You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Combination Syndrome (CS) is a dental condition commonly seen in patients with a completely edentulous maxilla combined with a partially edentulous mandible, typically with well-preserved anterior teeth.1 At times this syndrome includes a severe anterior maxillary resorption in concert with hypertrophic and atrophic changes in varying quadrants of the maxilla and the mandible. This is a challenging condition to restore due to the aforementioned factors.2
At times, depending on the severity of the resorption and associated "flabby tissue," a static impression or selective pressure impression can be chosen. Unfortunately these types of cases are very difficult and challenging in terms of patient acceptance and compliance wearing a mandibular removable partial denture.
If caught early enough, it is best to ensure patient compliance when it comes to cessation of additional trauma to the premaxilla. For example, if the patient continues to wear the maxillary denture but refuses to wear the mandibular removable partial denture, over a relatively short amount of time additional trauma to the premaxilla precipitates greater bone resorption and added difficulties for future treatment.
It is imperative that this cycle of CS be broken, especially if the patient is noncompliant.
A Novel Approach to CS
Even contemporary dentistry has not been able to solve this cycle of resorption if the patient is noncompliant. Conventional removable partial denture (RPD) constructions do not always satisfy patient comfort or esthetics in this situation. While the dental industry clamors to launch new products into the RPD arena in efforts to capture this large, "untouched" market share, a little technical ingenuity and an outside-the-box approach were needed, coupled with traditional processes such as casting and hand milling.3
In this article the author demonstrates a creative way to treat and design a mandibular removable partial that satisfies esthetic and practical demands by utilizing two posterior implants, a lingual plate, two 0° telescopic abutments, and assisted tissue support.
The Case
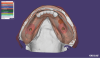
The patient initially presented with classic CS features: completely edentulous maxilla and missing mandibular posterior teeth. Two implants (ASTRA TECH Implant System EV, Dentsply Sirona; dentsplysirona.com) were placed in the mandible, and, after osseointegration was complete, two healing abutments were placed (Figure 1 through Figure 4). When the case was ready to be restored, a mandibular implant-level impression was taken using engaging impression posts and two viscosities of vinyl polysiloxane (VPS) materials (Figure 5). A maxillary edentulous impression was taken using a two-part alginate system. The casts were poured using a resin-reinforced type IV die stone (FUJIROCK IMP, GC America Inc.; gcamerica.com) that was vacuum mixed.
Once the master casts were fully set, they were trimmed, and base plates and wax rims were made (Gebdi Wax Bite Rims Vanilla Aroma, Gebdi Dental Products; gebdi-dental.de). At the clinical appointment, the wax rims were trimmed by the dentist and marked at the midline and canine positions and at the high smile line. A centric record was taken (Figure 6). As is typical in CS cases, the vertical dimension had collapsed somewhat and needed to be restored. This was done in the clinic. Additionally, the case was a skeletal Class II, and the setup was made to fit this skeletal class instead of attempting to alter the classification by placing the maxillary teeth in unnaturally palatal positions.
The first setup in wax closely met both clinical and patient expectations in terms of restored vertical dimension, esthetics, and phonetics (Figure 7). At this point, the mandibular implant telescopes were designed by scanning the implant model with scan bodies, the wax try-in as a pre-op scan, and the silicone matrix with teeth removed from the wax as an antagonist scan in order to register the basal surfaces of the teeth and incorporate them into the design of the primary telescopes (Figure 8 through Figure 12).
Once the primary telescopic titanium abutments were milled, they were then transferred to a milling model using a spider jig (Figure 13). This is especially important when hand milling any metal telescopes, as the heat and pressure generated by the hand milling process could loosen the analogs in the master model. Once hand milling and polishing were realized (Figure 14), temporary copings made of pattern resin (PATTERN RESIN LS, GC America Inc.) were made and seated completely on the primary titanium telescopic abutments.
Tertiary Structure/RPD Framework
At this point, the case was ready for the tertiary/RPD framework. A lingual plate was part of the plan in order to give the case as much support as possible. Additionally "baskets" were made over the top of the pattern resin temporary secondary copings so that they could be picked up into the framework intraorally to verify the exact implant positions from mouth to model (Figure 15).
At the next clinical appointment, the abutments were seated, temporary pattern resin copings were completely seated, and the framework was inserted to ensure the tissue rests and lingual plate components were seating passively and that there was a small space between the baskets and the temporary pattern resin copings. The resin copings were then luted to the framework in the mouth using pattern resin and allowed to set for 15 minutes. The framework was then removed, and the assembly was checked on the master model carefully to see if it seated passively. In the case that it did not seat passively, the model would be corrected to reflect the exact implant positions on the model. In this case, the assembly did fit passively, and it was possible to go directly to the electroforming phase.
Electroforming
The primary telescopic abutments were airbrushed with silver conductive lacquer (Figure 16) and connected to electric leads (Figure 17) in the electroforming machine (GAMMAT Easy, Gramm Technology; grammusa.com). The abutments were then put into the electroformer with the gold solution ECOLYT SG100 (Gramm Technology) and activator liquid. The amount of gold solution was calculated and entered into the unit, and the program was started. The process typically runs about 6 hours and forms a uniform gold coping directly to the primary telescopic abutment (Figure 18). The copings were removed from the primary abutments and placed into a 40% nitric acid solution in an ultrasonic unit for 15 to 20 minutes in order to remove all traces of the silver conductive lacquer (Figure 19).
The copings were then air abraded at 2 bar pressure with aluminum oxide and prepared with a metal primer (GC METALPRIMER II, GC America Inc.). The tertiary/RPD framework baskets were also air abraded and metal primer was applied.
Cementation
The tertiary/RPD framework was then cemented to the prepared gold copings using an adhesive resin cement (G-CEM, GC America Inc.). This step could also be performed intraorally in order to achieve 100% passivity in the event that the model is not completely accurate. In this case the cementation was done on the master verified cast. The tertiary framework was then opaqued, and the posterior denture teeth were reattached to the framework on the master verified cast using the previously made silicone matrix. The case was returned to the dentist for a final wax try-in with all hardware assembled. Following this full hardware wax try-in (Figure 20 and Figure 21), the case was ready for final processing in acrylic.
Processing
It is preferable that the processing is performed on a processing duplicate model. The screw accesses of the telescopic abutments were blocked in wax, and the master verified cast was duplicated using duplicating silicone. The negatives of the telescopes were recreated using pattern resin with small retentions for pouring of the processing duplicate model in buff stone.
Once the processing duplicate was made, the wax prosthesis could be seated fully on the processing duplicate model and sealed. The wax-up was invested for processing and the wax portion was covered with a two-part silicone putty. The second half was invested, and, after wax removal in the boil-out was completed, the framework could be removed. The internal aspects of the gold telescopes were partially filled with a light bodied VPS and quickly reseated on the duplicate model, and any excess VPS was removed. The VPS protects all of the internal surfaces of the gold copings.
A separating agent (COE-SEP, GC America Inc.) was painted onto the models and the negative impression of the gingiva was prepared for gingival characterized acrylics using NATURE-CRYL® (GC America Inc.) acrylic shades. Fibers were removed from shades #34 and #35, and modifiers were added to the monomer liquid to intensify the lighter #34 shade and darken the #35 shade to mimic more vascular colors. These colors were loaded into syringes for accurate placement into the negative mold of the gingiva.
It is important to note that when working in the negative space, all build-up is the reverse of positive build-up. The lighter modified #34 shade was placed first to mimic the somewhat blanched shading characteristic around the cervical of the teeth. This color was placed and feathered out with a kolinsky brush wetted with monomer. The darker modified #35 shade was placed at the periphery and feathered toward the dentition with the same kolinsky brush slightly wet with monomer. These two colors provided a very nice, natural appearance when blended well using this technique, and appeared in the finished prosthesis as three or four colors due to the variations of thickness and blending of the two (Figure 22).
A piece of the base acrylic-in this case shade #35-was mixed and a strip was placed over the characterization just prior to acrylic injection. This prevents shifting and/or movement of the carefully placed characterized acrylics.
Divesting
Post-processing divesting was performed carefully with a pneumatic air chisel, and the pattern resin telescope analogs were removed with the light body VPS, revealing a clean interior surface of the gold copings. The acrylic was finished minimally with carbide burs, polishing instruments, and finally with pumice substitute and high shine polish (DVA Acryl-Marvel, Dental Ventures of America, Inc.; dentalventures.com).
The day of insertion the telescopic abutments were placed and torqued to 30 NcM (Figure 23). The maxillary denture was placed, and the mandibular telescopic partial was carefully placed and seated (Figure 24). The patient was asked to remove and insert a few times in order to ensure that there were no problems seating and removing after leaving the dental office. The access holes were covered first with Teflon tape placed deep into the screw channel in order to protect the abutment screw and finally covered with flowable composite in a concave way, sealing the access holes.
Conclusion
Combination Syndrome cases can be difficult to treat. There are clear benefits to catching these cases early on, prior to excessive resorption of bone in the area of the premaxilla. By providing the patient with a solution that required no clasping or tooth preparation, the chances that the patient would be compliant in terms of actually wearing the partial mandibular prosthesis was greatly increased, thus increasing the ability to effectively treat these cases long term.
About the Authors
Arian Deutsch, CDT
Owner
Deutsch Dental Arts
Surprise, AZ
Rahul G. Kode, DDS, FAGD
Desert View Dental
Phoenix, AZ
References
1. The glossary of prosthodontic terms. J Prosthet Dent. 2005;94(1):10-92.
2. Kelly E. Changes caused by a mandibular removable partial denture opposing a maxillary complete denture. J Prosthet Dent. 1972;27(2):140-150
3. Attard NJ, Zarb GA. Implant prosthodontic management of partially edentulous patients missing posterior teeth: the Toronto experience. J Prosthet Dent. 2003;89(4):352-359.