You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
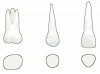
Initially, titanium root form implants, introduced to the United States by Dr. Per-Ingvar Brånemark, were not intended for fabricating partially edentulous restorations. They were designed strictly for restoring the edentulous mandible.1 However, as implant dentistry evolved from a specialized discipline to mainstream application, demand for fixed prosthodontic restorations for the partially edentulous patient increased. The stock abutments designed for chairside use are less than ideal for the restoration of molars in particular, and in many cases, the same holds true for maxillary central incisors and canines (Figure 1). A fixture matching 4 mm diameter is too small to provide proper sulcus development for teeth with larger diameters. It is important to remember that the anatomy of natural teeth is not cylindrical, as the implant is shaped, but rather somewhat triangular or rectangular. Consulting with Wheeler´s Dental Anatomy, Physiology and Occlusion (Figure 2) can help remind both technicians and clinicians of the basic differences between implant design and tooth anatomy.2
Laboratory Fabricated Custom Abutments
The dental implant field evolved quickly, and in 1988, Implant Innovations founder Dr. Richard Lazzarra introduced the UCLA abutment for custom cast fixed prosthodontic abutment development. This new design allowed the technician to wax and cast an anatomically correct emergence profile from the 4 mm implant abutment interface to the marginal level of the intended restoration.3
Prior to the availability of zirconia abutments, technician ingenuity led to the cutting back of the labial margin of the cast UCLA abutment and firing opaque and dentine ceramic materials to provide a “porcelain shoulder” to satisfy the esthetic requirements of patients with a thin gingival biotype. The corresponding PFM also had a matching porcelain shoulder.
Zirconia Abutments
Soon other materials started to find their way into implantology. The introduction of the first “stock” 4 mm preppable zirconia abutment from Nobel Biocare provided laboratory technicians with the opportunity to deliver improved esthetics and clinical performance (Figure 3). While the innovation provided better esthetics, it still did not address the need for ideal biologic contours at the restoration/abutment interface.
Technological Impact
Although CAD/CAM technology has had a significant impact on restorative dentistry, nowhere has the technology had greater effect than on implant restorations. The introduction of the first CAD/CAM developed implant abutment from Implant Innovations in 2004 proved to be a tremendous asset in meeting the challenges presented by less than ideal placement of implants.
Initially available only in titanium, these abutments allowed the development of ideal biologic contours at the abutment/restoration interface (Figure 4).
The evolution of esthetic restorative material development continued, and soon zirconia began to deliver as a high strength restorative material. Ultimately, this material proved to be ideal in meeting the need for esthetic implant abutments supporting all-ceramic restorations in the esthetic zone (Figure 5).
The Procera® system from Nobel Biocare gave dentistry its first technician-designed zirconia abutment. The technology is referred to as the “copy mill” technique, and the procedure required a wax up to develop the ideal abutment contours. The pattern would be scanned with a Procera digital contact scanner, and the resulting file would be sent by modem transfer to the Procera centralized production facility for fabrication. Upon completion, the abutment was returned to the laboratory for final adjustment and crown fabrication.
The continued development of software-driven technology has brought about major improvements in abutment fabrication processes. The more recent systems provide a remarkable level of sophistication insofar as design considerations are concerned. One example of such technology would be DENTSPLY Implant’s ATLANTIS™ VAD Technology, which automatically examines a comprehensive list of considerations when designing a patient-specific abutment.
Scanners and their software are designed to be compatible with specific fabrication technologies. These technologies give the technician the choice between sending a simple digital scan file to an outside laboratory for processing, and designing the abutment themselves (Figure 6) and sending a final design for completion. Direct laboratory digital scanning of casts with the appropriate scan body in the master cast is a significant time saver.
Concurrent Manufacturing
Concurrent manufacturing is a revolutionary concept in dentistry and is currently available in a number of digital impression systems. The first available application of concurrent manufacturing for implant abutments was found in ATLANTIS abutment core file technology (Figure 7), in which a high precision, digital file of an ATLANTIS abutment could be used for designing a coping before receipt of the final abutment. This allows for shorter working time and optimum accuracy. Developing the restoration digitally in the laboratory while the abutment is being completed offers laboratories and clinicians significant time-savings. The improved accuracy is accomplished by use of the digital abutment file rather than scanning a completed abutment, thus eliminating one round of data acquisition and transfer.
CAD/CAM Versus Hand Fabrication
There are many differences between CAD/CAM and hand-fabricated abutments, but the cost and the quality of the abutments are two of the most important factors technicians should be cognizant of when choosing between the two.
Cost
The fees associated with hand-fabricated abutment include the cost of noble alloy, manufacturer’s components, and highly skilled technical labor. By comparison, when fabricating crowns over stock abutments, there are associated increases in alloy cost of the corresponding PFM due to necessary buildup of copings to accomplish ideal porcelain support. When these costs are compared to CAD/CAM abutments, the fees are typically very closely matched.
Quality
There are two potential issues technicians must be aware of when using crowns over stock abutments. First, the lack of uniformity in coping thickness can create thermal stresses at the coping/ceramic interface. This can be attributed to to inconsistent cooling time associated with thicker versus thinner areas in the coping. Second, the basic techniques of waxing and casting a precious metal abutment involve placing the invested pattern in a burnout oven, which can result in inaccuracies at the interface when compared to milled titanium fabrication methods.
In the case of a plastic UCLA pattern, the replacement of the pattern with cast alloy gives us the first dimensional compromise. The necessity of finishing, sand blasting, and polishing the interface results in the second potential compromise in adaptation.
In the case of a higher quality, more costly manufactured high noble abutment designed for the wax and cast technique, similar limitations also exist. The burnout leads to oxidation of the milled component interface. Removing the oxide layer creates a dimensional compromise.
Conclusion
It has been a long road for the evolution of implant abutments. From Dr. Per-Ingvar Brånemark’s titanium root form implants to the latest technological advances in CAD/CAM technology, the end goal has always been to produce the highest-quality final product for clinicians and their patients. When all factors are considered, and new technologies taken into account, CAD/CAM manufacturing of implant abutments is the obvious choice above all others. The precision and biocompatibility of a highly detailed, anatomically correct milled titanium or zirconia component allows technicians to offer the absolute optimum treatment for today’s implant patient.
References
1. Brånemark PI, Breine U, Adell R, et al. Intra-Osseous Anchorage of Dental Prostheses:I. Experimental Studies. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery. 1969;3(2):81-100.
2. Nelson SJ. Wheeler´s Dental Anatomy, Physiology and Occlusion. Philadelphia, PA: Saunders;2009.
3. Lewis SG, Llamas D, Avera S. The UCLA abutment: a four-year review. J Prosthet Dent. 1992;67(4):509-515.
About the Author
Mark Stueck, CDT
Manager, Crown and Bridge
Drake Dental Laboratory
Charlotte, NC