You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
While over the past few decades zirconia has become one of the most commonly used restorative materials, zirconia bonding remains a contentious topic. In a recent study of the National Dental Practice-Based Research Network Collaborative Group, only 30% of zirconia restorations were bonded with resin cement, whereas the remaining 70% were cemented with conventional glass-ionomer or resin-modified glass ionomer (RMGI) cement.1 Although cementation of zirconia restorations with RMGI cement is an acceptable clinical procedure, bonding zirconia with resin cement has a number of clinical advantages. This article will discuss the clinical situations in which zirconia bonding is indicated, the evidence for effectiveness in zirconia bonding, and the steps involved in the protocol for zirconia bonding.
CLINICAL APPLICATIONS FOR ZIRCONIA BONDING
Using zirconia as a bonding material has specific clinical applications and certain advantages over bonding with other restorative materials, making bonded zirconia preferable for some restorations. To successfully address these clinical situations, many clinicians have found it beneficial to understand how to bond zirconia.
Some clinicians prefer bonding to glass-based ceramics such as lithium disilicate, as this material may be bonded using a traditional process of hydrofluoric acid etching and silane application. However, using zirconia as a bonded restoration rather than glass-based materials has some clinical advantages. First, zirconia is stronger than lithium disilicate and therefore may be a material of choice for fixed partial dentures (FPD), as it will provide the highest strength at connectors.2 In cases where there is limited resistance or retention form of the abutment tooth preparations, bonding the zirconia FPD may be necessary. Another advantage of zirconia is that when there is limited occlusal clearance, bonded zirconia is stronger than RMGI-cemented zirconia or bonded lithium disilicate.3
Bonded zirconia may also be used for veneers on discolored tooth preparations. For full coverage crowns, opaque framework materials may be utilized to block out a discolored tooth preparation. Because of their relative thinness, veneers are usually fabricated from monolithic material. As zirconia is more opaque than glass ceramics yet sufficiently esthetic for some anterior restorations, a zirconia veneer may be useful for masking discoloration.4
CURRENT EVIDENCE FOR ZIRCONIA BONDING
Published reports have provided ample evidence that zirconia bonding is not merely possible, but provides a stable bond that is comparable to bonding to glass-based ceramics. The evidence for the effectiveness of zirconia bonding should be assessed from both preclinical (laboratory studies) and clinical trials. Although individual studies are critical for evidence-based assessments, systematic reviews and meta-analyses of published studies are more efficient sources for the evaluation of current evidence. A systematic review is a summary of all existing research on a topic that complies with predefined eligibility criteria, while a meta-analysis is an analysis of data from many independent studies for which the results are statistically similar. Several systematic reviews and meta-analyses have been performed to assess bonding to zirconia.
All of the systematic reviews of laboratory studies of zirconia bonding concluded that mechanical and chemical pretreatment can be used to obtain a durable bond to zirconia,5-10 while the implication of these findings is that the zirconia bond strength is greater than would be achieved without these pretreatments. The term physico-chemical bonding is used in some of these reviews, which implies that thev surface is "physically" roughened and a "chemical" bond is achieved through this procedure. The typical mechanical surface roughening procedure is air abrasion with alumina particles, and the chemical bonding to the zirconia surface is achieved with 10-methacryloyloxydecyl-dihydrogen-phosphate (10-MDP). Another procedure, referred to as "tribochemical" bonding, involves air abrading zirconia with silica-coated alumina particles, which deposits silica on the surface of the zirconia. A silane primer is then used to bond to the deposited silica.
Of the systematic reviews of laboratory studies, three included meta-analyses.5-7 Two of the meta-analyses compared different methods of achieving surface roughness and chemical bonding. Both analyses concluded that tribochemical bonding and alumina air-abrasion with MDP primer were effective in the short-term bonding tests (less than 2 months of storage in one study and less than 6 months of storage in the other). 6,7 The analyses showed that bonding with both of these pretreatments yielded better bond performance than when no pretreatment was used after long-term storage.6,7 The other meta-analysis reported that physico-chemical bonding resulted in greater bonding effectiveness than occurred with physical or chemical pretreatment alone. Additionally, the study showed that MDP present in a cement (rather than used as a separate primer) was also effective in improving the bond to zirconia.8
A systematic review of clinical trials assessing the bond to nonretentive zirconia restorations was performed for both posterior inlay-retained FPDs and anterior resin-bonded FPDs.11 These restoration designs were investigated because the preparations lack retention form and therefore the clinical success of the restorations would be dependent on the bond to zirconia. Three studies were included that examined posterior inlay-retained FPDs; the cumulative clinical survival rates were 100% at 20 months, 95.8% at 5 years, and 12.1% at 10 years. Five studies were included that examined anterior resin-bonded bridges, which had a 100% 3- to 10-year survival rate. In the five studies of anterior resin-bonded bridges, several debonds occurred that required the restorations to be rebonded. The rate of debonding ranged from 1/24 restorations (in a 3-year study), 2/30 restorations (in a 5-year study), 2/42 restorations (in a 6-year study), 2/15 restorations (in an 8-year study), to 6/108 restorations (in a 10-year study).11
A recent narrative review of bonding to high-strength ceramics summarized the few clinical studies that examined bonding to zirconia crowns.12 A retrospective practice-based study of 126 mostly posterior zirconia crowns reported that only 6.6% experienced any crown loosening after 5 years. Another study of 20 porcelain-fused-to-zirconia crowns showed no loss of retention after 5 years.12
Systematic reviews of laboratory and clinical trials indicate that both physical and chemical pretreatments of zirconia improve bonding of zirconia to resin cement. Surprisingly, there are no reviews comparing the bond strength to zirconia with the bond strength to lithium disilicate. Some laboratory testing has shown lithium disilicate and zirconia to have an equivalent bond strength, with bond strength decreased for both materials after 150 days of water storage.13
PROTOCOL FOR ZIRCONIA BONDING
Best practices for successful zirconia bonding include surface pretreatment, surface cleaning, and chemical priming of the restorative material. Creating a surface texture that is optimal for bonding is the first step, requiring the performance of a roughening procedure that will increase the bond strength of the zirconia. Saliva contamination must also be removed from of the intaglio surface of zirconia. Finally, ceramic-specific primers should be utilized to help achieve a durable bond to zirconia.
Surface Roughening
As mentioned previously, surface roughening through particle abrasion with alumina (Figure 1 and Figure 2) has been shown to improve the bond to zirconia.5-7 The effectiveness of alumina air-particle abrasion in increasing the flexural strength of zirconia was also reported in a systematic review and meta-analysis of laboratory studies.14 It was further noted that any microcracks introduced through air-particle abrasion were likely confined to a surface transformation layer that occurs when zirconia undergoes transformation toughening.14 The conventional procedure for air-particle abrasion with alumina is to sandblast for 10 seconds with 50 μm alumina particles at under 2 bar pressure (0.2 MPa or 30 psi).15 In the subgroup analyses of the meta-analysis, no difference was found for flexural strength of zirconia when using different sized particles (25 to 150 μm), different pressures (1 to 6 bars), or different time durations (5 seconds to 2.5 minutes).14 A recent study suggested that air-particle abrasion should be performed immediately before bonding a restoration, as bond strength decreases if bonding occurs more than 15 minutes after particle abrasion.15 However, this recommendation is not feasible for many dentists who need to utilize the dental laboratory for particle abrasion of their zirconia restorations.16
Translucent zirconia (ie, containing 4 to 5 mol% yttria) performs less transformation toughening than original (conventional) formulations of zirconia (ie, containing 3 mol% yttria). Translucent zirconia is therefore more susceptible to decreases in strength following alumina particle abrasion. If particle abrasion is omitted, however, the bond strength is drastically reduced.17 One strategy for bonding to translucent zirconia is to reduce the particle abrasion pressure to 1 bar.17Another strategy is to particle abrade with glass beads, which do not affect the surface of the zirconia; however, they may deposit some silica on its surface. The surface may then be bonded with a silane/MDP primer. This strategy is different than "tribochemical" bonding, which uses silica-coated alumina particles that will create microcracking on the surface of translucent zirconia.18
Other methods of creating surface texture have been examined, such as those using high concentration acids. For example, one study used a solution of ethanol, 37% hydrochloric acid, and ferric chloride,19 and another used a 40% hydrofluoric acid solution.20 Operator safety must be considered when using these high-concentration acids.
Surface Cleaning
One of the challenging aspects of bonding to zirconia is that the zirconia must be cleaned following try-in. During the try-in procedure, the zirconia may be contaminated with proteinaceous components, inorganic particles, and bacteria from saliva and blood that cannot be rinsed off with water. Cleaning the surface with phosphoric acid is not advised, as attachment of the dissociated phosphate group from the phosphoric acid may block the bonding sites of phosphate-based zirconia primers. Therefore, zirconia cleaners are needed to remove contaminants from the surface of zirconia. Several such cleaners are available, eg, Ivoclean (Ivoclar), which contains sodium hydroxide and zirconia particles, ZirClean™ (BISCO Dental), which contains potassium hydroxide, and Katana™ Cleaner (Kuraray Dental), which contains 10-MDP.21
A systematic review and meta-analysis that analyzed different methods for removing salivary contamination from zirconia restorations concluded that air-particle abrasion was an effective approach.22 As mentioned earlier, however, this method may not be possible in all clinics if the necessary equipment is not available and because of the potential inconvenience of needing to move to a laboratory to perform the procedure. The use of cleaning solutions was found to be another effective method for removing salivary contamination, and is easier to perform than air-particle abrasion. Another recent study determined that all the commercial cleaning products were effective for removing salivary contamination,23 while the systematic review noted that alcohol and hydrogen peroxide were not effective methods.22 Sodium hypochlorite was mentioned as another possible cleaning solution; however, it should be thoroughly rinsed off the surface of the zirconia restoration so that it does not interfere with resin polymerization.22
A further strategy for removing saliva contamination is to apply the 10-MDP primer before the surface has been contaminated with saliva. 10-MDP makes the surface of the zirconia hydrophobic such that water-based contaminants, such as saliva, may be rinsed off the surface of the restoration with water alone.24
Chemical Priming
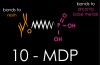
The 10-MDP molecule used to bond zirconia has a methacrylate functional group that bonds to resin cement and a phosphate-based functional group that bonds to zirconia (Figure 3). Several different chemical analyses have been performed to analyze the chemical bond between zirconia and 10-MDP.25-28
In one study, x-ray photoelectron spectroscopy was used to show that phosphorous atoms are present on the surface of zirconia after 10-MDP is applied and rinsed off.25 Fourier transform infrared spectroscopy revealed that the chemical bonds in the phosphate-based functional group of 10-MDP change state when mixed with zirconia.26 In another study, using time-of-flight secondary ion mass spectroscopy, zirconia and 10-MDP were allowed to bond and then ionized27; when their fragments were separated by atomic weight, fragments that corresponded to pieces of bonded 10-MDP and zirconia were found to exist.27 Finally, magic angle spinning nuclear magnetic resonance reported interatomic distances between zirconia and the phosphate-based functional group that correspond to ionic or hydrogen bonding.28
The 10-MDP molecule can be present in either ceramic-specific primers (eg, Z-Prime™ Plus, BISCO Dental; Monobond Plus, Ivoclar; Clearfil™ Ceramic Primer, Kurary Noritake Dental) or in universal adhesives that are also used to bond to tooth structure (eg, All-Bond Universal, BISCO Dental, Scotchbond™ Universal, 3M; Adhese® Universal, Ivoclar). A meta-analysis reported that ceramic primers and universal adhesives that contain 10-MDP were both effective at producing a bond with zirconia.29Silane is not an effective monomer for bonding to zirconia,30 and adding silane to MDP-based primers may actually be detrimental to the bond with zirconia.31
CONCLUSION
Bonding to zirconia can be advantageous in a number of clinical situations, such as when the strength of zirconia is desired for fixed partial denture connectors or when restorative space is limited. Additionally, the relative opacity of bonded zirconia veneers is useful in blocking out discolored preparations. Published reports provide ample evidence for the effectiveness of zirconia bonding. Laboratory studies have demonstrated short- and long-term improvements in bonding to zirconia when pretreatment with alumina air-particle abrasion is performed, while clinical trials have shown anterior resin-bonded zirconia fixed partial dentures to have high clinical survival rates. Clinicians may therefore benefit from learning the steps involved in a creating a successful bond to zirconia. Surface roughening should be undertaken with air-particle abrasion, which will not decrease the strength of original formulations of zirconia (those containing 3 mol% yttria), although lower pressures of particle abrasion may be needed for roughening translucent zirconia (ie, containing 4 to 5 mol% yttria). Cleaning solutions are necessary to remove contaminated saliva from the intaglio surface of zirconia restorations following try-in. Finally, chemical priming with ceramic-specific primers or universal adhesives containing 10-MDP should be performed. Because of its strength, durability, and esthetic properties, zirconia is an ideal restorative material in many clinical situations, and therefore adopting these bonding protocols will enable clinicians to gain from the several advantages offered by the high-strength bonding of this material.
References
1. Lawson NC, Litaker MS, Ferracane JL, et al; National Dental Practice-Based Research Network Collaborative Group. Choice of cement for single-unit crowns: findings from The National Dental Practice-Based Research Network. J Am Dent Assoc. 2019;150(6):522-530.
2. Heintze SD, Monreal D, Reinhardt M, et al. Fatigue resistance of all-ceramic fixed partial dentures - fatigue tests and finite element analysis. Dent Mater. 2018;34(3):494-507.
3. Lawson NC, Jurado CA, Huang CT, et al. Effect of surface treatment and cement on fracture load of traditional zirconia (3Y), translucent zirconia (5Y), and lithium disilicate crowns. J Prosthodont. 2019;28(6):659-665.
4. Cho Y-E, Lim Y-J, Han J-S, Yeo I-L, Yoon H-I. Effect of yttria content on the translucency and masking ability of yttria-stabilized tetragonal zirconia polycrystal. Materials (Basel). 2020;13(21):4726.
5. Inokoshi M, De Munck J, Minakuchi S, Van Meerbeek B. Meta-analysis of bonding effectiveness to zirconia ceramics. J Dent Res.2014;93(4):329-334.
6. Thammajaruk P, Inokoshi M, Chong S, Guazzato M. Bonding of composite cements to zirconia: a systematic review and meta-analysis of in vitro studies. J Mech Behav Biomed Mater. 2018;80:258-268.
7. Özcan M, Bernasconi M. Adhesion to zirconia used for dental restorations: a systematic review and meta-analysis. J Adhes Dent. 2015;17(1):7-26.
8. Tzanakakis EG, Tzoutzas IG, Koidis PT. Is there a potential for durable adhesion to zirconia restorations? A systematic review. J Prosthet Dent. 2016;115(1):9-19.
9. Scaminaci Russo D, Cinelli F, Sarti C, Giachetti L. Adhesion to zirconia: a systematic review of current conditioning methods and bonding materials. Dent J (Basel). 2019;7(3):74.
10. Papia E, Larsson C, du Toit M, Vult von Steyern P. Bonding between oxide ceramics and adhesive cement systems: a systematic review. J Biomed Mater Res B Appl Biomater. 2014;102(2):395-413.
11. Quigley NP, Loo DSS, Choy C, Ha WN. Clinical efficacy of methods for bonding to zirconia: a systematic review. J Prosthet Dent. 2021;125(2):231-240.
12. Blatz MB, Vonderheide M, Conejo J. The effect of resin bonding on long-term success of high-strength ceramics. J Dent Res. 2018;97(2):132-139.
13. Kwon SJ, Lawson NC, McLaren EE, Nejat AH, Burgess JO. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent. 2018;120(1):132-137.
14. Aurélio IL, Marchionatti AME, Montagner AF, May LG, Soares FZM. Does air particle abrasion affect the flexural strength and phase transformation of Y-TZP? A systematic review and meta-analysis. Dent Mater. 2016;32(6):827-845.
15. Blatz MB, Alvarez M, Sawyer K, Brindis M. How to bond zirconia: the APC concept. Compend Contin Educ Dent. 2016;37(9):611-617.
16. Lawson NC, Khajotia S, Bedran-Russo AK, et al; Council on Scientific Affairs. Bonding crowns and bridges with resin cement: an American Dental Association Clinical Evaluators Panel survey. J Am Dent Assoc. 2020;151(10):796-797.
17. Fu C-C, Darkoue Y, Burgess JO, Lawson NC, Givan DA, McLaren E. Surface treatment- shear-bond strength and biaxial flexural strength of zirconia. J Dent Res. 2019;98(Spec Iss A):3619.
18. Khanlar LN, Takagaki T, Abdou A, et al. Effect of air-particle abrasion protocol and primer on the topography and bond strength of a high-translucent zirconia ceramic. J Prosthodont. 2022;31(3):228-238.
19. Sakrana AA, Özcan M. Effect of chemical etching solutions versus air abrasion on the adhesion of self-adhesive resin cement to IPS e.max ZirCAD with and without aging. Int J Esthet Dent. 2017;12(1):72-85.
20. Xie H, Cheng Y, Chen Y, Qian M, Xia Y, Chen C. Improvement in the bonding of Y-TZP by room-temperature ultrasonic HF etching. J Adhes Dent. 2017;19(5):425-433.
21. Tian F, Londono J, Villalobos V, et al. Effectiveness of different cleaning measures on the bonding of resin cement to saliva-contaminated or blood-contaminated zirconia. J Dent. 2022;120:104084.
22. da Silva NRD, Araújo GM, Vila-Nova TEL, et al. Which zirconia surface-cleaning strategy improves adhesion of resin composite cement after saliva contamination? a systematic review and meta-analysis. J Adhes Dent. 2022;24(1):175-186.
23. Sulaiman TA, Altak A, Abdulmajeed A, Rodgers B, Lawson N. Cleaning zirconia surface prior to bonding: a comparative study of different methods and solutions. J Prosthodont. 2022;31(3):239-244.
24. Angkasith P, Burgess JO, Bottino MC, Lawson NC. Cleaning methods for zirconia following salivary contamination. J Prosthodont. 2016;25(5):375-379.
25. Xie H, Li Q, Zhang F, et al. Comparison of resin bonding improvements to zirconia between one-bottle universal adhesives and tribochemical silica coating, which is better? Dent Mater. 2016;32(3):403-411.
26. Chen Y, Lu Z, Qian M, Zhang H, Xie H, Chen C. Effect of 10-methacryloxydecyl dihydrogen phosphate concentration on chemical coupling of methacrylate resin to yttria-stabilized zirconia. J Adhes Dent. 2017;19(4):349-355.
27. Chuang S-F, Kang L-L, Liu Y-C, et al. Effects of silane- and MDP-based primers application orders on zirconia-resin adhesion-A ToF-SIMS study. Dent Mater. 2017;33(8):923-933.
28. Nagaoka N, Yoshihara K, Feitosa VP, et al. Chemical interaction mechanism of 10-MDP with zirconia. Sci Rep. 2017;7:45563.
29. Cuevas-Suárez CE, de Oliveira da Rosa WL, Vitti RP, da Silva AF, Piva E. Bonding strength of universal adhesives to indirect substrates: a meta-analysis of in vitro studies. J Prosthodont. 2020;29(4):298-308.
30. Elsayed A, Younes F, Lehmann F, Kern M. Tensile Bond Strength of So-called Universal Primers and Universal Multimode Adhesives to Zirconia and Lithium Disilicate Ceramics. J Adhes Dent. 2017;19(3):221-228.
31. Koko M, Takagaki T, Abdou A, et al. Effects of the ratio of silane to 10-methacryloyloxydecyl dihydrogenphosphate (MDP) in primer on bonding performance of silica-based and zirconia ceramics. J Mech Behav Biomed Mater. 2020;112:104026.