You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Dental implants have arguably been considered one of the most significant advances in modern dentistry. They have been shown to have a wide range of applications, from single-tooth replacement to fully edentulous reconstructions. It is not uncommon to have success rates quoted in the 95% or higher range, which has, in turn, given both practitioners and patients a sense of confidence with regard to their use.1-4 It may be, however, that this sense of confidence is overstated, as many of the classic studies related to long-term outcomes for dental implants have been reported using tightly controlled patient populations with highly calibrated surgical/restorative treatment teams. In addition, very few of these studies assess the esthetic success of the restoration and rely heavily on “survival data.” Moreover, there is a lack of long-term controlled data regarding hard- and soft-tissue complications and poor esthetic outcomes.5-8
As the use of dental implants expands both in indications and among practitioners of varying levels of training and experience, these high success rates may not be duplicated, and complications seem to be increasing. There is a need to further define treatment-planning protocols as well as to identify risk factors that may be associated with potential complications. For example, Kosldsland and Scheie et al attempted to evaluate the prevalence of peri-implant disease. This included the presence of radiographically detectable bone loss around implants and bleeding on probing, with or without bone loss. They found that assessing peri-implantitis at different levels of severity yielded a substantial variance in prevalence, from 11.3% to 47.1%. However peri-implant inflammation was a frequent finding with and without peri-implant bone loss.9 Some authors have attempted to identify common risk factors to predict hard- and soft-tissue implant complications. A history of aggressive periodontitis, diabetes, and genetic susceptibility via production of pro-inflammatory cytokines, among other factors, have yielded suggested associations with tissue loss and/or implant failure; however, there is a paucity of controlled clinical trials in this area.10,11 Despite a lack of conclusive data with regard to etiology and treatment protocols, the authors wish to explore dental- and patient-related factors that may contribute to complications of hard and soft tissue and how working as a team, implant surgeons and restorative dentists can avoid—or at least mitigate—these conditions.12
Identifying Complications
While the amount of available bone can now be more accurately determined with various 3-dimensional (3-D) studies such as cone beam technology, the goal of therapy ought not simply be to achieve successful osseointegration of an implant. Rather, it is incumbent upon the surgeon to develop adequate, stable hard- and soft-tissue volumes to support the functional/esthetic goal of the overall treatment plan developed by the periodontist/restorative dentist/laboratory technician. If deficiencies in any of these tissues in the implant site itself or of adjacent natural teeth are left untreated, the patient is at greater risk for esthetic and/or functional compromises that can result in significant disappointment for patients and clinicians. In fact, in a recent survey of patients contemplating restorative dentistry, more than 60% reported feeling anxious about the outcome and their concern that the result “may look false or unnatural.”13 Clearly, implant surgeons and restorative dentists need to have open and candid discussions with patients with regard to the limitations with which they present.
Implant complications of hard and soft tissue can be identified, as follows:
- those occurring prior to implant placement
- those occurring at the time of implant placement
- those occurring after implant placement
Similarly, the management of such complications can be undertaken immediately after identification in the planning phase, when periodontists and restorative dentists can identify opportunities and limitations that may impact the results. Once identified, these issues can be managed either prior to implant placement or during the surgical phase of implant placement. The last opportunity to identify complications and address them successfully is during the healing phase, just prior to restorative reconstruction of the implant. Unfortunately, once hard- and soft-tissue complications occur after final restoration, their management becomes more complex and less predictable. Clearly, in areas where tissue deficiencies cannot be reconstructed completely, the patient must be well informed with regard to limitations and functional/esthetic compromises that can occur throughout the treatment phase and, indeed, beyond. Implants may not be a “lifelong solution” in all cases. Moreover, it may not be possible to predict potential complications in the future. The authors would like to illustrate their approach to managing difficulties in the esthetic zone throughout the treatment phases and how support from both a technical and emotional perspective can mitigate potential failures.
Patient Expectations
During the treatment-planning phase, an overall understanding of both the patient’s needs and desires must be well understood.13,14 It seems reasonable to state that the restorative office should work with the patient to focus on potential final restorative treatment. Once the ideal desired treatment is developed, it is also reasonable to expect the surgeon to predict the probability of achieving the surgical result necessary to produce this outcome. Focusing a patient’s understanding of the situation to clarify what he or she “needs” in order to achieve what he or she “desires” is critically important. This negotiation may reveal that the patient does not wish to undergo a needed treatment to achieve the desired result. The treating dentists should be able to lay out the resulting limitations of the final treatment and eliminate any “complication” of unhappy patients when the final result is less than they expected. If the surgical ability to achieve patients’ desires is unlikely, an alternative plan must then be developed or patients must clearly understand and accept this treatment limitation.
Ideal esthetic treatment planning and discussion with patients needs to include a thorough evaluation of the entire anterior quadrant. The potential to do contralateral crown lengthening to help match the expected soft-tissue deficiencies of implant restorations may be an important discussion. Another important consideration is the number of implants needed to replace missing teeth. Almost invariably, patients initially expect individual “teeth” to replace the lost or failing ones. A careful evaluation of the edentulous space should be done with a realization of the difficulty in papilla creation between two implants and especially when they are within 4 mm of each other. Of course, it is well understood that when available space “forces” an implant placement too close to an adjacent natural tooth (< 1.5 mm), the expectation of papilla loss is very high.15,16 It may also be helpful to explain that an ovate pontic supported by a single or multiple implants sometimes has a much higher esthetic potential. From a restorative perspective, it is sometimes more esthetic to splint together multiple crowns, even when they could be separate, to allow the ceramist the greatest opportunity to hide the gingival deficiency. One of the most difficult decisions is the removal of teeth that could be saved to give greater predictability to the functional or esthetic outcome.
Managing Complications
True complications to the planned treatment are first identified at several points. During the surgery, it may be found that the expected bone is not present or will not provide the foundation expected. Management of this level of complication ranges from site development without implant placement, through placement of the implant, perhaps with additional grafting—despite the deficiencies—in the case that it has been determined that the patients’ expectations would still be met with a less-than-perfect implant positioning.17,18
The next level of manageable complications should be considered the initial evaluation at 1 week. Careful assessment of the implant positioning and restorative potential should be made at this point, as this is one of the last opportunities for simple implant removal if it is deemed unlikely to produce the result desired. The next level of evaluation occurs after the initial healing phase is completed. A thorough evaluation is necessary for the implant position, 3-D soft tissue profiles around the implant, adjacent teeth, and the entire anterior segment.19-21 The use of carefully made, implant-supported provisionals during this time period may help diminish esthetic complications with the provisional-guided development of emergence-profile and adjacent ovate pontics. The provisional must be fabricated to mimic the final restoration, and the costs associated with this part of the treatment are very significant. If the provisional costs are not included in the patient’s arrangement, they often become hindrances to implementation. When the best possible outcome with the provisional restoration is evaluated, complications can be identified and managed according to the patient’s needs. For example, an apical emergence profile could be improved esthetically with crown lengthening of the adjacent or contralateral teeth when it is appropriate. A deficiency in the soft-tissue papilla could be mitigated restoratively by restoring the adjacent tooth and the implant to equally obturate the deficiency. Sometimes the planned use of pink porcelain will produce the best possible outcome when a large soft-tissue deficiency is encountered.
The final and highly important consideration before proceeding to the final restoration should be an evaluation of the stability of the implant. Following these steps, from treatment planning through soft-tissue development with a provisional, usually makes the development of the final restoration a straightforward procedure. In addition, the patient knows what to expect and has been given the opportunity to opt in for adjunctive procedures.22-26
Probably the least-understood and most frustrating complication is the very broad category of peri-implantitis, which is most often seen during the maintenance phase of implant treatment. Peri-implant conditions generally are categorized into two diseases: peri-implant mucositis and peri-implantitis. The descriptions of each of these parallel those of gingivitis and periodontitis around teeth. While perimucositis is most often associated with reversible inflammatory reactions in the mucosa surrounding implants, peri-implantitis is the most threatening, as, by definition, it includes loss of supporting bone around the implant. Clearly the complication most associated with a deteriorating prognosis is peri-implantitis, and it is also the least understood. While these conditions around teeth and implants all involve the accumulation and maturation of biofilms, peri-implantitis may differ from periodontitis in several respects. The cell composition and the progression rate appear to differ and can, therefore, affect the prognosis for successful treatment.27 In addition, while the microbiota of both periodontitis and peri-implantitis lesions have similarities, currently there is no universally accepted protocol for treatment of peri-implantitis lesions.28,29 One of the most challenging problems with regard to managing peri-implantitis lesions is differences in implant surfaces and the difficulties associated with debridement techniques.30 Clearly, early diagnosis of this potentially devastating complication is essential in its successful management.31 The authors recommend data collection at periodic maintenance visits, which parallel those of periodontal maintenance patients. This means probing for depth and to assess bleeding on probing with standardized metal probes, radiographics to assess crestal bone status, and possible salivary and pocket culture to assess pathogens. Changes in any of these parameters may be more important than the initial measurement or initial bone level, which may be subject to implant/restoration design. Clearly, however, perimucositis should be addressed during both professional and patient-instituted plaque removal. Prevalence data indicates that mucositis ranges from 32% to almost 80% in some studies. Peri-implantitis is reported to have prevalence rates ranging from 7.5% to more than 50%.32,33 With regard to progressive bone loss in the presence of bleeding on probing and signs of peri-implantitis, these lesions should be managed early with surgical access, as non-surgical debridement has not been shown to be effective.34,35 An extreme example of biologic complications is the rare complete loss of integration of the implant. The reasons are probably varied and many for the complete loss of bone around an implant. The most disappointing is the presence of bone surrounding the implant, but the small radiolucency adjacent to the implant and implant mobility reveal that the stability of the implant has been lost. One important point to remember is that the loss of the implant is often a catastrophic loss to the patient, the restoration, and the restorative dentist. It is, of course, a substantial loss to the surgeon, but it is a serious patient management error to assume that if an implant is lost—even if it will be replaced at no charge by the surgeon—all responsibilities to the patient have been met. This ignores the enormous time and cost that has been invested in the final restoration and does not reflect fair responsibility for treatment integrity. It is imperative that all treating dentists go into the final treatment phase with great confidence that the implants are stable and within every reasonable expectation that they will remain so for an indefinite period. Managing the ultimate complication of implant loss needs to be a team effort that reflects the challenges of each office and the individual patient.
Case Reports
In conclusion, dental implant complications—especially in the esthetic zone—are inevitable to some degree. Minimizing their occurrence and idealizing clinicians’ response to them is critical. The first and foremost step for all practitioners is to have a strong and thorough understanding of predictable treatment protocols. The practitioners’ understanding of realistic potential outcomes allows the effective inclusion of the patient in the treatment planning. The patient’s expectation about the potential outcome should coincide with the informed practitioner’s expectation. A less-than-ideal outcome that is predicted by the practitioner and expected by the patient is not considered a complication. Closely following a patient after treatment completion is important to identify early on a destructive phase that may be initiated, for example, by occlusal forces, poor oral hygiene, etc. Intervention in these cases must be patient-specific and hinges on applicable surgical and restorative techniques. Implant dentistry at its best offers the remarkable promise of restoring to patients something they have lost; and, in the vast majority of cases, when acceptable protocols are followed, the outcomes are truly extraordinary. It is this overwhelming success potential that sometimes causes practitioners to forget that management of complications may be even more important than the initial treatment.
The following case reports are intended to illustrate some of the common issues periodontist/restorative dentist teams face, and how working together can help mitigate their consequences.
Case 1: Use of Cantilevered Anterior Restorations
The chief complaint of a 48-year-old woman who presented to her restorative dentist was, “I don’t like the way my implant looks” (Figure 1). This implant had been placed by a previous periodontist and restorative dentist. The patient is now seeking a second opinion. In evaluating this case upon referral to the periodontist, a reddened appearance of the gingival and mucosal tissue encompassing almost the entire facial aspect could be observed. In addition, the radiographs demonstrated a 5-mm diameter implant in place with a deciduous cuspid in the place of No. 11. Deep probing depths were noted around the facial aspect of the implant, and threads could be detected under the tissue.
In evaluating the options, it was decided that the implant placed was too large and that the deciduous cuspid site could be used for a single implant as an abutment for a cantilevered pontic to restore the missing lateral incisor in a more esthetic manner. The goal the treatment was to augment the lateral incisor site in order to bring the facial tissue level more coronal (Figure 2 through Figure 11).
Case 2: The Value of Crown Lengthening to Achieve Esthetic Results
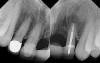
A 53-year-old woman presented with a failing implant in the No. 7 site (Figure 12 and Figure 13). Her desire was to eliminate infection and preserve esthetics. A team effort between the periodontist and restorative dentist to advocate for additional restorative dentistry as well as manage the patient’s expectation of time required was essential. In addition, the patient needed to have realistic expectations of a compromised outcome. Both the restorative dentist and the periodontist informed the patient about the difficulty of achieving this with acceptable esthetic results. Mutual emotional and technical support was required to successfully complete this case, from initial grafting of the defect to placement of anterior restorations (Figure 14 through Figure 23).
Case 3: Managing Patient Expectations
A 46-year-old patient presented with a long-standing fixed partial denture replacing tooth No. 9 (Figure 24). The distal abutment No. 10 was fractured, and the patient was referred for implant reconstruction. During the consultation, the patient expressed a desire to have individual teeth back. Both the periodontist and the restorative dentist recommended a single fixture No. 9 with a cantilevered No. 10 pontic. Due to the bone loss present on the mesial aspect of tooth No. 9 and the bone loss present on the mesial aspect of tooth No. 10, this solution was felt to be the most predictable, using augmentation to build a pontic site for No. 10. Despite extensive consultation, due to the patient’s insistence on single teeth, expectations for an ideal result needed to be managed and the patient accepted therapy understanding that esthetics would most likely be compromised with little chance of complete regeneration (Figure 25 through Figure 33).
Conclusion
The take-home message is as follows:
- Hard-tissue failure frequently results in soft-tissue loss.
- Trephine removal of implants should be avoided.
- Short anterior cantilevered restorations may improve esthetic outcomes.
- Consideration of restorative dentistry on adjacent teeth and/or esthetic crown lengthening procedures may facilitate enhanced restorative results.
- The patient must be brought into the decision-making process and continually reminded of potential compromises.
- The periodontist and restorative dentist must work as a mutually supportive team.
References
1. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416.
2. Quirynen M, Naert I, van Steenberghe D, Nys L. A study of 589 consecutive implants supporting complete fixed prostheses. Part I: Periodontal aspects. J Prosthet Dent. 1992;68(4):655-663.
3. Browaeys H, Defrancq J, Dierens MC, et al. A retrospective analysis of early and immediately loaded Osseotite implants in cross-arch rehabilitations in edentulous maxillae and mandibles up to 7 years. Clin Implant Dent Relat Res. 2011 Jul 11. doi: 10.1111/j.1708-8208.2011.00367.x. [Epub ahead of print]
4. Babbush CA, Brokloff J. A single center retrospective analysis of 1001 consecutively placed NobelActive implants. Implant Dent. 2012;21(1):28-35.
5. den Hartog L, Slater JJ, Vissink A, et al. Treatment outcomes of immediate, early and conventional single tooth implants in the esthetic zone: a systematic review to survival, bone level, soft tissue, aesthetics, and patient satisfaction. J Clin Periodontal. 2008;35(12):1073-1086.
6. el Askary AS. Multifaceted aspects of implant esthetics: the anterior maxilla. Implant Dent. 2001;10(3):182-191.
7. Chen ST, Wilson TG, Hammerle CH. Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004:19(Suppl):12-15.
8. Esposito MA, Koukoulopoulou A, Coulthard P, Worthington HV. Interventions for replacing missing teeth: dental implants in fresh extraction sockets (immediate, immediate-delayed, delayed implants). Cochrane Database Syst Rev. 2006;18(4):CD005968.
9. Koldsland OC, Scheie AA, Aass AM. Prevalence of peri-implantitis related to severity of the disease with different degrees of bone loss. J Periodontol. 2010;81(2):231-238.
10. Karoussis IK, Kotsovilis S, Fourmousis I. A comprehensive review of dental implant prognosis in periodontally compromised partially edentulous patients. Clin Oral Implants Res. 2007; 18(6):669-679.
11. Heasman P, Esail Z, Barclay C. Peri-implant diseases. Dent Update. 2010;37(8):511-512, 514-516.
12. Liddelow G, Klineberg I. Patient-related risk factors for implant therapy. A critique of pertinent literature. Aust Dent J. 2011;56(4):417-426; quiz 441.
13. Weiner AA, Stark PC, Lasalvia J, et al. Fears and concerns of individuals contemplating esthetic restorative dentistry. Compend Contin Educ Dent. 2010;31(6):446-448.
14. Dewi FD, Sudjana G, Oesman YM. Patient satisfaction analysis on service quality of dental health care based on empathy and responsiveness. Dent Res J (Isfahan). 2010;8(4):172-177.
15. Zetu L, Wang HL. Management of the inter-dental/inter-implant papilla. J Clin Periodontal. 2005;32(7):831-839.
16. Chow YC, Wang HL. Factors and techniques in influencing peri-implant papillae. Implant Dent. 2010;19(3):208-219.
17. Ishikawa T, Salama M, Funato A, et al. Three-dimensional bone and soft tissue requirements for optimizing esthetic results in compromised cases with multiple implants. Int J Periodontics Restorative Dent. 2010;30(5):503-511.
18. Nevins M, Mellonig JT, Clem DS III, et al. Implants in regenerated bone: long term survival. Int J Periodontics Restorative Dent. 1998;18(1):34-39.
19. Levi A, Psoter WJ, Agar JR, et al. Patient self-reported satisfaction with maxillary anterior dental implant treatment. Int J Oral Maxillofac Implants. 2003;18(1):113-120.
20. Leblebicioglu B, Rawal S, Mariotti A. A review of the functional and esthetic requirements for dental implants. J Am Dent Assoc. 2007;138(3):321-329.
21. Fu JH, Lee A, Wang HL. Influence of tissue biotype on implant esthetics. Int J Oral Maxillofac Implants. 2011;26(3):499-508.
22. Levin BP. Immediate temporization of immediate implants in the esthetic zone: evaluating survival and bone maintenance. Compend Contin Educ Dent. 2011;32(4):52-60.
23. Levine RA, Nack G. Team treatment planning for the replacement of esthetic zone teeth with dental implants. Compend Contin Edu Dent. 2011;32(4):44-50.
24. Kan JY, Rungcharassaeng K, Lozada JL, Zimmerman G. Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants. A 2 to 8 year follow-up. Int J Oral Maxillofac Implants. 2011;26(1):179-187.
25. Lodding DW. Long term esthetic provisional restorations in dentistry. Curr Opin Cosmet Dent. 1997;4:16-21.
26. Bilhan H, Geckili O, Mumcu E. The use of definitive implant abutments for the fabrication of provisional crowns: a case series. J Periodontal Implant Sci. 2011;41(5):248-252.
27. Lang NP, Berglundh T; Working Group 4 of Seventh European Workshop on Periodontology. Periimplant diseases: where are we now?—Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontal. 2011;38 Suppl 11:178-181.
28. Pye AD, Lockhart DE, Dawson MP, et al. A review of dental implants and infection. J Hosp Infect. 2009;72(2):104-110.
29. Rutar A, Lang NP, Buser D, et al. Retrospective assessment of clinical and microbiological factors affecting periimplant tissue conditions. Clin Oral Implants Res. 2001;12(3):189-195.
30. Albouy JP, Abrahamsson I, Persson LG, Berglundh T. Implant surface characteristics influence the outcome of treatment of peri-implantitis: an experimental study in dogs. J Clin Periodontal. 2011;38(1):58-64.
31. Heitz-Mayfield LJ, Lang NP. Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis. Periodontal 2000. 2010;53:167-181.
32. Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontol. 2008;35(8 suppl):286-291.
33. Máximo MB, de Mendonça AC, Alves JF, et al. Peri-implant diseases may be associated with increased time loading and generalized periodontal bone loss: preliminary results. J Oral Implantol. 2008;34(5):268-273.
34. Máximo MB, de Mendonça AC, Renata Santos V, et al. Short-term clinical and microbiological evaluations of peri-implant diseases before and after mechanical anti-infective therapies. Clin Oral Implants Res. 2009;20(1):99-108.
35. Roos-Jansåker AM, Renvert H, Lindahl C, Renvert S. Submerged healing following surgical treatment of peri-implantitis: a case series. J Clin Periodontol. 2007;34(8):723-727.
About the Authors
Donald S. Clem, DDS
Private Practice
Fullerton, California
George R. Perri, DDS
Private Practice
Whittier, California