. Virtual models are created according to the intended or planned outcome using planning software programs, which can subsequently be used with the virtual reconstruction to manufacture patient-specific facial implants, thereby overcoming the limitations exercised by significant ridge form and volume deficiencies in cases of craniomaxillofacial trauma, tumor, and reconstructive surgery.3,4 So, too, has orthognathic surgery planning evolved considerably from the use of ordinary 2-dimensional (2D) imaging to computer-based planning. Cephalometric and facial analysis and casts of dental arches mounted on mechanical articulators for surgical splint fabrication are being replaced by designs that are transferred from virtual planning to the actual surgical procedure, using prototyped surgical splints and cutting guides derived from computer-based design. In every case, 3D virtual planning outperforms 2D planning in optimizing treatment predictability and esthetics when correcting issues such as midline deviations, ramus asymmetry, occlusal plane canting, and chin position.5
The authors' interpretation of and a step-by-step approach to the digital workflow for dentistry, referred to as "digital touchpoints," are outlined in the following sections.
Digital Touchpoints 1 and 2: STL Files (IOS) and DICOM Files (CBCT)
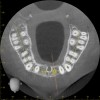
For dental implant-based treatment, the planning phase begins with collection of basic data sets; this is digital touchpoint 1. It includes: (1) a cone-beam CT (CBCT) to view edentulous areas or failing tooth structure, bone, and anatomic landmarks under the soft tissue (Figure 2 through Figure 4); and (2) an intraoral optical scan (IOS) or a scanned model or impression to record the soft tissue and tooth anatomy (Figure 5). The superimposition of the digital imaging and communications in medicine (DICOM) files from the CBCT and the standard tessellation language (STL) files from the IOS allows visualization of how bone, dental structures, and soft tissues relate. Both digital data points are key to implant selection and determining the surrounding bone-grafting needs. An initial treatment plan includes determining the desired implant manufacturer/implant design, size, and positions; these decisions remain the responsibility of the clinician (restoring and surgical team members) and not the technician or planning team.
To reduce the time and costs associated with the steps required to use these digital data sets, DICOM and STL files may be outsourced for off-site data management and virtual restoration design; this is referred to as digital touchpoint 2. This may be carried out by clinicians involved in the case if they are so inclined, or by a planning team, whether it be a laboratory or other service center. Using a trained planning team can significantly accelerate the preparation process.
To fully understand how the digital process benefits any form of treatment planning (eg, teeth or implants or a combination), it is helpful to work with systems that can handle precise data that includes the face and smile as a framework. Procedure-specific methods, such as "smiling scan techniques," have been described that bring into focus the importance of facially planned and driven surgical and prosthetic steps.6,7 For this article, the authors use a planning system (Face Hunter scanner, Zirkonzahn, zirkonzahn.com) that allows the creation of a "virtual patient" by creating a photorealistic 3D digitalized face that serves as a working basis for the production of dental prostheses. This program and tooling are primarily utilized in laboratories, but these types of planning and milling/printing systems may become more prevalent in high-volume dental clinics. Use of this type of digital platform versus conventional prosthodontic methods in the planning and execution of treatment strengthens the esthetic and functional value of the intraoral data from digital touchpoint 1. The steps in the aforementioned planning system protocol include:
1. The capture of the patient's face, which is reformatted into a photorealistic 3D digitalized rendering using a series of cameras that make up the scanning system. This screen capture is used as the working foundation, which the authors call "face-in" design of treatment, supplementing the CBCT and IOS scanning data (Figure 6).
2. Standardized reference planes, which are created using facial landmarks and thus establish an idealized dental midline, occlusal plane, and curve of Monson, all of which are tied into the frame of the face at rest and in dynamic movements. These reference planes, along with virtual articulation, basically eliminate the need to use conventional facebows or transfer bows and conventional articulators (Figure 7).
3. The face scan coupled with an optical scan or scanned impressions/casts, which are used to mock-up the desired restorative result by using a modeling software. This allows for creation of digital wax-ups and restoration designs, comparison of pre/post-restoration contours and positions using transparent overlays (permitting viewing of the anticipated changes relative to baseline through the use of 3D superimposition), and anticipation of endodontic procedures that may be required due to the expected reduction of tooth structure needed to achieve the desired outcome without altering tooth positions (Figure 8 and Figure 9). In turn, multiple try-ins and adjustments resulting from insufficient information are either entirely avoided or minimized. This detailed information is almost impossible to visualize using stone models. Also, it reduces working time in the design phase and "virtually" archives all proposals.
4. The entire set-up allows a preview of hard/soft-tissue augmentation or reduction requirements based on virtual and desired implant positions. It is here that decisions are made as to whether the plan can be achieved, or if pre-prosthetic steps such as orthodontic and orthognathic procedures are necessary to avoid open bites or reverse smiles. The benefit in virtually previewing the lip position relative to the transition zone (tissue-prosthesis interface) may especially be appreciated in all-on-4 or -6 full-arch implant restorations. Bone reduction guides or planned implant positions relative to a "virtually" reduced ridge to allow apical correction of the tissue-prosthesis interface are critical to the esthetic success of a prosthesis. "Face-in" planning literally eliminates this challenge (Figure 10 and Figure 11).
Digital Touchpoint 3: Initial Presentation/Digital Wax-ups and Inter-Practice Digital Communication
All involved clinicians and technicians, including the restoring dentist, laboratory technician, surgical members, orthodontist, and any other clinicians required in the treatment, can discuss every step of the plan via digital sharing platforms for online meetings. This virtual collaboration enables clear communication as to the direction of the case, and, most importantly, whether the desired outcome is achievable and affordable before any work is carried out. These digital steps also can enhance the level of discussion between practitioner and patient, enabling the avoidance of unrealistic expectations and possibly aiding patient motivation.
(To view a short video example of how digital collaboration can enhance a practitioner/patient discussion, scan the QR code on p.419 or go to compendiumlive.com/go/cced1880.)
Not having to physically meet to discuss and plan cases can allow clinicians to work with geographically distant contributors, whether a dentist, surgical team member, or technician. In the authors' experience, this format has strengthened the team approach by allowing more frequent communication, thereby enhancing case review, plan development and refinement, and production of required surgical and restoration components. With the capacity to collaborate in the virtual environment, global clinicians and technicians may be more readily included in the case, bringing the best available experts together to manage the task.
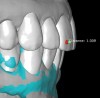
The direct impact of this collaborative approach is that the team is better able to anticipate surgical challenges and preplanned solutions. For instance, whether bone grafting relative to implant placement will be required and how to achieve these augmentation goals can be anticipated (Figure 12 and Figure 13). Planning implant position from the restoration down may allow positioning implants for screw retention or angled-screw technology, thus minimizing the need for cemented restorations. This type of preview may influence the choice of implant for the desired restoration, as not all systems currently offer corrective screw technologies without migrating into the use of non-authentic components.
Digital Touchpoint 4: Surgical Guide Fabrication (and Transitional Restoration Components)
From the data and collaboration in steps 1 through 3, surgical guides can be fabricated for static surgery, and when indicated, prosthetic components, such as custom healing abutments, provisional crowns, or fixed partial dentures, can be produced for delivery at the time of surgery to guide soft-tissue healing. The static approach, better known as computer-guided surgery, refers to the use of tissue-tooth or soft- and hard-tissue-supported surgical templates. In essence, the virtual implant position planned from the CBCT, IOS, and face-in data sets is reproduced. The guide is produced with master cylinders (portals) through which the osteotomy preparation drills are introduced, and in full-guidance cases, the delivery of the implant is carried out (Figure 14 and Figure 15). Dynamic guided surgery or computer "navigation" traces the virtual implant position directly from CBCT data and employs motion tracking or real-time tracking technology to prepare the implant osteotomy. This makes it possible to determine the actual position of the surgical drill on the reconstructed 3D image provided by the CBCT. The surgeon is guided to the position that was planned preoperatively while he or she performs the surgical procedure. Examples of dynamic navigation systems are Navident (ClaroNav, claronav.com), X-Guide Dynamic 3D Navigation (X-Nav, x-navtech.com), Image Guided Implant (IGI) Dentistry System (Image Navigation, image-navigation.com), Inliant® (Navigate Surgical, navigatesurgical.com), and YOMI®, a robotic haptic guidance system (Neocis, neocis.com).
Printing or milling of surgical guidance devices and prosthetic components needed at surgery can be performed in the clinic or laboratory. There are advantages and disadvantages to both approaches, and views on this may vary among clinicians. Those who are well-versed in computer-based technologies are more likely to plan and produce both surgical and restorative components in practice, while those who are not as comfortable in the handling of software to plan, design, and produce components for surgery and restoration will probably be more inclined to outsource. For clinicians who typically maintain a rigidly structured daily practice, taking the time required for in-office guide and restoration design/production may be unrealistic, and therefore outsourcing may be preferred. The cost of software and hardware needed to plan and produce the required components will influence this step. Co-sharing technology with laboratories can result in less case-by-case expense to the clinician, which, in turn, can be factored into treatment fees. Benefits realized by technicians from input from numerous clinicians contributing in the various touchpoints include improvement in plan accuracy and pace, which coupled with the patient's approval, tends to minimize revisions and remakes, enabling maximum profit to be derived through the production of the various provisional and definitive restorative components. Additional work and expenses are justified by improved visualization, information, and documentation.
Digital Touchpoint 5: Surgical Treatment Phase (and Optional Delivery of Prefabricated Restorative Components)
Guided surgery, whether it be static or dynamic navigation, improves accuracy in comparison to free-handed implant placement procedures.8,9Static surgery may involve the use of laboratory-processed stereolithographic guides to both prepare the osteotomies and deliver implants.10 Other than in regions with limited access, these accurate guidance templates can be considered for use in any scenario. Dynamic navigation offers advantages in these types of situations. Although linear and angular deviations between planned and executed implant positions are possible and probable, operator experience and use of appropriate hardware can minimize these deviations.11,12
The introduction of prefabricated provisional or transmucosal components enables clinicians to better control and realize the benefits of tissue guidance, especially in immediate implant placement protocols (Figure 16 through Figure 19).13 While immediate provisionalization or tissue guidance is not a new concept, the ability to preplan and fabricate these appliances before surgery is an important evolution tied to the digital workflow. Historically, restorative components such as custom healing abutments, provisional crowns, or fixed partial dentures were either made chairside "intrasurgically" or impressions were taken for delayed delivery. These conventional approaches both increase chairtime and potentially introduce errors or imprecision that are often inherent in these analog steps when done chairside. The impacts of precise production and ideal design of transmucosal parts cannot be overstated when considering the biologic responses of soft and hard tissues to these components. Peri-implant tissue stability is impacted by poor implant positioning and implant collar design/positioning relative to the osseous crest, but is also linked to the design of transmucosal restorative components (Figure 20 and Figure 21). A recent histologic and micro-CT analysis demonstrated that the configuration of transmucosal components influence the orientation of peri-implant tissues on implant designs with a horizontal offset.14
Digital Touchpoint 6: Conventional Impressioning vs IOS/Scan Bodies
A well-fitting prosthesis cannot be fabricated if the implant position is recorded inaccurately, and the resultant misfit can lead to biomechanical complications such as component breakage, screw loosening, and bone loss as a result of increasing stress within the prosthesis or at the interface of the implant and bone.15 A digitally focused practice may at times still need to use conventional impressioning, but only sparingly. Examples of such situations may include treatment of a fully edentulous patient where anatomic landmarks are limited, where accurate functional recording of the vestibular areas is needed in complete denture fabrication, and where reflective restorative materials or access preclude effective scanning. If the final prosthesis for the fully edentulous patient is a hybrid all-on-4 design, then accurate registering of the vestibular areas is unnecessary since the denture flanges will be cut back and reshaped in the final restoration.
Impressioning single implant units or short edentulous spans using scan flags or bodies is as reliable as conventional impressioning in terms of accuracy.16,17 "Precision" essentially is the evaluation of how close several measurements of the same object are, and "trueness" relates to the difference in measurement of a given object compared to the actual dimensions of that object. Scan bodies record the 3D position of the implant(s). When scanning a greater number of scan flags in larger edentulous situations, there are fewer reliable reference points between flags in comparison to partially dentate situations. Consequently, these areas can present as poorly "stitched" together and lead to inaccuracies. In a recent study, efforts to place markings or objects between implants or connect them did not improve the stitching process, resulting in distance and angular deviations.18 Scanning techniques for the dentate or partially edentulous cases (eg, occlusal, buccal, then palatal or occlusal, lingual, then buccal) influence accuracy, however there are no recommended pathways for fully edentulous cases.
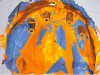
Scan flags themselves can contribute to inaccuracies associated with their shape or design. For example, their depth in the tissue affects how much of the flag remains visible; the torque applied to insert them is a factor; the material of their mating surface to the implant (eg, distortion of polyetheretherketone base material compared to titanium) is a consideration; and the amount of handling and number of uses the scan flag has experienced is a factor. The authors also have found through evaluations that use of multi-unit abutment scan flags, which thus far has been sparsely studied, resulted in significant deviations from conventional impressions comparing the same cases using heat-scan analysis (Figure 22 and Figure 23). Presently, in completely edentulous situations involving the scanning of four or more implants, obtaining digital impressions from a specific IOS remains a challenge.
Digital Touchpoints 7 Through 9: Printing or Milling Fixed or Removable Definitive Prosthetic Devices, Approval, and Insertion
Currently, printing and milling procedures are generally performed by laboratories, although some progressive clinicians are stepping into this arena as well. Many laboratories basically are fully digitized, with reduced analog steps that may be limited to site-selective and judicious addition of feldspathic porcelain. The last vestige of the analog realm that has yet to be overtaken is the cementation step, not only for the restoration of teeth but also in implant treatment where screw retention may be impossible.
Accuracy in prosthesis fit is essential in implant dentistry. Unlike teeth, implants cannot adapt to ill-fitting prostheses, which can result in complications such as undue stress on implant components. While cementation of a prosthesis allows for some adaptability, screw-retained restorations demand passivity of fit for restorative material and component success, more so than for implant success. Although the accuracy of CAD/CAM technology is superior to conventional casting methods, it nonetheless is dependent on the quality of the information "fed" into the system. Digital impressioning is assumed to be a method capable of reducing inaccuracies associated with impressions and material handling, although the literature on this subject is still undeveloped. Many factors have been noted to influence the trueness and precision of scan results when comparing digitally generated models to reference models in in vitro studies.19 In vitro studies evaluating accuracy of scanning using current scanner models showed equal or superior outcomes to conventional impression techniques. Few in vivo studies are available for reference. Linear variation ranged from 6 µm to 337 µm with angle deviations of as little as 0.07 degrees to 0.3 degrees. Some of the factors assessed that affect outcomes included: operator experience and scan method/strategy, type of scanner used, scan body design, visibility of the scan body, bone-level versus tissue-level implant scanning, distances between scan bodies, divergence between two implants, length of area and number of implants being scanned, and reference point availability. When viewed from a global perspective, this one aspect of the digital workflow has the potential to significantly increase the accuracy (precision and trueness) of the outcome or be a point of significant error introduction.
Unfortunately, randomized clinical trials for fully digitalized workflows for either teeth or implant-supported fixed restorations are scarce. Presently, a strong offering of rapid prototyping procedures exists, including CAD/CAM-produced full-contour or monolithic crowns (Figure 24) and milled frameworks combined with CAD/CAM veneering superstructures. A true digital workflow for crown-and-bridge is not mainstage at present, and barely exists in an analog-digital blend, but the authors believe this will change soon. The layering of porcelain is cumbersome and operator dependent with many working parts and lacks the consistent precision found with today's computerized technology. Joda described a threefold improvement in time efficiency, and either no or minor adjustments of implant-supported crowns, using a digital workflow (intraoral scanning and CAD/CAM technology) in comparison to conventional methods.20 Laboratory time savings have been most impacted by the digital workflow (average 54.5 minutes of production time versus 132.5 minutes), along with a 30% overall treatment cost reduction.21
With today's monolithic, stain-only occlusal surfaces, any modification can contribute to a poor esthetic result as the coloration is removed down to an underlying monotone white appearance. Designs derived from the digital wax-up can be verified and approved in a virtual meeting, much like that of the implant and surgical guide strategy steps. Once completed, the restorations are either cemented or screw-retained according to the manufacturer's instructions.
Conclusion
The digital workflow has long penetrated dental laboratories but until recently has only minimally impacted clinical practices. Digitally based technologies and thinking is beginning to alter the way clinicians conduct their surgical and restorative work and, most importantly, how they plan and communicate with patients and technicians. As technology evolves and scientific support strengthens, the authors anticipate that tomorrow's practitioners will significantly reduce their use of analog procedures, recognizing the clear advantages, efficiency, and accuracy of digital protocols, from documentation and planning through surgical and restorative treatment.
Acknowledgment
The authors acknowledge Neil Appelbaum, CDT, and Gerrit Van Schalkwyk, CDT, of Protec Dental Laboratories Ltd., Vancouver, Canada, and Klaas Van Der Walt, RDT, and Nico Pienaar, RDT, of Pro-Esthetics Dental Laboratory, Ltd., North Vancouver, Canada, for their contributions to this article.
About the Authors
Sonia S. Leziy, DDS, Dipl. Perio
Certified Specialist in Periodontics/Implant Dentistry, University of British Columbia, Vancouver, Canada; Private Practice, North Vancouver, British Columbia, Canada; Fellow, The Royal College of Dentists of Canada (FRCD[C]) Periodontist
Brahm A. Miller, DDS, Dipl. Pros
Certified Specialist in Prosthodontics/Implant Dentistry, University of British Columbia, Vancouver, Canada; Private Practice, North Vancouver, British Columbia, Canada; Fellow, The Royal College of Dentists of Canada (FRCD[C]) Prosthodontist
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Joda T, Zarone F, Ferrari M. The complete digital workflow in fixed prosthodontics: a systematic review. BMC Oral Health. 2017;17(1):124.
2. Guichet DL. Digital workflows in the management of the esthetically discriminating patient. Dent Clin North Am. 2019;63(2):331-344.
3. Gellrich NC, Rahlf B, Zimmerer R, et al. A new concept for implant-borne dental rehabilitation; how to overcome the biological weak-spot of conventional dental implants? Head Face Med. 2017;13(1):17.
4. Gellrich NC, Zimmerer RM, Spalthoff S, et al. A customised digitally engineered solution for fixed dental rehabilitation in severe bone deficiency: a new innovative line extension in implant dentistry. J Craniomaxillofac Surg. 2017;45(10):1632-1638.
5. Cintra O, Grybauskas S, Vogel CJ, et al. Digital platform for planning facial asymmetry orthodontic-surgical treatment preparation. Dental Press J Orthod. 2018;23(3):80-93.
6. Pozzi A, Arcuri L, Moy PK. The smiling scan technique: facially driven guided surgery and prosthetics. J Prosthodont Res. 2018;62(4):514-517.
7. Joda T, Bragger U, Gallucci G. Systematic literature review of digital three-dimensional superimposition techniques to create virtual dental patients. Int J Oral Maxillofac Implants. 2015;30(2):330-337.
8. Scherer U, Stoetzer M, Ruecker M, et al. Template-guided vs. non-guided drilling in site preparation of dental implants. Clin Oral Investig. 2015;19(6):1339-1346.
9. Choi W, Nguyen BC, Doan A, et al. Freehand versus guided surgery: factors influencing accuracy of dental implant placement. Implant Dent. 2017;26(4):500-509.
10. Skjerven H, Riis UH, Herlofsson BB, Ellingsen JE. In vivo accuracy of implant placement using a full digital planning modality and stereolithographic guides. Int J Oral Maxillofac Implants. 2019;34(1):124-132.
11. Jorba-Garcia A, Figueiredo R, González-Barnadas A, et al. Accuracy and the role of experience in dynamic computer guided dental implant surgery: an in-vitro study. Med Oral Patol Oral Cir Bucal. 2019;24(1):
e76-e83.
12. Block MS, Emery RW, Cullum DR, Sheikh A. Implant placement is more accurate using dynamic navigation. J Oral Maxillofac Surg.2017;
75(7):1377-1386.
13. Crespi R, Capparé P, Crespi G, et al. Tissue remodeling in immediate versus delayed prosthetic restoration in fresh socket implants in the esthetic zone: four-year follow-up. Int J Periodontics Restorative Dent. 2018;38(suppl):s97-s103.
14. Souza AB, Alshihri A, Kammerer PW, et al. Histological and micro-CT analysis of peri-implant soft and hard tissue healing on implants with different healing abutment configurations. Clin Oral Implants Res. 2018;29(10):1007-1015.
15. Örtorp A, Jemt T. CNC-milled titanium frameworks supported by implants in the edentulous jaw: a 10-year comparative clinical study. Clin Implant Dent Relat Res. 2012;14(1):88-99.
16. Marghalani A, Weber HP, Finkelman M, et al. Digital versus conventional implant impressions for partially edentulous arches: an evaluation of accuracy. J Prosthet Dent. 2018;119(4):574-579.
17. Ahilholm P, Sipilä K, Vallittu P, et al. Digital versus conventional impressions in fixed prosthodontics: a review. J Prosthodont. 2018;27(1):35-41.
18. Mizimoto RM. The accuracy of different digital impression techniques and scan bodies for complete-arch implant-supported reconstructions [thesis]. Columbus, Ohio; The Ohio State University; 2018.
19. Rutkūnas V, Gečiauskaitė A, Jegelevičius D, Vaitekūnas M. Accuracy of digital implant impressions with intraoral scanners. A systematic review. Eur J Oral Implantol. 2018;10 suppl 1:101-120.
20. Joda T, Katsoulis J, Bragger U. Clinical fitting and adjustment time for implant-supported crowns comparing digital and conventional workflows. Clin Implant Dent Relat Res. 2016;18(5):946-954.
21. Joda T, Bragger U. Time-efficiency analysis of the treatment with monolithic implant crowns in a digital workflow: a randomized controlled trial. Clin Oral Implants Res. 2016;27(11):1401-1406.