You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
While a number of pediatric oral health promotion programs have been implemented over the past fifty years in the United States (US), dental caries remain prevalent among low-income and minority children as compared to their counterparts.1 In 2015, the highest prevalence of dental caries (56.3%) were among children from households with incomes below 100% of the Federal Poverty Level (FPL), compared with 51.8%, 42.2%, and 34.8% among children from household income groups of 100%-199%, 200%-300%, and over 300% of the FPL, respectively.1 In 2007, 4.35 million US children were reported as having a toothache and dental caries within a 6-month period2 and of the over 12 million children with untreated dental caries in 2011-2014, roughly 2 million were aged 0-5 years.3 When left untreated, dental caries over time can become symptomatic, resulting in dental pain and infection, which in turn can influence nutrition, growth, development, and overall quality of life.4,5 While one of the major symptoms of untreated dental caries is a toothache, tooth eruption particularly in younger aged children, may also result in dental pain.6 Therefore, it is important for parents and caregivers to receive ongoing oral health education from both dental and non-dental professionals concerning their child's oral health, so that they are aware of the various oral cavity changes at each age milestone.
Programs such as the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is one mechanism to promote oral health through collaboration with dental professionals such as dental hygienists, or by training WIC staff members on basic oral health as it relates to nutritional health.6,7 The WIC program is one of the largest federally funded public health programs providing nutritious foods, nutritional education, and referrals to health care services8 including dental care7 to low-income pregnant, breastfeeding, and non-breast-feeding postpartum women, infants,8 and children under age 5. In 2018, there were roughly 7 million participants monthly9; more than half of the infants in the US participate in the program.7 Access to nutritious foods and nutritional education are necessary elements in promoting good oral health-related behaviors, which results in decreased dental caries risk. In some states, WIC programs address oral health through promoting a dental visit for the child by age one, ensuring families have a dental home, and discussing nutritional topics related to oral health if desired by the caregiver.10 Only a few studies have specifically examined oral health outcomes or the use of dental services in a WIC population.11-13 Among these cohort studies, findings have revealed that the prevalence of dental caries among child WIC participants increases with age13 and that WIC participants are more likely to receive preventive dental services compared to non-participants.11,12
Since many children under age 5 participate in WIC, it is important to understand the oral health status of these participants compared to non-participants. The purpose of this study was to use a nationally representative dataset to examine disparities associated with caregiver-reported cavities and toothaches among children aged 2-4 years across three categories of WIC eligibility and participation.
Methods
To address the study aim, data was obtained from the 2016 National Survey of Children's Health (NSCH),14 a nationally representative cross-sectional survey that includes key information related to the health and well-being of children and their families.15 The NSCH has been used in previous studies to examine oral health outcomes and dental service use among children.2,16,17 The NSCH data collection process consists of an address-sampling frame to identify households across the 50 states and District of Columbia. The inclusion criteria required participants to have a valid residential address and a completed screening survey for one child in the household. Among 138,009 households who completed the screening surveys, 67,047 households were eligible to complete the NSCH survey. The final NSCH 2016 dataset included a total of 50,212 non-institutionalized children aged 0-17 years and had an overall weighted response rate of 40.7%.15
The analytic sample for this study included children aged 2-4 years with complete information about the household's WIC participation (n=7,719). Since the survey asked parents/caregivers to report on children's conditions and status in the previous 12 months, children under the age of 2 years were not included in this analysis. It is rare for children under 12 months of age to experience a dental cavity because the first primary tooth does not erupt until around age 6 months. Similarly, with toothaches, the report of this problem would most likely be related to pain associated with tooth eruption (teething) instead of untreated dental cavities. More technical details about the survey can be found in the 2016 NSCH methodology report.15 Old Dominion University's Human Subjects Committee approved this study as exempt.
Independent Variables
The primary independent variables were the indicators of WIC eligibility and participation status. For the NSCH 2016 dataset, federal poverty level defined as total family income and family poverty threshold ranging from 50-400>FPL.15 Income eligibility for WIC, which is a household income ≤185% of the FPL was used for this study. Participation in WIC was defined as a family member in the household receiving WIC benefits during the past 12 months. Based on income eligibility and participation status, three groups were created: WIC participants, income-eligible non-participants, and higher-income non-participants. Child-level socio-demographics included age (2-4 years), sex (male or female), race and ethnicity (Hispanic, non-Hispanic white [NHW], non-Hispanic black [NHB]. Non-Hispanic other/multi-racial [NHO] was defined as children who reported as one race category of American Indian or Alaska Native, Native Hawaiian, or Pacific Islander and some other race. Multi-racial included non-Hispanic children who were reported as having more than one race); and type of health insurance was defined as public only, private only, other (private and public or unspecified), or uninsured.14 Caregiver-level socio-demographic variables were the highest educational attainment in the household (≤ high school/GED, some college/technical school, and college degree or higher), mother's age at the time the child was born was grouped by the researchers (18-25 years, 26-30 years, 31-35 years, and ≥ 36 years), and caregiver-reported condition of the child's teeth (excellent/very good, good, fair/poor).15
Dependent Variables
The dependent variable was defined by the caregiver's report of dental cavities and toothaches of the child. Both outcome measures were defined as binary indicators, i.e., yes or no, based on the following questions from the NSCH: "During the past 12 months, has [this child] had frequent or chronic difficulty with any of the following: decayed teeth or cavities, or toothaches."18
Statistical Analysis
The data were analyzed with Stata Statistical Software: Release 15 (StataCorp.; College Station, TX). All analyses were weighted to account for the complex survey design. Missing data were removed from the analysis. Weighted proportion and chi-square tests werev estimated for all sociodemographic variables among WIC participants, income-eligible non-participants, and higher-income non-participants. Similarly, chi-square tests were performed to evaluate differences in caregiver-reported dental cavities and toothaches among the three groups. Multivariate logistic regressions were used to examine the disparities in caregiver-reported oral health status (dental cavities and toothaches) among the three groups. All models were stratified by child and caregiver-level sociodemographic characteristics while controlling for covariates, and WIC participants were the reference group for each model. Statistical significance for all analysis was reported at p< 0.05.
Results
Demographics
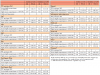
The analytical sample included children aged 2-4 years (n=7,719), over half were NHW (54.4%) and most were reported as having private insurance. Among all children, there were WIC participants (n=1,032), income-eligible non-participants (n=1,037), and higher-income non-participants (n=5,650). Roughly one-third of the WIC participants were NHW (33.0%) and 74.4% were insured through public insurance. Over 40% of caregivers who were WIC participants attained less than a high school diploma, or high school/GED and 37.7% were age 18-25 years. Income-eligible non-participating children had a higher proportion of no-insurance (10.3%) than WIC participating children (6.6%) and higher-income non-participating children (2.4%) (p<0.001).
Higher-income non-participating children had statistically different demographics from WIC participating children. For example, there was a higher proportion of higher-income non-participating children who were NHW, privately insured, and had a caregiver(s) with a higher educational attainment and were older in age. In terms of the caregivers' report of their child's teeth condition, WIC participants were more likely to report their child's teeth as fair/poor (6.0%) than income-eligible non-participants (4.4%) and higher-income non-participants (1.5%) (p<0.001) (Table I).
Caregiver-Reported Dental Cavities
Overall, the prevalence of caregiver-reported dental cavities differed among WIC participants and non-participants. The proportion of caregiver-reported dental cavities was greater among WIC participants (10.0%) than income-eligible non-participants (8.9%) and higher-income non-participants (4.4%) (p<0.001). The proportion of caregiver-reported dental cavities increased with age for WIC participants with children aged 4 years having the highest reported cavities (18.6%) compared with income-eligible non-participants (10.4%) and higher-income non-participants (7.4%) (p<0.001). When stratified by race and ethnicity, NHW WIC participants had higher caregiver-reported dental cavities (14.0%) than income-eligible non-participants (6.7%) (p=0.03). This racial disparity was consistent among all WIC participating children. Hispanic WIC participants had the lowest caregiver-reported (5.9%) dental cavities compared with income-eligible participants (13.4%), but the disparity was not statistically significant (p=0.08). However, NHB WIC participants had nearly 3.6 times (9.0%) more caregiver-reported dental caries than NHB income-eligible non-participants (2.5%) (p=0.03). Children participating in WIC whose mothers were aged >36 years had a higher proportion of reported dental cavities (17.2%) than non-WIC participating children (income-eligible non-participants - 8.6% and higher-income non-participants - 4.0% (p=<0.001) (Table II).
Caregiver-Reported Toothaches
In terms of toothaches, WIC participants (5.2%) had higher caregiver-reported toothaches than income-eligible non-participants (3.2%), and higher-income non-participants (0.1%) (p<0.001). Similar to caregiver-reported dental cavities, WIC participants who were aged 4 years also had higher caregiver reported toothaches (6.6%) than income-eligible non-participants (1.9%) (p=0.03). Among race and ethnic groups, NHW WIC participants (8.2%) had higher caregiver-reported toothaches than NHW income-eligible nonparticipants (1.9%) (p=<0.01). However, among Hispanic WIC participants there was a lower caregiver report of toothaches (0.5%) than Hispanic income-eligible non-participants (2.8%) (p=0.03). Also similar to dental cavities, WIC-participating children whose mothers aged >36 years reported more toothaches (5.9%) than non-WIC participating children (income-eligible non-participants-2.9% and higher-income non-participants (0.7%) (p=<0.01) (Table III).
In general, there was a higher portion of caregiver-reported fair/poor teeth conditions associated with dental cavities or toothaches for all three WIC eligibility and participation groups. When stratified by eligibility and participations groups, there were differences but without statistical significance (Tables II and III).
Adjusted odds for caregiver-reported dental cavities and toothaches
The adjusted logistic regression results after controlling the confounders with WIC participants as the reference group for all models are shown in Table IV. In general, higher-income non-participants had higher odds (OR: 1.93; 95% CI: 1.05-3.52; p<0.05) of caregiver-reported dental cavities than WIC participants. This association holds in certain socio-demographic subgroups as well. For example, higher-income non-participants who were girls (OR: 3.17; 95% CI: 1.31-7.64; p<0.05), NHB (OR: 20.58; 95% CI: 2.82-150.48; p<0.05) or insured through public insurance (OR: 3.03; 95% CI: 1.19-7.74; p<0.05) had higher odds of caregiver-reported dental cavities than WIC participants. When examining dental cavities, higher-income non-participant children whose caregivers were aged 18-25 years had higher odds of reported dental cavities (OR: 3.17; 95%CI: 1.06-9.49; p<0.05) than WIC participants. Caregivers of higher-income non-participating children who reported their child's teeth condition as excellent or very good had higher odds of dental cavities (OR: 4.04; 95%CI: 1.18-13.85) than WIC participants. In terms of toothaches, caregivers of income-eligible non-participating children who reported their child's teeth condition as fair/poor had higher odds of toothaches (OR: 7.90; 95% CI 1.71-36.57) than WIC participants (Table V).
Discussion
While some studies have examined the oral health outcomes and dental service use of WIC children at the local or state-levels,11-13 to the best of the authors' knowledge, this is the first study to use a nationally representative dataset to examine caregiver-reported dental cavities and toothaches by WIC eligibility and participation. When comparing all three WIC eligibility and participation groups, caregiver-reported dental cavities were higher than toothaches. However, the adjusted odds ratio revealed an opposite finding when all socio-demographic characteristics were controlled in the logistic regression model for dental cavities.
Higher-income non-participants had higher odds of caregiver-reported dental cavities than WIC participants. This observed pattern varied when stratified by sociodemographic characteristics. Specifically, higher-income non-participants, insured through public insurance, had higher caregiver-reported odds of dental cavities than WIC participants. It should be noted that in the current study the federal poverty level used to determine WIC eligibility was ≤185%. Some families whose household income is >185% FPL may be eligible for other federal and state-level benefits such as Medicaid or the Children's Health Insurance Program (CHIP) within their respective state.19,20 Medicaid provides the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) for children under 21 years and offers children services such as periodic screenings for hearing, vision, and dental health.19 The CHIP program provides coverage for children under 19 years and whose family income does not meet the Medicaid eligibility limit and also includes dental benefits for children.20 One of the benefits of WIC, aside from nutritional education and services, are referrals to the welfare, health care system and dental services.10 Early recognition and diagnosis of dental cavities leads to better health and oral outcomes for the child.
Overall findings of this study suggest that dental cavities in some WIC eligibility and participant groups may be addressed prior to becoming symptomatic. Among WIC participating children, when the caregiver-reported conditions of teeth were examined independently among all three WIC eligibility and participation groups, WIC participants had a higher report of fair/poor teeth conditions than non-WIC participants, which is reflective of the caregivers' report of dental cavities. In general, there was a higher caregiver report of fair/poor conditions associated with dental cavities and toothaches among all WIC eligibility and participation groups.
These findings potentially highlight the caregivers' awareness of the child's dental needs, which may lead to timely treatment. Talekar et al. found that parents of pre-school aged children identified their child's oral health as poor if they perceived the need for dental treatment or preventive dental care.21 Similarly, Sohn et al. also found parents' perception of their child's oral health to be related with the clinical observations of dental caries.22 Divaris et al. also reported similar findings.23 However, their results also highlighted the overestimation of the child's oral health status but an underestimation of dental treatment needs particularly, among very young children (aged <2 years).23 These observed differences must be considered when measuring caregiver-reported outcomes for the child.
Caregiver-reported dental cavities and toothaches
When examining only WIC participating children, caregiver-report of dental cavities increased with age; with children aged 4 years having this highest reported among all three age groups and nearly doubled when compared to nonparticipants. This finding is consistent with Gold et al. who also examined dental caries prevalence among children in a community-based WIC oral health program in Florida.13 Their findings revealed that among children aged ≤1-5 years, dental caries increased with age and the highest prevalence were among children aged 4 and 5 years (43.5% and 81.1%, respectively). The current study also found a consistent pattern with caregiver-reported toothaches among WIC participating children. While the proportion of caregiver-reported toothaches decreased for all WIC participating age groups, caregivers of children aged 4 years, reported nearly two-times more incidence of toothaches than higher-income non-participants. Lewis et al. used the 2007 NSCH dataset and found that children from low-income families (<100% FPL and 101%-200% FPL) and Medicaid insured, (14.7%) had a higher prevalence of toothaches compared to those who were privately insured (8.6%).2
Among race and ethnicity groups, WIC participating children who were Hispanic had higher caregiver-reported dental cavities but lower reported toothaches. However, among WIC participating children who were NHB, caregivers reported dental cavities nearly 3.6 times more than income-eligible nonparticipating children. In general, NHB and Hispanic children tended to have a higher prevalence of dental caries.1 One study found that African American children were more likely to have never had a dental visit, or had longer intervals between dental visits than White children.24 A national study found that children WIC participants who were NHB had a poorer diet and nutrient intake to include more added sugars and sodium than NHW children.25 The time between dental visits paired with dietary habits may explain the dental cavities prevalence observed among NHB children.
In addition to timely routine dental care and diet, WIC participation rates across race/ethnicity may help explain the oral health disparities among Hispanic and NHB children. For example, in 2015 Hispanic infants and children had the highest rate of participation out of those were eligible (62.7%, n=5,190,958) compared to NHW (42.2%, n=5,854,332) and NHB (57%, n=2,721,555) children.26 Similar to the current study findings, there was a higher proportion of NHW children who were income-eligible but non-WIC participants than Hispanic, NHB, NHO children. Participation in the WIC program may offer Hispanic families the resources and support needed to navigate the health care system while providing continuous nutritional education in the first years of life. The literature suggests that Hispanic mothers and their social networks who perceive preventive dental care as important are more likely to obtain dental care at an early age and continue dental care.27
In general, it has been shown that WIC participating children are more likely to receive preventive and restorative dental services than nonparticipating children.11 These factors may help to explain the positive impact of WIC observed among some participants in the current study. However, more culturally sensitive studies may be needed to design effective programs to reduce the racial/ethnic disparities identified in WIC programs. It was also shown that caregivers who were older or had attained less than a college degree reported more dental cavities and toothaches with varying degrees among the three WIC participation and eligibility groups. These socio-demographic characteristics provide further support that caregivers' level of educational attainment may be related to greater awareness of their child's dental needs; however, accessing dental services in a timely manner may also be a barrier.
Limitations
This study had limitations. Due to the cross-sectional design of the 2016 NSCH data collection, causal inferences could not be determined. Most of the demographic variables included in the analysis were non-modifiable factors. Subjectivity and recall bias must also be considered for caregivers' report of dental cavities and toothaches. Additionally, due to the self-administered format of the survey, other biases, such as social desirability and interpretation of questions, must be taken into consideration. Particularly, the question concerning dental cavities used in the survey. In the asymptomatic stages of dental cavities, caregivers may underestimate the appearance of dental caries28 as well as treatment needs.23 This may explain differences observed among WIC eligibility and participation groups by sociodemographic characteristics. Self-selection bias into the WIC program may also explain differences associated with a higher caregiver-report of dental cavities and toothaches among WIC participants compared to income-eligible non-participants. Children who participate in the WIC program may be more likely to access dental services through referrals that the WIC program provide and therefore, are advised about dental problems earlier than non-participants.
Given these limitations, the use of caregiver-reported information has been used when clinical data is not available.2,16,17 Future research may include comparing clinical findings of dental caries to those that are caregiver-reported from a representative sample that include various racial and ethnic groups by WIC eligibility and participation.
Implications for dental hygienists
While not required of WIC programs, in some states, WIC clinics have dental partnerships to assist in the promotion of oral health and offer preventive services such as education, screenings, and fluoride treatments.7 Further, WIC programs that have partnered with dental and medical professionals, safety net, and health clinics have been able to provide education, preventive dental services and referrals as needed for children.29 In addition, with increasing direct access20 and innovative workforce models such as the dental therapist,31 dental hygienists can provide patient care in diverse settings such as WIC, to narrow the oral health disparity gap. Increasing collaborative partnerships and direct access to dental hygiene care within WIC programs is one strategy to address the dental caries burden among children.
Conclusions
Using a nationally representative data, this study provided insight on the oral health outcomes of WIC participants compared to non-participants. When stratified by child and caregiver-level characteristics, there were oral health disparities across WIC eligibility and participation. However, in some cases, WIC participation revealed a lower caregiver-report of dental cavities and toothaches compared to non-participating groups. Examining the oral health promotion and education practices within WIC programs for caregivers is warranted to identify factors contributing to the disparities in reporting cavities and toothaches. Partnerships between dental hygienists, dentists, WIC programs, and health clinics can promote early prevention and detection of dental cavities, which will narrow the oral health disparity gap among children.
Disclosure
This research was partially funded by the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health & Human Development (R03HD090387-01).
Denise M. Claiborne, PhD, MS, RDH is an assistant professor and the Graduate Program Director, Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University, Norfolk, VA, USA.
Chun Chen, PhD is an associate professor, School of Public Health and Management, Wenzhou Medical University, Chashan University, Wenzhou, Zheijang, PRC.
Qi Zhang, PhD is a professor and the Health Services Research PhD Program Director, School of Community and Environmental Health, Old Dominion University, Norfolk, VA, USA.
References
1. Fleming E, Afful J. Prevalence of total and untreated dental caries among youth: United States, 2015-2016 [Internet]. Maryland: National Center for Health Statistics; 2018 Apr [cited 2020 Mar 25]. Available from: https://www.cdc.gov/nchs/data/databriefs/db307.pdf.
2. Lewis C, Stout J. Toothache in US children. Arch Pediatr Adolesc Med. 2010 Nov 1; 164(11):1061-1063.
3. Gupta N, Vujicic M, Yarbrough C, Harrison B. Disparities in untreated caries among children and adults in the U.S., 2011-2014. BMC Oral Health. 2018 Mar 6;18(30):1-9.
4. Sheiham A. Oral health, general health and quality of life. [Internet]. Bulletin of the World Health Organization; 2020 Sep [cited 2020 Sep 12]. Available from: https://www.who.int/bulletin/volumes/83/9/editorial30905html/en/.
5. CDC. Children's oral health. [Internet]. Atlanta: Center for Disease Control and Prevention; 2020 [cited 2020 Dec 5]. Available from: https://www.cdc.gov/oralhealth/basics/childrens-oral-health/index.html
6. AAP. Toothaches in children. [Internet]. Itasca: American Academy of Pediatrics; 2020 [updated 2015; cited 2020 Oct 10]. Available from: https://www.healthychildren.org/English/health-issues/injuries-emergencies/Pages/Toothaches-in-Children.aspx.
7. Center for Oral Health. WIC early entry into dental care [Internet]. Manhattan Beach: Center for Oral Health; 2020 [cited 2020 Oct 19]. Available from: https://www.centerfororalhealth.org/wp-content/uploads/2018/11/wic_dental_guidebook.pdf
8. USDA. About WIC-WIC at a glance. [Internet]. Washington DC; US Department of Agriculture, Food and Nutrition Service; 2020. [cited 2020 Oct 19]. Available from: https://www.fns.usda.gov/wic/about-wic-wic-glance
9. USDA. WIC program overview. [Internet]. Washington DC; US Department of Agriculture, Food and Nutrition Service; 2020. [updated 2020; cited 2020 Oct 19]. Available from: https://www.ers.usda.gov/topics/food-nutrition-assistance/wic-program/.
10. NWA. Statement on WIC and oral health NWA 2011. [Internet]. Washington DC: National WIC Association; 2020 [cited 2020 Oct 19]. Available from: https://s3.amazonaws.com/aws.upl/nwica.org/statement_wic_oral_health.pdf
11. Lee JY, Rozier G, Norton EC, Kotch JB, Vann WF. Effects of WIC participation on children's use of oral health services. Am J Public Health. 2004 May;94(5):772-77.
12. Lee JY, Rozier G, Norton EC, Kotch JB, Vann WF. The effects of Women, Infants, and Children supplemental food program on dentally related Medicaid expenditures. J Public Health Dent. 2004 Spr;64(2):76-81.
13. Gold J, Tomar SL. Interdisciplinary community-based oral health program for women and children at WIC. Matern Child Health J. 2018 Jun 23;22(11):1617-1623.
14. CAHMI. 2016 National Survey of Children's Health (NSCH). [Internet]. Baltimore: Data Resource Center for Child and Adolescent Health; 2020 [cited 2020 Oct 19]. Available from: www.childhealthdata.org.
15. US Census Bureau. 2016 National survey of children's health methodology report. [Internet]. Washington, DC: US Department of Commerce Economics and Statistics Administration. US Census Bureau; 2018 Feb 2 [cited 2020 Oct 19]. Available from: https://www.census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/methodology/2016-NSCH-Methodology-Report.pdf
16. Lewis CW, Johnson BD, Linsenmeyar KA, et al. Preventive dental care for children in the United States: A national perspective. Pediatrics. 2007 Mar;119(3): e544-e553.
17. Lebrun-Harris LA, Canto MT, Vodicka P. Preventive oral health care use and oral health status among U.S. Children: 2016 National Survey of Children's Health. JADA. 2019 Apr 1;150(4):246-58.
18. CAHMI. Guide to topics and questions asked. [Internet]. Baltimore: Data Resource Center for Child and Adolescent Health; 2020 [cited 2020 Mar 4]. Available from: https://www.childhealthdata.org/learn-about-the-nsch/topics_questions/2016-nsch-guide-to-topics-and-questions.
19. CMS. Early and periodic screening, diagnostic and treatment (EPSDT): a guide for states: coverage in the Medicaid benefit for children and adolescents. [Internet]. Baltimore: Center for Medicare and Medicaid Services; 2014 [cited 2020 Mar 25]. Available from: https://www.medicaid.gov/sites/default/files/2019-12/epsdt_coverage_guide.pdf.
20. CMS. Children's insurance program (CHIP) benefits. [Internet]. Baltimore: Centers for Medicare & Medicaid Services; 2020 [cited 2020 Sep 12]. Available from: https://www.medicaid.gov/chip/benefits/index.html
21. Talekar BS, Rozier RG, Slade GD, Ennett ST. Parental perceptions of their preschool-aged children's oral health. J Am Dent Assoc. 2005 Mar 1; 136:364-72.
22. Sohn W, Taichman LS, Ismail Ai, Reisine S. Caregiver's perception of child's oral health status among low-income African Americans. Pediatr Dent. 2008 Nov-Dec; 30(6): 480-7.
23. Divaris K, Vann W, Baker DA, Lee J. Examining the accuracy of caregivers' assessments of young children's oral health status. J Am Dent Assoc. 2012 Nov 1;143(11):1237-47.
24. Pourat N, Finocchio L. Racial and ethnic disparities in dental care for publicly insured children. Health Aff. 2010 Jul;29(7):1356-63.
25. Zimmer MC, Rubio V, Kintziger KW, Barroso C. Racial/ethnic disparities in dietary intake of U.S. children participating in WIC. Nutrients. 2019 Nov 11;11(2607):1-10.
26. USDA. WIC 2015 eligibility and coverage rates. [Internet]. Washington DC; US Department of Agriculture, Food and Nutrition Service; 2018 [cited 2020 Oct 19]. Available from: https://www.fns.usda.gov/wic/wic-2015-eligibility-and-coverage-rates.
27. Kim Rhee YO. Reducing disparities in dental care for low-income Hispanic children. J Health Care Poor Underserved. 2005 Aug 3;16(3):431-43.
28. Horton S, Barker JC. Rural Mexican immigrant parents' interpretation of children's dental symptoms and decisions to seek treatment. Community Dent Health. 2008 Dec; 26(4):216-21.
29. National Maternal and Child Oral Health Resource Center. Targeted MCH oral health service systems project highlights [Internet]. Washington DC; National Maternal and Child Oral Health Resource Center; 2020 [cited 2021 Jan 14]. Available from: https://www.mchoralhealth.org/PDFs/TOHSS_ProjectHighlights.pdf.
30. ADHA. Facts about the dental hygiene workforce in the United States. [Internet]. Chicago: American Dental Hygienists' Association; 2021 [cited 2021 Jan 15]. Available from: https://www.adha.org/resources-docs/75118_Facts_About_the_Dental_Hygiene_Workforce.pdf.
31. ADHA. Expanding access to care through dental therapy. [Internet]. Chicago: American Dental Hygienists' Association; 2021 [cited 2021 Jan 15]. Available from: https://www.adha.org/resources-docs/Expanding_Access_to_Dental_Therapy.pdf.