You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Sleep problems in our society are very prevalent. National Sleep Foundation surveys show that 75% of Americans report at least one sleep symptom and approximately 60% of adults drive while drowsy each year.1 Sixty-seven percent of adults snore. This condition affects the quality of their sleep and the sleep of others near them. Obstructive sleep apnea (OSA) is one of the most prevalent sleep disorders and is affecting 26% of adults between the ages of 30 and 70.2 People with untreated OSA can experience a significantly reduced quality of life. It can lead to difficulty in daytime functioning due to daytime sleepiness, fatigue, irritability, and decreased cognitive function. In addition, research studies show that people with OSA have a higher risk of cardiovascular disease (hypertension, heart attack, stroke, atrial fibrillation, etc.), diabetes, asthma, cancer, and dementia.3,4 People with this condition are also more likely to have motor vehicle accidents, which affects everyone.5,6
Part I of this series addressed the physiology, diagnosis, and medical and dental consequences of OSA, and can be accessed at insidedentaltech.com/idt849. This article will cover the management of OSA, as well as the current state of screening for OSA in the dental practice.
Management Strategies
CPAP
Continuous Positive Airway Pressure (CPAP) is the gold-standard treatment for OSA.23,37 Using a mask worn on the face, air is forced into the nose and/or mouth to keep the airway from collapsing during sleep. The pressure required to maintain a patent upper airway is traditionally determined by a second sleep study or the second half of the diagnostic study (see Part I). During this CPAP titration, the technologist systematically increases the air pressure while respiration data are being inspected (Figure 1). The aim is to determine the minimum pressure that keeps the airway open during those conditions in which the airway is most likely to collapse, specifically REM sleep and supine sleep (sleeping on one’s back). Because of the expense of a second sleep study, some third-party payers prefer that the patient be prescribed a CPAP machine that automatically determines the pressure (auto-CPAP), thus forgoing CPAP titration in a sleep laboratory.
CPAP reduces the apnea-hypopnea index (AHI) to <10 events>38,39 However, only about 50% of patients are able to tolerate its use long-term, and it is also very common for patients to use their CPAP for only 4-6 hours per night.40,41 Patient complaints include: presence and contact by headgear and chin straps, claustrophobia, unstable or inadequate fit of mask to facial contours, air leakage, mask-related skin ulceration and headache, aerophagia (swallowing air), and uncomfortably high pressure levels (Figure 2).42,43 Durable medical equipment (DME) providers work with patients to find a comfortable mask and level of humidification to improve tolerance. Some patients find modified forms of CPAP more tolerable, eg, Auto-CPAP in which an onboard computer determines the appropriate pressure from moment to moment, or Bi-level-CPAP, in which a higher pressure is delivered during inspiration and a lower pressure during expiration. Cognitive behavioral training has been used in an attempt to desensitize patients to the use of CPAP and thus improve adherence to therapy.
Based on studies of patients’ use of CPAP and its impact on daytime sleepiness and quality of life, compliance to therapy has been defined as use for a minimum of four hours per night on at least five nights per week.42 This definition is often used, as well, for other therapies for OSA. Most CPAP machines today have monitoring chips that record nightly use, pressure delivered, and measures of sleep respiration pertaining to the efficacy of therapy. This information can either be downloaded by the DME company or clinician, or with some new systems automatically transmitted via cell phone or Internet directly to the DME company or treating physician, who is able to make adjustments to the machine’s settings remotely.
Oral Appliances
Oral appliances represent an alternative to CPAP.44 Most commonly used is a mandibular advancement device (MAD), also known as a mandibular advancement splint (MAS) or mandibular repositioning appliance (MRA) (Figure 3). The custom-fabricated, adjustable MAD is recognized as the standard-of-care oral appliance by the American Academy of Dental Sleep Medicine, and is the appliance of most relevance to the dental technologist.45 It will be described in detail in Parts III and IV of this series.
In addition to MADs, other oral appliances used to treat SDB include tongue devices.46,47,48 These devices include stock/prefabricated (Figure 4) or custom-fabricated (Figure 5) suction cups to hold the tongue forward or a dental appliance that pushes the base of the tongue forward using an acrylic appendage from the posterior aspect of the appliance (Figure 6). These tongue devices are used less frequently than MADs but may be indicated for edentulous patients, patients undergoing orthodontic treatment, or patients who cannot protrude the jaw (as is the case of patients who have undergone joint replacement surgery).
The MAD improves airway patency by stabilizing the jaw in a forward and (typically) closed mouth position.45 Because the tongue, its base, and the soft palate have attachments to the jaw, these tissues move forward, increasing the upper airway space. Also, the jaw is prevented from sliding or rotating backward during supine sleep. Both actions, if not prevented, can lead to upper airway collapse. Because airflow behind the soft palate becomes less turbulent and/or the soft palate becomes tauter, snoring is reduced or eliminated. Some studies have argued that neuromuscular reflexes that protect the airway work more effectively when a patient with OSA uses a MAD.49
Based on literature prior to 2005, MADs were found to reduce the AHI to <10 events>44 Multiple studies over the past decade, however, have shown that when properly adjusted, MADs are not inferior to CPAP in efficacy for patients with mild or moderate disease and that a higher percentage of patients with severe OSA — as high as 60% — can be adequately treated.38,39 The literature also confirms that any shortfall in efficacy compared to CPAP is compensated by the substantially better compliance to therapy.50,51 Reports over the past 15 years suggest that approximately 75% of patients are still using their appliance 2-3 years after delivery.52,53
Recently, compliance monitors, simpler than those used in CPAP machines, have been introduced for MADs (Figure 7).51,54,55 They are fabricated into the oral appliance by the dental laboratory technologist (Figure 8). Based on early studies with these types of monitoring devices, approximately 80% of patients were found to be compliant at one year post-delivery of appliance.51 Patients’ reports of utilization match the data recorded by these chips remarkably well. With greater utilization of therapy even with lower efficacy, MADs provide similar treatment effectiveness to that of CPAP and are predicted to have similar long-term outcomes on health. The limited studies conducted to date show that MADs and CPAP are equally effective in improving cardiovascular outcomes in patients with OSA.56,57
Combination Therapy
Approximately 25% of patients will not respond adequately to MAD therapy.38,39,58 If these patients have failed CPAP therapy, combination therapy provides the next logical step in the patients’ treatment (Figure 9 ).59 When used in combination with CPAP, a MAD serves as an adjunct to improve its tolerance by lowering the pressure required to keep the airway open.60 With lower pressures, there are fewer pressure-related complaints that often lead patients to abandon therapy. These include air leakage and need to over-tighten the mask, arousals from sleep due to the air stimulation, and air entering the stomach (aerophagia). MADs also stabilize the jaw in a forward and upward position, thereby improving the fit and stability of masks that cover both the nose and mouth or eliminating the need for a full-face mask. Because the oral appliance lowers the upper airway resistance, the efficacy of CPAP can be improved. The use of a MAD to improve the tolerance and efficacy of CPAP remains largely “off-label,” although some third-party payers will cover both therapies at the same time. Research funding has not been available to conduct randomized clinical trials to study this innovative therapy, limiting its endorsement.
Other therapies that are used in combination with MADs are tongue devices and positional therapy (forced side-sleeping).61,62 In these cases, treatment with the MAD constitutes the primary therapy. The tongue device or positional therapy is considered adjunctive. The aim of these combination therapies is to reduce the frequency of respiratory events below the level achieved by use of the MAD alone.
Surgery
Many different types of surgical procedures for the soft tissues are used to increase the upper airway space. These involve using a scalpel, laser, or tissue-lesioning probe to reduce the mass of the soft palate or base of the tongue.63,64 The most common procedure historically has been uvulopalatopharyngoplasty (UPPP), or laser-assisted uvulopalatopharyngoplasty (LAUP), in which a crescent-shaped section of the soft palate is removed, including the uvula and tonsils (Figure 10 and 11). Given its poor to moderate efficacy, this procedure is used today sparingly for snoring and mild forms of SDB, but rarely for more severe forms of OSA.
In contrast to soft-tissue surgery, greater success has been reported for surgery that increases upper airway size by repositioning anteriorally the maxilla and/or mandible (Figure 12 and 13). Maxillomandibular advancement surgery for OSA involves one or more of the following: Le Fort I osteotomy, in which the maxilla is moved forward; bilateral split sagittal osteotomy, in which the body of the mandible is moved forward; and anterior inferior mental osteotomy, in which the chin is moved forward (Figure 14).65,66,67 Orthodontics is required before and after the surgery. The surgery is usually reserved for patients with severe OSA who cannot tolerate CPAP, and has been reported successful in 65-100% of patients depending on the definition of success. Unlike CPAP and oral appliances, the surgery attempts to cure, rather than manage, OSA, and compliance to therapy is 100%.
Other
Because many, if not most, patients have worse OSA when sleeping on their back than on their sides, side sleeping can be an important adjunct to other therapies for OSA or serve as an adequate monotherapy in patients who have OSA only when sleeping on their back.62 Belts and nightshirts that restrict patients’ ability to sleep on their back are commercially available.
The avoidance of substances that relax the muscles or obtund airway protective reflexes (alcohol and sedatives) is also often recommended.68 Weight loss in obese patients will decrease the severity of OSA (but will rarely cure it) and will improve the efficacy of oral appliances.69
Nasal decongestants or surgery are indicated for patients who cannot breathe through their nose while sleeping. Although not curative, measures to restore normal nasal patency can improve the effectiveness of CPAP and of oral appliances.70
Other therapies that have been introduced recently include oral suction to pull the soft palate and tongue forward, and hypoglossal nerve stimulators.71 The implanted nerve stimulator monitors sleep respiration and electrically stimulates the genioglossus muscle when breathing becomes labored, thereby increasing airway patency.
Sleep Medicine in Dentistry
Sleep Medicine in dentistry includes screening for SDB, oral appliance therapy for SDB, and orthognathic surgery and orthodontic therapies, such as Rapid Maxillary Expansion (RME), for SDB. A short discussion on screening for SDB is presented below. Parts III and IV of this series will focus on oral appliance therapy. Orthognathic surgery and orthodontics for SDB will not be considered in this series.
Screening in Dental Practice
Screening for hypertension in the dental office is standard of care. It leads to the identification of patients at risk for cardiovascular disease and their subsequent treatment. In contrast, screening for OSA — almost as prevalent in the adult population as hypertension — is rarely performed. No guidelines for the general screening of patients in a dental practice have been established and validated. Best practice dictates that patients with both clinical findings suggestive of SDB and who screen “at risk” on OSA questionnaires should be advised to see their physician or a sleep physician for an evaluation to rule out or identify sleep apnea.
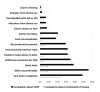
Clinical findings suggestive of SDB include: being overweight, a large neck circumference/cervical fat, a small and/or retruded jaw, dental attrition (bruxism) or erosion (GERD), a long face, a narrow arch form with large or thick tongue, a long soft palate and/or uvula, large tonsils crowding the airway, presence of respiratory sounds in supine position, and falling asleep during the dental appointment (Figure 15).15,16,17 OSA questionnaires assess patients’ reports of symptoms of SDB including snoring, being told by others that their breathing stopped during sleep, daytime sleepiness or fatigue, and hypertension.72 The most common screening questionnaires were developed for administration to patients prior to surgery and thus have good to excellent sensitivity, but moderate to poor specificity.73 Thus, their use without consideration of clinical indicators of SDB classifies “at risk” a large number of patients who do not have OSA. The use of home sleep apnea testing for general screening for SDB is not endorsed by the American Academy of Sleep Medicine.19 It is particularly ill advised in the dental setting, as home sleep testing is not able to rule out sleep apnea, only in.
Patients who have OSA utilize health care resources at twice the rate of those without OSA for as far back as 10 years before they are diagnosed.74 The use of health care dollars for untreated OSA is in the billions each year. Despite the prevalence of this disorder, the impact on a person’s health and life, and the economic burden of this condition, only 15-20% of the individuals with OSA have been diagnosed.75 It is the responsibility of physicians, dentists, and other health care providers to identify people at high risk for OSA and to encourage them to have the problem evaluated, diagnosed and treated.
Disclosure
The authors had no disclosures to report.
References
1. National Sleep Foundation 2005 Sleep in America Poll. https://sleepfoundation.org/sites/default/files/2005_summary_of_findings.pdf. Published March 29, 2005. Accessed October 3, 2015.
2. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. May 1 2013;177(9):1006-1014.
3. Huang QR, Qin Z, Zhang S, Chow CM. Clinical patterns of obstructive sleep apnea and its comorbid conditions: a data mining approach. J Clin Sleep Med. Dec 15 2008;4(6):543-550.
4. Abrams B. Hierarchy of comorbidity indicators for obstructive sleep apnea. Chest. Jun 2010;137(6):1491-1492.
5. Hiestand D, Phillips B. Obstructive sleep apnea syndrome: assessing and managing risk in the motor vehicle operator. Curr Opin Pulm Med. Nov 2011;17(6):412-418.
6. Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med. Dec 15 2009;5(6):573-581.
7. Tsuiki S, Isono S, Ishikawa T, Yamashiro Y, Tatsumi K, Nishino T. Anatomical balance of the upper airway and obstructive sleep apnea. Anesthesiology. Jun 2008;108(6):1009-1015.
8. Isono S, Tanaka A, Tagaito Y, Ishikawa T, Nishino T. Influences of head positions and bite opening on collapsibility of the passive pharynx. J Appl Physiol (1985). Jul 2004;97(1):339-346.
9. Watanabe T, Isono S, Tanaka A, Tanzawa H, Nishino T. Contribution of body habitus and craniofacial characteristics to segmental closing pressures of the passive pharynx in patients with sleep-disordered breathing. Am J Respir Crit Care Med. Jan 15 2002;165(2):260-265.
10. Remmers JE, deGroot WJ, Sauerland EK, Anch AM. Pathogenesis of upper airway occlusion during sleep. J Appl Physiol Respir Environ Exerc Physiol. Jun 1978;44(6):931-938.
11. Fietze I, Quispe-Bravo S, Hansch T, Rottig J, Baumann G, Witt C. Arousals and sleep stages in patients with obstructive sleep apnoea syndrome: Changes under nCPAP treatment. J Sleep Res. Jun 1997;6(2):128-133.
12. Guilleminault C, Partinen M, Quera-Salva MA, Hayes B, Dement WC, Nino-Murcia G. Determinants of daytime sleepiness in obstructive sleep apnea. Chest. Jul 1988;94(1):32-37.
13. Capdevila OS, Kheirandish-Gozal L, Dayyat E, Gozal D. Pediatric obstructive sleep apnea: complications, management, and long-term outcomes. Proc Am Thorac Soc. Feb 15 2008;5(2):274-282.
14. Arnardottir ES, Mackiewicz M, Gislason T, Teff KL, Pack AI. Molecular signatures of obstructive sleep apnea in adults: a review and perspective. Sleep. Apr 2009;32(4):447-470.
15. Friedman M, Tanyeri H, La Rosa M, et al. Clinical predictors of obstructive sleep apnea. Laryngoscope. Dec 1999;109(12):1901-1907.
16. Shigemoto S, Shigeta Y, Nejima J, Ogawa T, Matsuka Y, Clark GT. Diagnosis and treatment for obstructive sleep apnea: Fundamental and clinical knowledge in obstructive sleep apnea. J Prosthodont Res. Jul 2015;59(3):161-171.
17. Gharibeh T, Mehra R. Obstructive sleep apnea syndrome: natural history, diagnosis, and emerging treatment options. Nat Sci Sleep. 2010;2:233-255.
18. Kakkar RK, Hill GK. Interpretation of the adult polysomnogram. Otolaryngol Clin North Am. Aug 2007;40(4):713-743.
19. Collop NA, Anderson WM, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. Dec 15 2007;3(7):737-747.
20. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. Oct 15 2012;8(5):597-619.
21. Thomas RJ, Guilleminault C, Ayappa I, Rapoport DM. Scoring respiratory events in sleep medicine: who is the driver--biology or medical insurance? J Clin Sleep Med. Nov 15 2014;10(11):1245-1247.
22. Guilleminault C, Stoohs R, Clerk A, Cetel M, Maistros P. A cause of excessive daytime sleepiness. The upper airway resistance syndrome. Chest. Sep 1993;104(3):781-787.
23. Epstein LJ, Kristo D, Strollo PJ, Jr., et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. Jun 15 2009;5(3):263-276.
24. Asker M, Asker S, Kucuk U, Kucuk HO. An overlooked cause of resistant hypertension: upper airway resistance syndrome - preliminary results. Clinics (Sao Paulo). Nov 2014;69(11):731-734.
25. Sanders AE, Essick GK, Beck JD, et al. Periodontitis and Sleep Disordered Breathing in the Hispanic Community Health Study/Study of Latinos. Sleep. Dec 20 2014.
26. Berger G, Berger R, Oksenberg A. Progression of snoring and obstructive sleep apnoea: the role of increasing weight and time. Eur Respir J. Feb 2009;33(2):338-345.
27. Bao G, Guilleminault C. Upper airway resistance syndrome--one decade later. Curr Opin Pulm Med. Nov 2004;10(6):461-467.
28. Dubrovsky B, Raphael KG, Lavigne GJ, et al. Polysomnographic investigation of sleep and respiratory parameters in women with temporomandibular pain disorders. J Clin Sleep Med. Feb 15 2014;10(2):195-201.
29. Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. Aug 2008;31(8):1079-1085.
30. Ancoli-Israel S, Palmer BW, Cooke JR, et al. Cognitive effects of treating obstructive sleep apnea in Alzheimer's disease: a randomized controlled study. J Am Geriatr Soc. Nov 2008;56(11):2076-2081.
31. Al-Jewair TS, Al-Jasser R, Almas K. Periodontitis and obstructive sleep apnea's bidirectional relationship: a systematic review and meta-analysis. Sleep Breath. Mar 24 2015.
32. Sanders AE, Essick GK, Fillingim R, et al. Sleep apnea symptoms and risk of temporomandibular disorder: OPPERA cohort. J Dent Res. Jul 2013;92(7 Suppl):70S-77S.
33. Carra MC, Bruni O, Huynh N. Topical review: sleep bruxism, headaches, and sleep-disordered breathing in children and adolescents. J Orofac Pain. Fall 2012;26(4):267-276.
34. Manfredini D, Restrepo C, Diaz-Serrano K, Winocur E, Lobbezoo F. Prevalence of sleep bruxism in children: a systematic review of the literature. J Oral Rehabil. Aug 2013;40(8):631-642.
35. De Luca Canto G, Singh V, Gozal D, Major PW, Flores-Mir C. Sleep bruxism and sleep-disordered breathing: a systematic review. J Oral Facial Pain Headache. Fall 2014;28(4):299-305.
36. Raphael KG, Janal MN, Sirois DA, et al. Validity of self-reported sleep bruxism among myofascial temporomandibular disorder patients and controls. J Oral Rehabil. May 26 2015.
37. Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. Apr 18 1981;1(8225):862-865.
38. Hoekema A, Stegenga B, Wijkstra PJ, van der Hoeven JH, Meinesz AF, de Bont LG. Obstructive sleep apnea therapy. J Dent Res. Sep 2008;87(9):882-887.
39. Holley AB, Lettieri CJ, Shah AA. Efficacy of an adjustable oral appliance and comparison with continuous positive airway pressure for the treatment of obstructive sleep apnea syndrome. Chest. Dec 2011;140(6):1511-1516.
40. Rauscher H, Popp W, Wanke T, Zwick H. Acceptance of CPAP therapy for sleep apnea. Chest. Oct 1991;100(4):1019-1023.
41. Stepnowsky CJ, Jr., Moore PJ. Nasal CPAP treatment for obstructive sleep apnea: developing a new perspective on dosing strategies and compliance. J Psychosom Res. Jun 2003;54(6):599-605.
42. Kribbs NB, Pack AI, Kline LR, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. Apr 1993;147(4):887-895.
43. Pepin JL, Leger P, Veale D, Langevin B, Robert D, Levy P. Side effects of nasal continuous positive airway pressure in sleep apnea syndrome. Study of 193 patients in two French sleep centers. Chest. Feb 1995;107(2):375-381.
44. Ferguson KA, Cartwright R, Rogers R, Schmidt-Nowara W. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep. Feb 2006;29(2):244-262.
45. Scherr SC, Dort LC, Almeida FR, et al. Definition of an effective oral appliance for the treatment of obstructive sleep apnea and snoring: A report of the American Academy of Dental Sleep Medicine. Journal of Dental Sleep Medicine. 2014;1(1):39-50.
46. Deane SA, Cistulli PA, Ng AT, Zeng B, Petocz P, Darendeliler MA. Comparison of mandibular advancement splint and tongue stabilizing device in obstructive sleep apnea: a randomized controlled trial. Sleep. May 2009;32(5):648-653.
47. Cartwright RD. Predicting response to the tongue retaining device for sleep apnea syndrome. Arch Otolaryngol. Jun 1985;111(6):385-388.
48. Singh GD, Keropian B, Pillar G. Effects of the full breath solution appliance for the treatment of obstructive sleep apnea: a preliminary study. Cranio. Apr 2009;27(2):109-117.
49. Yoshida K. A polysomnographic study on masticatory and tongue muscle activity during obstructive and central sleep apnea. J Oral Rehabil. Aug 1998;25(8):603-609.
50. Phillips CL, Grunstein RR, Darendeliler MA, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med. Apr 15 2013;187(8):879-887.
51. Dieltjens M, Braem MJ, Vroegop AV, et al. Objectively measured vs self-reported compliance during oral appliance therapy for sleep-disordered breathing. Chest. Nov 2013;144(5):1495-1502.
52. de Almeida FR, Lowe AA, Tsuiki S, et al. Long-term compliance and side effects of oral appliances used for the treatment of snoring and obstructive sleep apnea syndrome. J Clin Sleep Med. Apr 15 2005;1(2):143-152.
53. Marklund M, Stenlund H, Franklin KA. Mandibular advancement devices in 630 men and women with obstructive sleep apnea and snoring: tolerability and predictors of treatment success. Chest. Apr 2004;125(4):1270-1278.
54. Smith YK, Verrett RG. Evaluation of a novel device for measuring patient compliance with oral appliances in the treatment of obstructive sleep apnea. J Prosthodont. Jan 2014;23(1):31-38.
55. Bonato RA, Bradley DC. Introducing a Novel Micro-recorder for the Detection of Oral Appliance Compliance: DentiTrac(R). Sleep Diagnosis and Therapy. 2013;8(3):12-15.
56. Iftikhar IH, Hays ER, Iverson MA, Magalang UJ, Maas AK. Effect of oral appliances on blood pressure in obstructive sleep apnea: a systematic review and meta-analysis. J Clin Sleep Med. Feb 1 2013;9(2):165-174.
57. Lin CC, Wang HY, Chiu CH, Liaw SF. Effect of oral appliance on endothelial function in sleep apnea. Clin Oral Investig. Mar 2015;19(2):437-444.
58. Fleury B, Rakotonanahary D, Petelle B, et al. Mandibular advancement titration for obstructive sleep apnea: optimization of the procedure by combining clinical and oximetric parameters. Chest. May 2004;125(5):1761-1767.
59. Sanders AE, Denbar MA, White J, et al. Dental clinicians’ observations of combination therapy in PAP-intolerant patients. Sleep Review Magazine. 2015;16(4):18-21.
60. El-Solh AA, Moitheennazima B, Akinnusi ME, Churder PM, Lafornara AM. Combined oral appliance and positive airway pressure therapy for obstructive sleep apnea: a pilot study. Sleep Breath. May 2011;15(2):203-208.
61. Dort L, Remmers J. A combination appliance for obstructive sleep apnea: the effectiveness of mandibular advancement and tongue retention. J Clin Sleep Med. Jun 15 2012;8(3):265-269.
62. Ravesloot MJ, van Maanen JP, Dun L, de Vries N. The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea-a review of the literature. Sleep Breath. Mar 2013;17(1):39-49.
63. Sundaram S, Bridgman SA, Lim J, Lasserson TJ. Surgery for obstructive sleep apnoea. Cochrane Database Syst Rev. 2005(4):CD001004.
64. Elshaug AG, Moss JR, Southcott AM, Hiller JE. Redefining success in airway surgery for obstructive sleep apnea: a meta analysis and synthesis of the evidence. Sleep. Apr 2007;30(4):461-467.
65. Prinsell JR. Maxillomandibular advancement surgery in a site-specific treatment approach for obstructive sleep apnea in 50 consecutive patients. Chest. Dec 1999;116(6):1519-1529.
66. Hsieh YJ, Liao YF. Effects of maxillomandibular advancement on the upper airway and surrounding structures in patients with obstructive sleep apnoea: a systematic review. Br J Oral Maxillofac Surg. Dec 2013;51(8):834-840.
67. Camacho M, Teixeira J, Abdullatif J, et al. Maxillomandibular advancement and tracheostomy for morbidly obese obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. Apr 2015;152(4):619-630.
68. Peppard PE, Austin D, Brown RL. Association of alcohol consumption and sleep disordered breathing in men and women. J Clin Sleep Med. Apr 15 2007;3(3):265-270.
69. Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. Dec 20 2000;284(23):3015-3021.
70. Rosow DE, Stewart MG. Is nasal surgery an effective treatment for obstructive sleep apnea? Laryngoscope. Aug 2010;120(8):1496-1497.
71. White DP. New therapies for obstructive sleep apnea. Semin Respir Crit Care Med. Oct 2014;35(5):621-628.
72. Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anaesth. May 2010;57(5):423-438.
73. Kim B, Lee EM, Chung YS, Kim WS, Lee SA. The utility of three screening questionnaires for obstructive sleep apnea in a sleep clinic setting. Yonsei Med J. May 2015;56(3):684-690.
74. Albarrak M, Banno K, Sabbagh AA, et al. Utilization of healthcare resources in obstructive sleep apnea syndrome: a 5-year follow-up study in men using CPAP. Sleep. Oct 2005;28(10):1306-1311.
75. Institute of Medicine (US) Committee on Sleep Medicine and Research. 4. Functional and Economic Impact of Sleep Loss and Sleep-Related Disorders. In: Colten HR, Altevogt BM, editors Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US); 2006: 137-172.
About the Authors
Gregory K. Essick, DDS, PhD
Professor
Department of Prosthodontics and Center for Pain Research and Innovation
School of Dentistry
University of North Carolina
Chapel Hill, NC
Jonathan A. Parker, DDS
Owner, Clinical Director
Snoring and Sleep Apnea Dental Treatment Center
Edina, MN
Jamison R. Spencer, DMD, MS
Director
The Center for Sleep Apnea and TMJ
Boise, ID
Andrew R. Blank, AAS, BS
Dental Student
East Carolina University School of Dental Medicine
Greenville, NC
Part III
The third installment of this four-part series will address oral appliances in detail, including practice guidelines, types of appliances, and side effects of therapy.
This article was double-blind peer reviewed by members of IDT’s Editorial Advisory Board