You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Permanent first molars with severe enamel hypoplasia/hypocalcification defects, with or without associated dental caries infection, pose difficult challenges for the clinician. The ultimate treatment for such teeth, at the appropriate time, is full (or onlay) coronal coverage with precision cast metallic crowns, ceramic crowns, or ceramic fused to metal crowns. Such long-term repair cannot be achieved until the late teen or early adult years, until sufficient eruption and maturation of the affected teeth occurs. The chief challenge for the clinician is how to restore the affected tooth for an interim period, from multiple months of caries control to as long as 10 to 15 years.
Treatment decisions are influenced by the following:
• eruption status of the tooth (How much soft tissue is covering the occlusal and axial surfaces, limiting restorative access?)
• patient discomfort due to tooth sensitivity
• severity of caries involvement
• considerations about durability and longevity of whatever restorative method is used
• severity and extent of hypoplasia and hypocalcification (How many cusps are salvageable? Is there sufficient enamel remaining for adhesive bonding of suitable restorative materials, or would the best restoration be a custom adapted stainless steel crown?)1,2
• judicious repair to conserve tooth structure and not compromise eventual long-term precision ceramic/metallic crown preparation in the late teen or adult years
• which materials to use to assure no postoperative tooth sensitivity for the patient
Restoration of malformed/carious permanent molars has been reported on previously by this author.3,4 Since the 2014 report, several new materials have been introduced that influence success of these types of molar restorations. Chief concerns are physical characteristics of the restorative material, pulp protection, tooth sensitivity, and avoiding development of subsequent caries lesions.
Case Histories
This report documents treatment for several children. The cases included interim repair of three malformed first permanent molars in two children using direct application of tooth-colored adhesive restorative material in lieu of full-coverage stainless steel crown restoration. New materials are discussed that were not described in the author’s prior technique articles. A novel calcium silicate light-hardened liner was used for pulpal healing and protection, along with a 38% silver diamine fluoride (SDF) solution that addressed tooth sensitivity and for one molar. Use of a preformed stainless steel orthodontic molar band as a matrix, with the rubber dam retainer in place, is also demonstrated, along with use of a unique resin-modified glass-ionomer (RMGI) bioactive ionic resin-based composite.5 Disinfection of the cavity preparation was performed using a 5% glutaraldehyde/hydroxyethylmethacrylate (HEMA) solution. A patient who had stainless steel crown repair of a maxillary first molar is also documented, and one patient whose non-restorable maxillary and mandibular first molars were extracted is shown, with subsequent extraction site replacement by the second and third molars, over the years.
Case 1
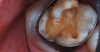
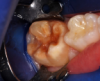
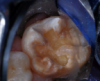
A 9-year-old boy had a partially erupted mandibular first molar with much hypocalcification of the occlusal surface and a large caries lesion involving the occlusal and buccal surfaces (Figure 1). The patient complained of continuing sensitivity to cold stimulus and air inspiration. Because the tooth was only partially erupted, consideration for stainless steel crown full coverage had to be delayed. As an interim repair, it was decided to debride the carious tooth substance and place a light-hardened calcium silicate/mineral trioxide aggregate (MTA) liner, followed by a bonded restoration. After inferior alveolar block anesthetic injection and cotton roll isolation, cavity outline form was cut using a high-speed, water-cooled, medium-grit cylindrical diamond bur (Figure 2). Insufficient eruption precluded use of a rubber dam. A large, round bur at slow speed was used to debride the carious enamel and dentin. The prepared surfaces were swabbed for two 60-second applications of a 5% glutaraldehyde/HEMA solution for desensitization and disinfection of the preparation.6,7 Cavity liner was then injected and spread over the deepest sections of the cavity floor and hardened with the visible light beam (Figure 3). After a self-etching bonding agent was applied over the remaining enamel surfaces, without the need for any type of matrix, an RMGI bioactive ionic resin-based composite was injected, in one portion, into the preparation and spread over the four cusps using a ball burnisher. This restorative complex was then photo-polymerized using two 20-second exposures of the visible light beam (1,200 mW/cm2). The restoration was trimmed and finished with large, round diamond burs at slow speed, and occlusion was evaluated with articulating paper and adjusted.
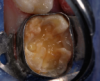
The repaired molar is shown immediately after treatment (Figure 4) and at 13 months (Figure 5). It was hoped that the restoration of the molar would last long enough that stainless steel crown full coverage would not be needed before precision cast crown placement late in the teen or adult years. However, stainless steel crown coverage could be considered, as needed, pending more eruption of the tooth.
Case 2
The same boy pictured in Case 1, in another dentistry office, had occlusal-lingual resin-based composite restoration of his malformed maxillary right first molar about 18 months previously. The bonded repair had been completed expertly and was holding up well. However, the boy developed a new caries lesion involving the distolingual cusp (Figure 6). After local infiltration anesthetic injection, a cotton roll was placed in the mucobuccal fold to absorb saliva from the parotid duct in the cheek.
The occlusal-distolingual tooth preparation was completed, and a stainless steel orthodontic band was pressed into place to serve as a matrix (Figure 7). After two 60-second applications of a 5% glutaraldehyde/HEMA desensitizing solution, a self-etching bonding agent was painted on the enamel surfaces. An RMGI bioactive ionic resin-based composite was then injected in two portions (Figure 8), with 10-second light beam exposure between the injections. After the material was injected to overfill, the light beam was applied once more, for 20 seconds (Figure 9). The restoration was then trimmed and finished in the usual manner using large, round diamond burs at slow speed and diamond finishing burs on the axial surfaces (Figure 10). The self-etching bonding agent was then applied as a final glaze, and occlusal contacts were adjusted using articulating paper as a guide.
One year after restoration, the patient presented with a section of the composite fractured from the distobuccal aspect of the tooth (Figure 11). That cusp was hypoplastic but not carious, and the patient complained of sensitivity to cold and inspired air. Three applications of 38% SDF solution were painted over the region, with gentle air drying after each application (Figure 12 and Figure 13). The patient reported no sensitivity immediately after treatment, and 3 months later the SDF was applied again. The patient denied having any sensitivity since the first SDF treatment.
Case 3
A 7-year-old boy had a newly erupted mandibular right permanent first molar. The tooth had hypoplastic and hypocalcification malformation and associated dental caries (Figure 14). After inferior alveolar block anesthetic injection, the rubber dam was applied using the slit-dam method.8 Occlusal-distobuccal preparation was completed using a water-cooled, coarse-grit cylindrical diamond bur. All carious and chalky hypocalcified tooth structure was removed. Preparation design included mechanical undercut retention form (Figure 15). After placement of an orthodontic band as a matrix, without removal of the rubber dam clamp, 5% glutaraldehyde/HEMA desensitizing solution was applied and agitated with a microbrush for two 60-second exposures, and air-dried after each application (Figure 16). A self-etching bonding agent was then painted over the enamel and dentin and spread to a thin layer with the air syringe. After 10 seconds of light exposure, an RMGI bioactive ionic resin-based composite was injected to overfill, in one portion. The restoration was trimmed with slow-speed diamond burs, and the self-etching bonding agent was applied over the composite surfaces and surrounding enamel. The light beam was applied for another 10 seconds (Figure 17). Occlusion was determined using articulating paper, and corrections were made (Figure 18). The occlusal view of the restored molar is shown 20 months after treatment (Figure 19).
Case 4
A 7-year-old boy originally had resin-based composite repair of his severely malformed permanent molar elsewhere. Chronic tooth sensitivity followed, and the resin-based composite repair failed (Figure 20). The tooth was then restored with a preformed stainless steel crown with careful marginal trimming, crimping, finishing, and polishing, using the methods of Croll and Castaldi (Figure 21 through Figure 23).1,9 The crown is shown 18 months after treatment (Figure 24). This treatment was reported as Case 4 in a prior publication.4 Two years after crown placement, the mesial marginal ridge of the adjacent second molar engaged the distal margin of the stainless steel crown (Figure 25). An orthodontic band was pressed firmly into place over the steel crown, for 3 months, serving to distally reposition the second molar (Figure 26 and Figure 27).
Case 5
In 1998, a 7-year-old boy was brought in for emergency care with the chief complaint of toothache of the mandibular left permanent first molar. The malformed tooth was non-restorable and extracted, with no other treatment options. The child was not returned for continuing routine care but was returned on an emergency basis in 1999. He had a dentoalveolar abscess of the severely carious maxillary left permanent first molar, and the tooth was judged non-restorable (Figure 28). That molar was extracted. The patient was not returned to the office again until 4 years later, in 2003. The maxillary second molar had migrated into good position distal to the second premolar, and the third molar followed into place (Figure 29). The mandibular second molar was tipped mesially, followed by the crown of the third molar. Four years after that (2007), the patient returned as a 15-year-old. The second and third molars had migrated into position, with no orthodontic intervention (Figure 30).
Discussion
With severe coronal enamel malformation with or without dental caries, adhesively bonded direct application resin-based composite materials or any of the glass-ionomer systems may not be durable enough for tooth repair with extended longevity. Full coverage with preformed stainless steel crown forms or extraction of certain teeth may prove to be the best alternatives.10-12 When tooth extraction is considered, the dentist needs to have assurance that the second and third molars are evident, in acceptable positions and with early root formation. Parents need to know that orthodontic treatment may be necessary for ideal tooth positioning, and orthodontic specialty consultation is often advisable.
The patients in Cases 1, 2, and 3 had their molars restored with an RMGI bioactive ionic resin-based composite.5 The material has characteristics of both RMGI cements and resin-based composites. The author has completed over 2,560 primary and permanent tooth restorations with the material since February 2014. Three years of clinical observations and many research reports have revealed the durability and reliability of this restorative material.13-21 The novel calcium silicate light-hardened dentin liner used has become a standard that protects the pulp and cut dentin and supplies calcium ions for pulpal healing.22,23 It is proving itself invaluable in cases of deep dentinal penetration as an indirect pulp cap material and in some cases for direct pulp capping. SDF not only is becoming a valuable densensitizing agent, it also is showing great promise intercepting progression of dental caries lesions.24
About the Author
Theodore P. Croll, DDS
Private Practice
Doylestown, Pennsylvania
Affiliate Professor
Department of Pediatric Dentistry
University of Washington School of Dentistry
Seattle, Washington
Adjunct Professor
Department of Pediatric Dentistry
University of Texas Health Science Center
San Antonio, Texas
Queries to the author regarding this course or the specific products used may be submitted to authorqueries@aegiscomm.com.
References
1. Croll TP, Castaldi CR. The preformed stainless steel crown for restoration of permanent posterior teeth in special cases. J Am Dent Assoc. 1978;97(4):644-649.
2. Croll TP. Preformed posterior stainless steel crowns: an update. Compend Contin Educ Dent. 1999;20(2):89-100.
3. Croll TP. Restorative options for malformed permanent molars in children. Compend Contin Educ Dent. 2000;21(8):676-682.
4. Croll TP. Treatment options for hypoplastic and hypocalcified permanent molars in children. Inside Dentistry. 2014;10(8):58-66.
5. Croll TP, Berg JH, Donly KJ. Dental repair material: a resin-modified glass-ionomer bioactive ionic resin-based composite. Compendium Contin Educ Dent. 2015;36(1):60-65.
6. Christensen R. Disinfection of tooth preparations-why and how? Clinicians Report. 2009;2(11):1-2.
7. Christensen R. Focus on: tooth preparation disinfection. Dent Today. 2014;33(3):16.
8. Croll TP. Alternative methods for use of the rubber dam. Quintessence Int. 1985;16(6):387-392.
9. Croll TP, Epstein DW, Castaldi CR. Marginal adaptation of stainless steel crowns. Pediatr Dent. 2003;25(3):249-252.
10. Cobourne MT, Williams A, Harrison M. National clinical guidelines for the extraction of first permanent molars in children. Br Dent J. 2014;217(11):643-648.
11. Eichenberger M, Erb J, Zwahlen M, Schätzle M. The timing of extraction of non-restorable first permanent molars: a systematic review. Eur J Paediatr Dent. 2015;16(4):272-278.
12. Jälevik B, Möller M. Evaluation of spontaneous space closure and development of permanent dentition after extraction of hypomineralized permanent first molars. Int J Paediatr Dent. 2007;17(5):328-335.
13. Garcia-Godoy F, Morrow BR, Pameijer CH. Flexural strength and fatigue of new Activa RMGICs [abstract]. J Dent Res. 2014;93(spec iss A). Abstract 254.
14. Girn VS, Chao W, Harsono M, et al. Comparison of mechanical properties of dental restorative material [abstract]. J Dent Res. 2014;93(spec iss A). Abstract 1163.
15. Pameijer CH, Garcia-Godoy F, Morrow BR, Jefferies SR. Flexural strength and flexural fatigue properties of resin-modifed glass ionomers. J Clin Dent. 2015;26(1):23-27.
16. Garcia-Godoy F, Morrow BR. Wear resistance of new Activa compared to other restorative materials [abstract]. J Dent Res. 2015;94(spec iss A). Abstract 3522.
17. Bansal R, Burgess J, Lawson NC. Wear of an enhanced resin-modified glass-ionomer restorative material. Am J Dent. 2016;29(3):171-174.
18. Chao W, Girn V, Harsono M, et al. Comparison of deflection at break of four dental restorative materials [abstract]. J Dent Res. 2015;94(spec iss A). Abstract 2375.
19. Daddona J. Compressive strength and deflection at break of four cements [abstract]. J Dent Res. 2016;95(spec iss A). Abstract 0658.
20. Slowikowski L, John S, Finkelman M, et al. Fluoride ion release and recharge over time in three restoratives [abstract]. J Dent Res. 2014;93(spec iss A). Abstract 268.
21. Murali S. Fluoride release of bioactive restoratives with bonding agents [abstract]. J Dent Res. 2016;95(spec iss A). Abstract 0368.
22. Gandolfi MG, Siboni F, Taddei P, et al. Apatite-forming ability of TheraCal pulp-capping material [abstract]. J Dent Res. 2011;90(spec iss A). Abstract 2520.
23. Gandolfi MG, Siboni F, Prati C. Chemical-physical properties of TheraCal, a novel light-curable MTA-like material for pulp capping. Int Endod J. 2012;45(6):571-579.
24. Croll TP, Berg JH. Delivery of fluoride solutions to proximal tooth surfaces. Part II: Caries interception with silver diamine fluoride. Inside Dentistry. 2017;13(9):56-58.