You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Photobiomodulation (PBM) is a form of light therapy that uses nonionizing light sources, including lasers, light emitting diode (LED) devices, and broad-spectrum lamps, to deliver light energy in the visible and near-infrared (NIR) portion of the electromagnetic spectrum with wavelengths between 400 nm and 1400 nm. These devices range in size from small probes, which are only a few millimeters in diameter and can be placed intraorally, to whole body devices, which resemble tanning beds. PBM is a nonthermal process involving endogenous chromophores (absorbers of light) that elicit photophysical and photochemical events at various biologic scales.1 PBM processes result in beneficial therapeutic outcomes that include but are not limited to the alleviation of pain or inflammation, the facilitation of immunomodulation, and the promotion of wound healing and tissue regeneration.2 Simply stated, PBM is the use of a nonionizing source of photonic energy to generate nonthermal therapeutic effects.1
Preferred Terminology
The term photobiomodulation is a combination of the Greek root words "photo," which means "light," and "bios," which means "life," with the word "modulation," which means to stimulate or inhibit a response. The term was derived at a 2014 workshop held by the North American Association for PhotobiomoduLation Therapy (NAALT) and the World Association for PhotobiomoduLation Therapy (WALT) to assist in the standardization of the terminology. Previously, PBM was referred to by a variety of terms, including photostimulation, low level laser (or light) therapy (LLLT), phototherapy, photomedicine, biostimulation, and more. In 2015, the National Library of Medicine added photobiomodulation to its Medical Subject Headings thesaurus to encompass all of the terms that had been used in the past.
Because PBM is playing an ever-increasing role in patient care in both dentistry and medical care, using the abbreviation PBM for photobiomodulation therapy helps to avoid confusion with the medical abbreviation PBMT, which is already used for the terms "post bone marrow transplant" and "perioperative blood management technologist."
PBM Basics
The late Endre Mester, MD, DSc, is considered to be the father of PBM. In 1967, at Semmelweis Medical University in Budapest, Mester observed how low dose laser energy had a biologic effect on the stimulation of wound healing and hair growth in a process that he termed "photostimulation."
A familiar form of basic PBM that occurs naturally is the process by which sunlight stimulates the production of Vitamin D3. Among other cellular responses, PBM can be used to control inflammation, manage edema, enhance tissue healing, reduce pain, and improve tissue and muscle performance. Due to its biphasic response, PBM can also produce an analgesic effect.
In pharmacology, chemical energy is introduced into the body to stimulate a biologic/biochemical response. This response is dependent on the type of medicine administered as well as the dosage and the intervals at which it is administered. Similarly, PBM involves introducing light energy into the body to stimulate a biologic/photochemical response that is dependent on the source of the energy being administered (eg, laser, LED, broad-spectrum lamp), the wavelength of light energy used, the dosage/amount of light energy used, and the duration of time and interval at which it is administered.
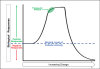
As the light energy from PBM enters the tissue being treated, it can be transmitted, scattered, reflexed, or most importantly, absorbed. Low levels of light energy penetrate into tissues where they interact with and are absorbed by endogenous chromophores located in cells, resulting in nondestructive photophysical and photochemical changes that lead to alterations at the molecular, cellular, and tissue levels of the body. Due to the biphasic nature of light absorption by tissue, depending on the dosage, PBM can either stimulate or inhibit a biologic response in a manner that is often described using the Arndt-Schultz law (Figure 1).3,4
Although PBM is similar in nature to photodynamic therapy (PDT), the nonablative use of light energy with PBM should not be confused with PDT, which uses exogenous chromophores and photosensitizers (nontoxic dyes) that are activated by light to accomplish the disinfection and cellular destruction of unwanted biologic structures.5
Proper Application
A primary concern with all forms of light therapy is the ability of the energy to penetrate the tissue and be absorbed by the desired target. Fortunately for dentists, the anatomy of the oral cavity and the head and neck provide an almost ideal environment for PBM therapy. The depth of penetration achieved by light energy is determined by the source (eg, laser, LED, broad-spectrum lamp), the wavelengths of the light, and the power used. Due to the organization and coherence of laser light, many researchers believe it has the ability to provide the deepest penetration at the same power density (W/cm2) when compared with other light sources, such as LED and broad-spectrum lamps.
When properly used, PBM has been shown to be a safe treatment modality that does not result in adverse effects.6 Realizing the true value of PBM requires a comprehensive understanding of the physics of light interaction, the tissue's condition and composition, and the biologic processes that enable the desired outcomes to be obtained. With the appropriate devices and protocols, practitioners can promote positive processes such as enhanced healing and tissue regeneration as well as inhibit the negative processes of pain and inflammation.
Empirical Evidence
PBM's ability to assist in controlling inflammation and edema leads to a reduction in pain while enhancing tissue repair, which makes it an ideal adjunctive therapy that can be administered both pre- and postoperatively for many routine oral procedures (Table 1). Today, the use of PBM is strongly recommended to assist in the prevention and management of oral mucositis in cancer patients,7,8 and it has even been shown to assist in alleviating tissue fibroses associated with graft-versus-host disease.9-11
The use of PBM has been shown to reduce pain in patients undergoing surgical procedures, extractions,6 and endodontic therapy.12 Regarding periodontal and implant surgery, research has demonstrated that PBM can positively affect the stimulation of healing in periodontal soft and hard tissues and reduce inflammation.13,14 In addition, PBM shows promise in being able to reduce the discomfort, duration, and severity of some viral outbreaks.15 Studies have indicated that PBM irradiation promotes the responses of dental pulp cells that are relevant to tissue repair, accelerating the recovery of the dental structures involved in cavity preparation in the predentin region and eliciting intentional tertiary dentin formation in the dental pulp.16-18 Furthermore, evidence suggests that laser light with controlled parameters can be effective in the treatment of tooth hypersensitivity.12,19,20
Due to PBM's effect on biologic processes, especially inflammation, it is considered an effective adjunctive treatment modality for patients with trismus and temporomandibular joint disorder (TMD). In TMD patients, PBM has been shown to reduce pain and contribute to functional enhancement.21 The various parameters and protocols that have been reported in the literature are often related to the underlying cause of the TMD and the specific PBM device being utilized, which has made the standardization of PBM therapy for TMD complicated.
PBM's ability to accelerate and enhance the healing of biologic tissue can be valuable in the recovery of the inferior alveolar nerve after traumatic injury during the removal of impacted third molars. PBM has been shown to be beneficial and advantageous as a noninvasive treatment to help reduce longstanding sensory nerve impairment following third molar surgery.22 In one study, the ability of patients to identify the direction of movement of a brush stroke stimulus was dramatically improved over time with PBM. When the neurosensory assessment scores after treatment with PBM were compared with the baseline values prior to treatment, progressive improvement was evident, signifying the return of neurosensory functions.23
Mechanisms of Action
PBM's mechanisms of action have been identified through extensive research, including more than 40 years of laboratory experiments and controlled trials using lasers of minimal power and other sources of light energy. Presently, there have been more than 9,000 academic papers published and more than 900 randomized controlled trials performed in the area of PBM, and research is ongoing with many more studies being published on a monthly basis.
During PBM, the primary target for absorbing the light energy is the cytochrome complex. Cytochrome c oxidase (CcO) is a heme protein that is localized in the compartment between the inner and outer mitochondrial membranes of a cell.24 CcO is a critical component of the electron transfer mechanism that drives cellular metabolism. As the light energy is absorbed and the mitochondria is energized, CcO stimulates the production of adenosine triphosphate (ATP), which is the molecule that facilitates energy transfer within a cell.25
In addition, the absorption of light energy also produces free nitric oxide (NO) and reactive oxygen species (ROS). NO is a powerful vasodilator and an important cellular signaling molecule involved in many physiologic processes. NO signaling drives vasodilation, which improves microcirculation in the damaged tissue, delivering oxygen, vital sugars, proteins, and salts while removing waste. ROS have been shown to affect many important physiologic signaling pathways, including the inflammatory response. In concert, the production of NO and the production of ROS have been shown to induce growth factor production, to increase cell proliferation and motility, and to promote extracellular matrix deposition and pro-survival pathways outside the cell.1
In stressed or ischemic tissue, CcO produces NO in the mitochondria, which displaces oxygen and reduces the production of ATP. Furthermore, there is an excessive production of ROS, which increases the oxidative stress in the tissue, leading to inflammation. In such stressed tissues, CcO absorbs the light energy from PBM and uses that energy to displace the NO.1
At the cellular level of stressed tissue, an excessive amount of ROS overstimulates nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), which causes the gene transcription associated with inflammation and cell survival. PBM reduces ROS by reducing NF-κB stimulation and related inflammation and has positive effects on cells that are important for tissue regeneration and the autoimmune response, including neutrophils, macrophages, fibroblasts, mast cells, endothelial cells, keratinocytes, lymphocytes, and odontoblasts.1
Beyond the direct effects of the light energy used in PBM, the therapy also produces a positive extracellular "bystander effect" in neighboring cells that do not receive the light energy because they absorb the secretions from the stimulated cells. These secretions can enter the bloodstream and lymphatic system and affect the body in regions far away from the treated areas, promoting healing and function while reducing inflammation and pain.
Side Effects and Contraindications
If PBM is administered with the appropriate dosages and proper protocols, there are no known side effects. However, with inappropriate use of PBM devices, there is a risk of thermal damage to the irradiated structures both on the surface of the tissue and deeper within.26 In addition, as with all light-based technologies, there is a concern for the potential for ocular damage, and the necessary precautions should be closely adhered to. Some patients, especially those taking certain medications, may be more sensitive to light exposures; therefore, the use of lower exposures or delayed treatment should be considered. There are no known mutagenic or cancer risks associated with PBM therapy that uses light energy in the visible and NIR ranges.27 However, when providing PBM to a patient who is being treated for cancer, it is strongly recommended to have a medical consult with his or her oncologist.
Conclusion
Today, with the appropriate PBM devices and protocols, clinicians have the ability to efficiently deliver effective doses of light deep into tissues to accelerate healing and enhance treatment outcomes, reduce inflammation and pain, and achieve other beneficial results. To obtain the desired effects of PBM, it is imperative that clinicians have clear objectives and goals for treatment, a comprehensive understanding of laser/light physics, and knowledge regarding the location and composition of the target tissue (Table 2). Clinicians should also be properly trained in the techniques and protocols specific to the devices used as well as understand the benefits and limitation of the technologies.
Queries regarding this course may be submitted to authorqueries@aegiscomm.com
About the Author
John A. Cianciola, DDS, MSD
Clinical Assistant Professor
Midwestern University
College of Dental Medicine
Glendale, Arizona
Private Practice
Scottsdale, Arizona
Scott D. Benjamin, DDS
Associate Professor of Clinical Dentistry
Eastman Institute for Oral Health
University of Rochester Medical Center
Rochester, New York
Private Practice
Sidney, New York
References
1. Khan I, Arany P. Biophysical approaches for oral wound healing: emphasis on photobiomodulation. Adv Wound Care (New Rochelle). 2015;4(12):724-737.
2. Anders JJ, Lanzafame RJ, Arany PR. Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg. 2015;33(4):183-184.
3. Anders JJ. Photobiomodulation. American Society for Laser Medicine & Surgery website. http://www.aslms.org/for-the-public/treatments-using-lasers-and-energy-based-devices/
photobiomodulation. Updated June 27, 2016. Accessed May 27, 2022.
4. Huang YY, Chen ACH, Carroll JD, Hamblin MR. Biphasic dose response in low level light therapy. Dose Response. 2009;7(4):358-383.
5. Benov L. Photodynamic therapy: current status and future directions. Med Princ Pract. 2014;24(suppl 1):14-28.
6. Pergolini D, Del Vecchio A, Palaia G, et al. Photobiomodulation after surgical extraction of the lower third molars: a narrative review. Oral. 2022;2(1):18-28.
7. Zadik Y, Arany PR, Fregnani ER, et al. Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. 2019;27(10):3969-3983.
8. Courtois E, Bouleftour W, Guy JB, et al. Mechanisms of photobiomodulation (PBM) focused on oral mucositis prevention and treatment: a scoping review. BMC Oral Health. 2021;21(1):220.
9. Epstein JB, Raber-Durlacher JE, Huysmans MC, et al. Photobiomodulation therapy alleviates tissue fibroses associated with chronic graft-versus-host disease: two case reports and putative anti-fibrotic roles of TGF-β. Photomed Laser Surg. 2018;36(2):92-99.
10. Arany PR, Tuan T. Targeted approaches to scar management based on our current understanding of triggers, modulators, and effectors of aberrant healing. In: Sen CK, ed. Advances in Wound Care: Volume 2. Mary Ann Liebert, Inc. Publishers; 2010.
11. Tam M, Arany PR, Robijns J, et al. Photobiomodulation therapy to mitigate radiation fibrosis syndrome. Photobiomodul Photomed Laser Surg. 2020;38(6):355-363.
12. Vahdatinia F, Gholami L, Karkehabadi H, Fekrazad R. Photobiomodulation in endodontic, restorative, and prosthetic dentistry: a review of the literature. Photobiomodul Photomed Laser Surg. 2019;37(12):869-886.
13. Gholami L, Asefi S, Hooshyarfard A, et al. Photobiomodulation in periodontology and implant dentistry: part 1. Photobiomodul Photomed Laser Surg. 2019;37(12):739-765.
14. Gholami L, Asefi S, Hooshyarfard A, et al. Photobiomodulation in periodontology and implant dentistry: part 2. Photobiomodul Photomed Laser Surg. 2019;37(12):766-783.
15. Khalil M, Hamadah O. Association of photodynamic therapy and photobiomodulation as a promising treatment of herpes labialis: a systematic review. Photobiomodul Photomed Laser Surg. 2022;40(5):299-307.
16. Holder MJ, Milward MR, Palin WM. Effects of red light-emitting diode irradiation on dental pulp cells. J Dent Res. 2012;91(10):961-966.
17. Shigetani Y, Sasa N, Suzuki H, et al. GaAlAs laser irradiation induces active tertiary dentin formation after pulpal apoptosis and cell proliferation in rat molars. J Endod. 2011;37(8):1086-1091.
18. Godoy BM, Arana-Chavez VE, Núñez SC, Ribeiro MS. Effects of low-power red laser on dentine-pulp interface after cavity preparation. An ultrastructural study. Arch Oral Biol. 2007;52(9):899-903.
19. He S, Wang Y, Li X, Hu D. Effectiveness of laser therapy and topical desensitising agents in treating dentine hypersensitivity: a systematic review. J Oral Rehabil. 2011;38(5):348-538.
20. Blatz MB. Laser therapy may be better than topical desensitizing agents for treating dentin hypersensitivity. J Evid Based Dent Pract. 2012;12(3 Suppl):229-230.
21. Ayyildiz S, Emir F, Sahin C. Evaluation of low-level laser therapy in TMD patients. Case Rep Dent. 2015;2015:424213.
22. Qi W, Wang Y, Huang YY, et al. Photobiomodulation therapy for management of inferior alveolar nerve injury post-extraction of impacted lower third molars. Laser Dent Sci. 2020;4(1):25-32.
23. Ozen T, Orhan K, Gorur I, Ozturk A. Efficacy of low level laser therapy on neurosensory recovery after injury to the inferior alveolar nerve. Head Face Med. 2006;2:3.
24. Hough MA, Silkstone G, Worrall JAR, Wilson MT. Chapter 8: NO Binding to the Proapoptotic Cytochrome c-Cardiolipin Complex. In: Litwack G, ed. Nitric Oxide. Elsevier, 2014:193-210.
25. Knowles JR. Enzyme-catalyzed phosphoryl transfer reactions. Annu Rev Biochem. 1980;49:877-919.
26. Khan I, Tang E, Arany P. Molecular pathway of near-infrared laser phototoxicity involves ATF-4 orchestrated ER stress. Sci Rep. 2015;5:10581.
27. Brandão TB, Morais-Faria K, Ribeiro ACP, et al. Locally advanced oral squamous cell carcinoma patients treated with photobiomodulation for prevention of oral mucositis: retrospective outcomes and safety analyses. Support Care Cancer. 2018;26(7):2417-2423.