You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Esthetic and restorative dentistry aims to replace lost or damaged structures with artificial materials that possess biological, physical, and functional properties similar to natural teeth.1 Among these materials, composite resins occupy a paramount position because they offer excellent esthetic potential and acceptable longevity without the need for extensive sound structure preparation, allowing minimally invasive preparation or sometimes no preparation at all.2 Numerous composite systems have been developed in recent years with a multitude of shades, translucencies, opacities, and effects that, together with innovative placement techniques, make the fabrication of restorations that faithfully emulate the polychromatic variations and optical characteristics present in natural teeth possible.3-5 This conceptual evolution in materials and techniques gives clinicians the option to treat a large range of problems faced in everyday practice in a reliable, predictable, and conservative way. Because direct composite restorations are now a more integral part of restorative procedures, to provide improved patient care dentists should have an in-depth knowledge regarding the properties, indications of use, and clinical performance of these materials.
COMPOSITE RESIN FORMULATIONS
Composite resins are basically a mixture of an organic resin matrix, inorganic filler particles, and a coupling agent. The resin matrix consists of monomers, initiator systems, stabilizers, and pigments, while the inorganic filler consists of some form of glass filler particles. Although there are variations of the specific composition and distribution of the matrix and filler phases in every commercial composite resin, most composites are fabricated using either bisphenol-A-diglycidylmethacrylate (bis-GMA) or urethane dimethacrylate (UDMA) matrix polymers and different kinds of filler particles, such as glass, quartz, and colloidal silica.6 The matrix and the filler are the components that dictate most of the material’s mechanical properties (ie, fracture toughness and elastic modulus), as well as physical properties (ie, polishability and optical characteristics). Also, the relationship between the resin matrix and the filler’s particle size and loading defines the different types of composite resins available today.
CLASSIFICATION OF COMPOSITE RESINS
Composite resins have been classified according to various characteristics (ie, curing mechanism and particle type); however, the most commonly used classification considers mainly the distribution and average particle size of a given composite’s filler phase.7 Even though macrofilled composite resins are still available on the market, their use is very restricted because their limited properties lead to less than optimal clinical performance (ie, roughness, staining, wear, and discoloration). Most composite resins can be classified in two main categories: microfilled and hybrid composites.
Microfilled Composite Resins
These composites were introduced in the early 1980s. They are generally filled 35% to 50% by weight with prepolymerized 0.02-µm to 0.04-µm silicon dioxide filler particles. The main characteristics of these composites are the high polish that can be achieved and maintained over time and excellent enamel-like translucency. Therefore, they are indicated for the restoration of anterior teeth and cervical abfraction lesions; they should not be used in heavy stress-bearing areas because they frequently exhibit marginal chipping and bulk fracture.7
In general, their physical properties are inferior to those of hybrid composites because of their lower percentage of filler content; the exception is their compressive strength, which can be relatively high. Microfilled composites have higher coefficients of thermal expansion, greater water sorption, greater polymerization shrinkage, lower module of elasticity, lower tensile strength, and lower fracture toughness.6
Clinical evaluations comparing anterior restorations produced with microfills and hybrid composite resins have demonstrated that hybrid composites present a significantly better performance with regard to marginal integrity, color, and marginal discoloration.8,9 Some reinforced microfill composite resins are also available and are indicated for use in posterior teeth. Good clinical results have been reported with these composites.10
With the trend toward simplification, together with the search for “universal” materials and the evolution of hybrid materials, the use of microfilled composites will become more restricted.
Hybrid Composite Resins
Hybrid composite resins contain a heterogeneous aggregate of filler particles. They are usually filled 70% to 80% by weight with 0.04-µm and 1-µm to 5-µm filler particles. The average particle size of hybrid composites is usually > 1 µm. This mixture of fillers accounts for their excellent physical properties with high polishability when compared to the earlier macrofilled composites. Regrettably, one problem with hybrid composite resins is their inability to maintain their gloss.11
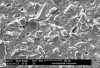
Given the need for a highly polishable composite resin with optimal physical properties for use in the anterior and posterior regions, manufacturers developed microhybrid composite resins. They reduced the particle size, ranging from 0.04 µm to 1 µm (Figure 1). By incorporating smaller particles, microhybrid composites polish and handle better than their hybrid counterparts. Microhybrid composites are stronger than most microfilled composites and can be used in both anterior and posterior teeth. Therefore, microhybrid composites can be used as universal or all-purpose composite resins.7
Although these materials can be used with basic shades, many of these new composites also have a complete set of incisal, enamel, dentin, and effect shades so they can be built using a stratification technique for a more toothlike appearance (Figure 2 through Figure 4). A number of manufacturers include specialized shade guides and recipes to help the clinician choose the best mix of shades to use in specific circumstances.
Regarding consistency, the great majority of microhybrid composite resins present medium viscosity; however, some other types of composite resins can be classified as high-viscosity (“packable” composites) or low-viscosity (“flowable” composites) (Figure 5). High-viscosity composite resins (also known as “condensable” or “heavy-body”), possess a greater amount of load (above of 80% in volume), which makes them more resistant and easier to apply because of their excellent sculptability. The use of these composite resins is especially indicated for the reestablishment of the contour and proximal contacts in class 2 restorations and for the precise definition of occlusal anatomy features.11 As the clinical performance of these composites is similar to that of regular-viscosity microhybrid composites, the selection of this type of material must be based on individual preferences.12
On the other hand, flowable composite resins present much less load (about 50% in volume), possess inferior mechanical properties, and present a greater degree of polymerization shrinkage.13 Recent studies have demonstrated that the use of flowable composites does not improve the marginal sealing of adhesive restorations;14,15 however, its use is indicated in areas of difficult access and irregular cavity preparations because it favors the insertion and adaptation of the subsequent increments.16 These composite resins are also useful in the restoration of highly conservative preparations such as placing preventive resin restorations, repairing margins of existing composite resin restorations, surfacing fiber splints, repairing bis-Acryl composite provisional restoration margins, luting porcelain veneers, and placing temporary pedodontic restorations.11,17 Some manufacturers have developed flowable composites that are part of a family of composites with their esthetic microhybrid composites.
Nanofilled Composite Resins
Nanofilled composites were recently introduced and they consist of nanomers (5 nm to 75 nm particles) and “nanocluster” agglomerates as the fillers. Nanoclusters are agglomerates (0.6 µm to 1.4 µm) of primary zirconia/silica nanoparticles (5 nm to 20 nm in size) fused together at points of contact. The resulting porous structure is infiltrated with silane.18 The nanofilled composites present similar mechanical and physical properties to those of microhybrid composites, but when it comes to polish and gloss retention they perform significantly better.19 Several manufacturers are now incorporating nano-sized particles into their formulations, resulting in the creation of yet another category, the “nanohybrid” composites.
Click here to view a case study.CONCLUSION
The evolution in the development and improvements with composite resins has changed the way dentists practice restorative dentistry. Currently, the new generations of composite resins offer excellent performance materials for anterior and posterior direct placement restorations. When selecting composite resins, the criteria should include highly esthetic shade matching, translucency, and fluorescence; high polishability; excellent mechanical properties that contribute to restoration durability; good handling properties; excellent wear resistance; radiopacity; low polymerization shrinkage; and biocompatibility. The criteria for future development and introduction of new composite resins point to the progression to one universal composite.20 This is a difficult challenge to manufacturer and clinician alike. To date, in general, the microhybrid and nanofilled composites offer an alternative to microfilled composites in their ability to be highly polishable with toothlike translucency. This class of composites would be considered universal-use composite resins. Clinicians can expect excellent mechanical properties, excellent esthetics with shade selection, good color stability, stain resistance, low wear, and good polishability when using these composites.11
REFERENCES
1. Chu SJ, Ahmad I. Light dynamic properties of a synthetic, low-fusing, quartz glass-ceramic material. Pract Proced Aesthet Dent. 2003;15(1):49-56.
2. Dietschi D, Ardu S, Krejci I. A new shading concept based on natural tooth color applied to direct composite restorations. Quintessence Int. 2006;37(2):91-102.
3. Baratieri LN, Araujo Jr EM, Monteiro Jr S. Composite Restorations in Anterior Teeth: Fundamentals and Possibilities. Hanover Park, IL; Quintessence Publishing: 2005.
4. Sensi LG, Marson FC, Roesner, TH, et al. Fluorescence of composite resins: clinical considerations. Quintessence Dent Technol. 2006;29:43-53.
5. Sensi LG, Araujo FO, Marson FC, et al. Reproduction of opalescence and counter-opalescence with composite resins. Quintessence Dent Technol. 2007;30:77-86.
6. Ferracane JL. Current trends in dental composites. Crit Rev Oral Biol Med. 1995;6(4):302-318.
7. Ritter AV. Direct resin-based composites: current recommendations for optimal clinical results. Compend Contin Educ Dent. 2005;26(7):481-490.
8. Reusens B, D’hoore W, Vreven J. In vivo comparison of a microfilled and a hybrid minifilled composite resin in Class III restorations: 2-year follow-up. Clin Oral Investig. 1999;3(2):62-69.
9. Geitel B, Kwiatkowski R, Zimmer S, et al. Clinically controlled study on the quality of class III, IV and V composite restorations after two years. J Adhes Dent. 2004;6(3):247-253.
10. Rasmusson CG, Lundin SA. Class II restorations in six different posterior composite resins: five-year results. Swed Dent J. 1995;19(5):173-182.
11. Strassler HE. Product advances with direct-placement composite resins: Current state-of-the-art. Contemp Esthet. 2006;10(2):16-19.
12. Loguercio AD, Reis A, Hernandez PA, et al. 3-year clinical evaluation of posterior packable composite resin restorations. J Oral Rehabil. 2006;33(2):144-151.
13. Labella R, Lambrechts P, Van Meerbeek B, et al. Polymerization shrinkage and elasticity of flowable composites and filled adhesives. Dent Mater. 1999;15(2):128-137.
14. Lindberg A, van Dijken JW, Horstedt P. In vivo interfacial adaptation of class II resin composite restorations with and without a flowable resin composite liner. Clin Oral Investig. 2005;9(2):77-83.
15. Baratieri LN, Canabarro S, Lopes GC, et al. Effect of resin viscosity and enamel beveling on the clinical performance of Class V composite restorations: three-year results. Oper Dent. 2003;28(5):482-487.
16. Fortin D, Vargas MA. The spectrum of composites: new techniques and materials. J Am Dent Assoc. 2000;131(Suppl):26S-30S.
17. Andersson-Wenckert I, Sunnegardh-Gronberg K. Flowable resin composite as a class II restorative in primary molars: A two-year clinical evaluation. Acta Odontol Scand. 2006;64(6):334-340.
18. Hervas-Garcia A, Martinez-Lozano MA, Cabanes-Vila J, et al. Composite resins. A review of the materials and clinical indications. Med Oral Patol Oral Cir Bucal. 2006;11(2):E215-E220.
19. Mitra SB, Wu D, Holmes BN. An application of nanotechnology in advanced dental materials. J Am Dent Assoc. 2003;134(10):1382-1390.
20. Roeters JJ, Shortall AC, Opdam NJ. Can a single composite resin serve all purposes? Br Dent J. 2005;199(2):73-79.
About the Authors
Luis Guilherme Sensi, DDS, MS, PhD
Assistant Professor
Department of Endodontics, Prosthodontics and Operative Dentistry
University of Maryland Dental School
Baltimore, Maryland
Howard E. Strassler, DMD
Professor and Director of Operative Dentistry
Department of Endodontics, Prosthodontics and Operative Dentistry
University of Maryland Dental School
Baltimore, Maryland
William Webley
Undergraduate Dental Student
University of Maryland Dental School
Baltimore, Maryland
Robert C. Margeas, DDS
Adjunct Professor
Department of Operative Dentistry
University of Iowa College of Dentistry
Iowa City, Iowa
Private Practice
Des Moines, Iowa