You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
From the beginning of the COVID-19 global pandemic, numerous lives and communities have been affected by this complex and serious disease. Worldwide, over 271 million people had been infected, while more than 5.3 million died from this disease.1 By December 2021, more than 50.1 million people had been infected in the United States (US) and 798,997 had died of COVID-19.1 To address this health crisis, public health measures were instituted including social distancing, wearing face masks, hand washing, and avoidance of crowded indoor spaces. In November 2020, several pharmaceutical companies reported early results of large vaccine trials demonstrating efficacy for most participants.2 Pharmaceutical companies began seeking federal and regulatory approvals, and by early December 2020 various state and national agencies were discussing vaccine acquisition, storage, and distribution.2,3
Vaccinations represent an important public health tool for mitigating dangerous diseases including polio, measles, smallpox, influenza, and COVID-19. According to the World Health Organization (WHO), vaccines have prevented at least 10 million deaths between 2010-2015 worldwide and millions more have been protected from suffering and disability.4 Nevertheless, skepticism and hesitancy surrounding vaccinations remains among populations around the world,5,6 and vaccine hesitancy is considered to be one of the top global health threats.7 Vaccine hesitancy is the term used to describe individuals who display reluctance or refusal to receive vaccines despite the public health recommendations and the availability of vaccination services.8,9 Hesitancy toward COVID-19 vaccination can be a significant barrier to the prevention efforts aimed at alleviating the devastating consequences of this pandemic.
The issue of vaccine hesitancy among the US public, both prior to and since the availability of COVID-19 vaccines, has been studied to better understand the factors influencing attitudes and behaviors. One longitudinal study conducted from March to August 2020, surveyed US residents from across the country (n=1,018) to determine the intention to receive the COVID-19 vaccine once available, along with general vaccination attitudes including intention to get a flu vaccine. Findings for all measures demonstrated a statistically significant decreasing trend in intention to receive a COVID-19 vaccine over the 6-month period of the study. This trend was identified as being driven by participants who identified their political party affiliation as Republican and who also tended to perceive the SARS-CoV-2 virus as less threatening. Influencing factors included exposure to media channels and social networks.10 Another study related to the impact of COVID-19, and factors contributing to COVID-19 vaccine refusal was conducted among a cross section of individuals across the US to reflect national census data.11 Results revealed that 68% (n=316) of respondents were supportive of being vaccinated when it became available; however, concerns regarding the vaccine centered on possible side effects, efficacy, and length of testing.11 It was concluded that messaging to the public should promote information regarding the safety of vaccines, transparency, and thoroughness of testing to improve vaccination rates.11 Furthermore, it was recommended to emphasize the consequence of the pandemic on the overall health and well-being of the US population in vaccination messaging as well as ensuring that low-income populations have access to the COVID-19 vaccine.11
Another study of adults in the US (n=1,971) conducted in July of 2020, focused on the factors associated with the choices and willingness to accept a hypothetical COVID-19 vaccine.12 Attributes included vaccine related attributes and political factors.12Results revealed that an increase in efficacy and duration were associated with a higher probability of choosing a vaccine, as were endorsements from the US Centers for Disease Control and Prevention and the WHO as compared to other political endorsements.12 Respondents who indicated Democrat political party were significantly more likely to report willingness to receive a COVID-19 vaccine than those who reported Republican political partisanship.12 Older adults, Black individuals, women, and uninsured adults reported being less likely, on average, to receive a COVID-19 vaccine, and it was recommended that public health authorities consider outreach strategies that address these specific factors.12
A similar national study of US adults was conducted in June 2020 to identify population subgroups with higher probabilities of vaccine hesitancy towards a potential COVID-19 vaccine.13 Of these respondents, 22% (n=1,878) reported vaccine hesitancy, which was higher among females, African Americans, Hispanics, those who had children at home, rural dwellers, people in the northeastern US, and those identifying as Republicans.13 It was concluded that evidence-based education and policy level interventions would be needed to promote COVID-19 immunization programs, and that willingness to be vaccinated might change once COVID-19 vaccines become available.13
Vaccine acceptance and hesitancy among health care workers is an important consideration to explore, as health care workers are exposed to a higher risk of infections.14 In addition, health care providers are viewed as trusted individuals who are able to share evidence-based information regarding vaccines to their patients and the public.15 Furthermore, as a means to ensure an adequate workforce to provide care for infected patients, health care workers were among the first group to receive the COVID-19 vaccine in early 2021. Assessing the attitudes of health care workers also helps address barriers to widespread vaccination acceptance.
Prior to the availability of a COVID-19 vaccine, health care workers across five hospital systems in New Mexico, Texas, Missouri, and Ohio were surveyed between October and November of 2020 to determine their willingness to receive a COVID-19 vaccine.16 Only 36% (n=3,479) indicated willingness to take a COVID-19 vaccine as soon as it became available.16 Most respondents were female, white, indicated that they were Democrat or Liberal, had no chronic medical conditions and were younger than 40 years of age.16 Concerns included safety, adverse effects, effectiveness, rapidity of development/approval, and trust of government and regulatory authorities overseeing the vaccine development.16 Females and Black health care workers had lower acceptance while those identifying as Democrat/Liberal indicated higher vaccine acceptance.16 Healthcare workers who had not taken care of COVID-19 patients had higher refusal rates.16 Of those who were not planning to receive a COVID-19 vaccine, they also indicated that they would not recommend the vaccine to family and friends. Many respondents indicated trusting their own health care providers for recommending the COVID-19 vaccine. This finding could suggest an important role for key messaging through professional societies to increase vaccination acceptance and uptake among health care workers.16
Health care students represent another key population to consider regarding vaccinations. Vaccine hesitancy and acceptance among medical students at an allopathic medical school in southeast Michigan were assessed in an online survey during September 2020.17 Findings revealed that 23% of the participants (n=167) were vaccine hesitant with concerns related to serious side effects, lack of trust from public health experts, politicization of the vaccine, transparency, and speed of vaccine development impacting safety. Based on the study results, it was recommended an educational curriculum be developed to enhance medical student knowledge about COVID-19 vaccine and to teach counseling skills so they can share vaccination experiences with patients and encourage vaccination.17 In a companion study comparing COVID-19 vaccine acceptance and hesitancy among dental and medical students, results from the medical student study17 were compared to dental students from Michigan, Florida, and Utah who completed the same survey in December 2020.18 Results revealed that 45% of the dental students (n=248) were hesitant to receive the COVID-19 vaccine18 as compared to 23% of the medical students (n=167).17 More dental students (11%) compared with medical students (3%) reported having contracted COVID-19 and were more likely to indicate that the only reason they will get the vaccine is if it is mandated.18
Oral health care providers, including dentists and dental hygienists, fall into the high-risk category for potential exposure to the SARS-CoV-2 virus. Dentists and in some states, dental hygienists, are now authorized to administer the COVID-19 vaccine to the public and patients. Oral health care providers can serve as advocates for the vaccine to their patients. However, before an oral health care provider is allowed and willing to perform duties as vaccinators, they should be knowledgeable about vaccines and agree to receive the COVID-19 vaccine themselves. Findings from the dental student vaccine acceptance and hesitancy study indicated that nearly half of the dental student participants do not meet these criteria and highlighted the need for additional curricular education designed to enhance knowledge about the COVID-19 vaccine and vaccine counseling skills.18
Outside of the US, in February 2021 a global study of vaccine hesitancy was conducted through the International Association of Dental Students.19 Dental students from 22 countries (n= 6,639) completed the questionnaire.19 Findings revealed that 22.5% of dental students were vaccine hesitant while 13.9% rejected COVID-19 vaccines.19 Participants from lower income levels, females, and those infected and recovered from a COVID-19 infection, tended to be more vaccine hesitant or vaccine resistant.19 They also indicated using media and social media as their primary source of vaccine-related information,19 thus exposing them to misleading information. Insufficient knowledge about vaccines and their safety, and mistrust of governments and the pharmacological industry were identified as barriers for vaccination.19 The authors indicated that urgent interventions by health organizations were needed to work proactively with media content creators to disseminate higher quality messaging as well as improved dental curricula related to infectious disease epidemiology education and vaccination trends.19
International studies have also been conducted among oral health care professionals. Vaccine hesitancy and adherence intentions among Italian dentists enrolled at the Board of Physicians and Dentists in Lombardy was surveyed in December 2020.20 Of the participants (n=421), 10.9% had received a diagnosis of COVID-19, while 17.8% reported vaccine hesitancy or resistance.20 Reasons cited included fear the vaccine was unsafe and fear of adverse events, concerns of pharmaceutical companies influence decisions on vaccination policies, previous diagnosis of COVID-19, and belief that the vaccine had suboptimal protective efficacy.20 In another study conducted in Israel during December 2020, vaccination attitudes, including specific attitudes towards COVID-19 vaccines, were surveyed among dentists (n=67) and dental hygienists (n=73) as compared to the Israeli public (n=361).21 In general, dental hygienists had more negative attitudes toward vaccines, demonstrated significant mistrust of vaccine benefits, more worries over unforeseen future effects, more negative attitudes toward the COVID-19 vaccines and showed significantly more concerns about commercial profiteering.21 Compared to the general female Israeli adult population, dental hygienist respondents in this study appeared to have a higher anti-vaccination approach to the COVID-19 vaccine.21
Based on the results of these international studies, it can be concluded that the vaccination of health care workers, including oral health care providers, should remain a high priority due to heightened occupational risk levels20 and that ongoing public health messaging, vaccination education programs and the promotion of trust by local health authorities may aid in decreasing vaccine hesitancy among oral health care providers and the public.21 Due to the limited scope of literature related to dental hygienists' attitudes regarding COVID-19 vaccination in the US, the purpose of this study was to determine the intentions and hesitancy among US dental hygienists toward COVID-19 vaccination.
Methods
Registered dental hygienists in the American Dental Hygienists' Association (ADHA) database (n=133,000) were invited to participate in a longitudinal anonymous web-based survey (Qualtrics; Provo, UT, USA) from 9/29/20 through 8/30/21. Eligibility criteria included being 18 years of age, licensed as a dental hygienist in the US, and employment as a clinical dental hygienist as of 3/1/20. Potential respondents signed an electronic informed consent before participating in the survey. The survey was sent monthly and remained open for 5-10 days for responses. The novel survey and research were approved by the ADA Institutional Review Board and preregistered at ClinicalTrials.gov (NCT04423770). Further details of the study population and questionnaires have been described previously.22,23
This study focused on survey questions related to COVID-19 vaccination. On 9/29/20 respondents were asked to rate the degree to which they were concerned about COVID-19 transmission to themselves or patients on a scale of 1-5, with 1 being very concerned and 5 being not concerned at all. Scores of 1-2 were categorized as very concerned, 3 as moderately concerned, and 4-5 as not concerned. Additional questions were added over the course of the longitudinal study, including on 1/4/21 inquiring whether respondents intended to be vaccinated for COVID-19, on 2/1/21 whether respondents had been vaccinated or planned to be vaccinated for COVID-19 and any barriers encountered to receiving a COVID-19 vaccination, and on 6/1/21 whether respondents felt safer having been vaccinated, or if unvaccinated, what information was needed in order to consider being vaccinated. Lastly, on 8/16/21 unvaccinated respondents were asked what they would do if a COVID-19 vaccination was mandated by their employers. Respondents were categorized as being willing to be vaccinated if they were either partially or fully vaccinated against COVID-19 or if they stated that they planned to be vaccinated; respondents were categorized as being hesitant if they stated they were not planning to be vaccinated. Not all questions were asked every month, and respondents were free to skip questions, or end the survey before completion. Respondents could skip months and re-join the survey at any point.
Content analysis was used to analyze write-in responses. Themes were identified inductively, with iterative coding of each response by two independent researchers. Disagreements were resolved via discussion. Descriptive statistics, Chi-square and Fisher Exact tests, and logistic regression modeling were conducted in SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA), with statistical significance set at 0.05. Purposeful model selection was used to build the multivariable regression model. Individual variables that were not statistically significant in single variable models and did not diminish the Akaike Information Criterion (AIC) value of the model, in comparison to other models, were not included in the final multivariable models. Multicollinearity was tested for, but none was found. There was no pattern in missing vaccination information (all regression p-values >0.05) indicating the data is missing at random. Under this assumption, available case analysis was used.
Results
Survey respondents were aged 18 to 77 years with a mean of 44.42 years (SD: 11.92). Most respondents were female (88.8%, n=6192), with 1.1% identifying as male (n=76), and 10.2% identifying as another gender or preferring not to say (n=708). Non-Hispanic Whites made up the majority (73.4%, n=5118), while 6.9% identified as Hispanic (n=483), 3.3% identified as Non-Hispanic Asian (n=231), 2.0% identified as Non-Hispanic Black (n=142) and 4.4% identified as another race or as preferred not to state (n=277). Every US state, as well as Washington, D.C., the Virgin Islands and Puerto Rico, was represented in the sample. Demographic characteristics of the sample are shown in Table I.
Rates of the fully vaccinated respondents increased sharply from 2/5/21 to 3/5/21 (26.0% to 53.9%), then leveled off in subsequent months and ended at 75.4% on 8/30/21 (Figure 1). Rates of the partially vaccinated stayed fairly level throughout the study, ending with 80.5% of the respondents having received at least one dose of a COVID-19 vaccine by 8/30/21. There were 4.7% of respondents who said they were planning on getting vaccinated but had not yet been vaccinated by the end of the survey.
The percentage of individuals who received at least one COVID-19 vaccine dose by 8/30/21 varied state by state (Figure 2). Of the respondents, the highest percentages of partially or fully vaccinated dental hygienists were found in Hawaii (100%, n=17), Alaska (92.3%, n=13) and Maryland (90.7%, n=75). The lowest percentages were identified in Kansas (60.0%, n=30), Alabama (60.0%, n=10) and New Mexico (68.9%, n=28).
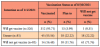
COVID-19 vaccine hesitancy was found among approximately 14% (n=455) of respondents, and varied significantly based on age, gender, race/ethnicity, previous COVID-19 infections, history of socializing in groups of 10 or more during the pandemic, symptoms of anxiety or depression over the course of the survey, number of years of practice as a dental hygienist, and primary practice setting. There was no statistically significant relationship between pre-disposing medical conditions for more severe COVID-19 infections and hesitancy to be vaccinated (X2 or Fisher p-values >0.05). The lowest rates of vaccine hesitancy were seen among Non-Hispanic Asians (5.7%, n=6), as well as among those 65+ (5.4%, n=9). The highest hesitancy rate was among those aged 26-39 years (22.5%, n=206) and individuals who had contracted COVID-19 (25.9%, n=112). Characteristics of the sample associated with COVID-19 vaccination and intention are shown in Table I.
Over the survey period of 9/28/20 to 10/8/20, respondents rated the degree to which they were concerned about COVID-19 transmission to themselves or patients. Both types of concerns were correlated to the participants who later chose to receive the COVID-19 vaccine. Those who indicated being significantly more concerned about COVID-19 transmission to themselves or patients were significantly less hesitant to get vaccinated (X2 p-value for concern for self: <.0001, X2 p-value for concern for patients: 0.001). Of the respondents who were highly concerned about transmission of a COVID-19 infection to themselves, 7.7% (n= 29) were vaccine hesitant, while 12.5% (n=32) of respondents who were moderately concerned and 19.4% (n=117) of those who were not very concerned about infection, indicated COVID-19 vaccine hesitancy. Of the respondents who were highly concerned about COVID-19 transmission to patients, 8.8% (n= 29) were hesitant to get vaccinated, while 13.9% (n= 39) of respondents who were moderately concerned, and 17.6% (n= 110) of those who were not very concerned, indicated vaccine hesitancy.
To account for differences in age, race/ethnicity, or other characteristics, a multi-variable logistic regression modeling on the final observation of each respondent was employed (Table II). Even controlling for all other factors, participants who had ever had a COVID-19 infection had statistically significant higher odds of being vaccine hesitant (aOR: 1.847, 95% CI:1.274, 2.678). Respondents who had socialized in groups of 10 or more between 1/4/21-8/16/21 also had statistically significant higher odds of being vaccine hesitant (aOR:1.550, 95% CI:1.151, 2.087). Respondents who displayed symptoms of anxiety or depression between 1/4/21 to 8/16/21, had statistically significant lower odds of being vaccine hesitant (aOR: 0.662, 95% CI: 0.456, 0.960).
Over the period of 2/1/21 to 2/6/21, respondents were asked whether they had encountered any barriers to being vaccinated; most respondents indicated no barriers (72.3% n= 829) while 27.7% (n= 317) experienced barriers. During the last month of the survey, 8/16/21 to 8/30/21, respondents who had been vaccinated were asked whether receiving the vaccine made them feel safer; 83.1% (n= 751) said yes and 8.3% (n= 75) said no, while 8.6% (n= 78) said they were unsure. Of the 75 who did not feel safer after the vaccination, 83.8% (n=61) were non-Hispanic white and 80.0% (n=60) were between 40-65 years old.
During the period of 1/4/21 to 1/8/21, the survey respondents were asked if the vaccine became available to them if they intended to get vaccinated: 68.1% (n= 1,063) answered yes, 17.8% (n= 278) answered no, and 14.0% (n= 219) answered maybe. When the stated intentions were compared with the reported vaccine status in the final observation for each participant, 25 of the respondents had changed their intentions. One respondent went from wanting to get vaccinated to being hesitant, while the other 24 changed from being vaccine hesitant to either being vaccinated or to planning on being vaccinated (Table III). Participants who changed their minds about receiving the vaccine had higher odds of having had COVID-19 (aOR:4.071, 95% CI:1.652, 10.030). No clear causative patterns emerged in the participants who changed from being vaccine hesitant to getting vaccinated or becoming willing to get the vaccine. Data were available on each of these participants for 2 to 8 months of the survey, an average of 3.88 months from 2/1/21 to 8/30/21. One-third (33.3%, n=8) indicated changing their minds about being vaccinated after being infected with COVID-19. None of these participants responded to the item asked from 8/16/21 to 8/30/21 regarding employers mandating the vaccine, so it is unknown if the change of mind was because vaccination was required for employment.
The most common reason respondents gave from 5/24/21 to 6/21/21 for the type of information needed to consider getting a COVID-19 vaccine was that they needed to see longer term studies or more research conducted (41.6%, n=87). The next most common reasons included the desire to wait for the full Food and Drug Administration (FDA) approval (12.0%, n=25) or the belief that since they had already had a COVID-19 infection that they were already immune (10.0%, n=21). A minority (5.3%, n=11) gave reasons based on misinformation, such as that there was no COVID-19 pandemic or that COVID-19 vaccines were more lethal than a COVID-19 infection. Lastly, 7.7% (n=16) desired more information on what a COVID-19 vaccination could mean for future fertility, current pregnancy, or breast feeding.
Discussion
This study of vaccine status indicates that there was vaccine hesitancy among dental hygienists during the period of the survey. Approximately 14% (n=455) of the dental hygienists in the study were vaccine hesitant, less than that of previous studies of the public, medical and dental students, and international dental students,13,18-20 and comparable to dentists.20,21 However, in an international study of nurses' intent to receive the COVID-19 vaccine once available, vaccine hesitancy was shown to be 37% of the participants (n=1,205); a level considered to be suboptimal to achieve herd immunity.24 Results from the current study indicate a high percentage of dental hygienists in the US are vaccinated, indicating a recognition of the high occupational risk related to clinical practice and the importance of disease prevention.
The highest rate of vaccine hesitancy was among younger individuals, those aged between 26-39 years. It may be that some of these individuals desired more information regarding the pandemic itself, vaccines in general, or issues related to pregnancy and breastfeeding. Seeking trusted and credible resources is an important consideration when gathering information about vaccines. Previous research has indicated that this age group tends to rely on social media for information, which may not provide evidence-based, current information19 The Centers for Disease Control and Prevention (CDC) has a variety of educational materials available for the public and health professionals related to COVID-19 and vaccines.25 More specifically, the CDC has a document that addresses COVID-19 vaccines during pregnancy, fertility problems and breastfeeding.25 Furthermore, many respondents may have felt more research needed to be conducted or they were waiting for full FDA approval before deciding upon vaccination. These concerns were expressed during the data collection in the spring 2021 and may have been better addressed as additional information about vaccines became available. It should be noted that the FDA approved COVID-19 vaccines during the latter part of August 2021,26 near the conclusion of this study.
It is of interest to note that there were respondents who expressed concern regarding the transmission of COVID-19 infections to patients yet were also hesitant to get vaccinated. In addition, those who indicated having had COVID-19, had contact with someone with the disease, or socialized in groups of 10 or more during the study period, had higher odds of being vaccine hesitant. These findings indicate a lack of understanding of virology, disease transmission, epidemiology, and the general benefits of vaccinations. Further education is needed to help dental hygienists appreciate these concepts to enable informed decision-making regarding immunization.
It is also of relevance that twenty states have authorized dental hygienists to administer COVID-19 vaccines.27 As vaccine administrators, dental hygienists must be cognizant of their responsibility to be knowledgeable regarding the disease and the vaccine. They should be capable of communicating with the public and their patients regarding the COVID-19 vaccine. The ADHA Code of Ethics supports efforts to promote public health and safety and create a work environment that minimizes health and safety risks.28 The CDC has provided resources for how to talk to patients about the COVID-19 vaccine focusing on embracing an attitude of empathy and collaboration, asking permission to discuss vaccination, using motivational interviewing, and responding to questions.29 Additional training may be essential for individuals who are vaccine hesitant, to help them achieve vaccine administrator status.
There were limitations to this study. All the results are based on self-report and are therefore subject to recall bias. Due to the potentially contentious or sensitive nature of COVID-19 vaccination status in the US, responses regarding vaccination rates may have been subject to social desirability bias. The overall survey had a response rate of 5.2% (n=6,976) indicating that the findings may be subject to response bias. However, it is not known how many of the 133,000 email addresses contacted were eligible, web-based surveys have lower response rates than other methods, and there were no incentives associated with this study; all of which may ameliorate the extent of this bias. Strengths of these findings include the wide representativeness of the sample, and the longitudinal nature of this research enables the explication of temporal relationships and thereby causality. Further study could explore dental hygienists' attitudes towards vaccination given the new variants of COVID-19 infections, FDA approval of vaccines and boosters, and vaccination mandates.
Conclusion
Results from this longitudinal study of dental hygienists in the US indicate the percentage of COVID-19 vaccination is high amongst these oral health care professionals, demonstrating recognition of the importance of vaccinations for the prevention and lowering risk of COVID-19 infection and disease severity. However, vaccine hesitancy remains an important consideration which must be addressed as dental hygienists are key prevention specialists who should promote adherence to vaccination programs for the health of the public. Further implementation of virology, epidemiology, and vaccination education is recommended.
Disclosures
The authors have no conflicts of interest to report. This research was funded by the American Dental Hygienists' Association and the American Dental Association.
Acknowledgements
The authors wish to thank all survey participants for generously sharing their thoughts and experiences.
JoAnn R. Gurenlian, RDH, MS, PhD, AFAAOM is the Director of Education and Research, American Dental Hygienists' Association, Chicago, IL, USA.
Laura A. Eldridge, MS is a Research Associate, Evidence Synthesis and Translation Research, American Dental Association Science & Research Institute, LLC, Chicago, IL, USA.
Cameron G. Estrich, MPH, PhD is a Health Research Analyst, Evidence Synthesis and Translation Research, American Dental Association Science & Research Institute, LLC, Chicago, IL, USA.
Ann Battrell, MSDH, is the Chief Executive Officer, American Dental Hygienists' Association, Chicago, IL, USA.
Ann Lynch is the Director of Advocacy, American Dental Hygienists' Association, Chicago, IL, USA.
Rachel W. Morrissey, MA is a Senior Research Analyst, Education and Emerging Issues, Health Policy Institute, American Dental Association, Chicago, IL, USA.
Marcelo W. B. Araujo, DDS, MS, PhD is the Chief Science Officer, American Dental Association, Science and Research Institute, Chicago, IL, USA.
Marko Vujicic, PhD is the Chief Economist and Vice President, Health Policy Institute, American Dental Association, Chicago, IL, USA.
Matthew Mikkelsen, MA is the Manager, Education Surveys, Health Policy Institute, American Dental Association, Chicago, IL, USA.
References
1. John Hopkins University of Medicine Coronavirus Resource Center. COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) [Internet]. Baltimore (MD): Johns Hopkins University; 2021 [cited 2021 Dec 14]. Available from: coronavirus.jhu.edu/map.html.
2. Cohen J. Vaccine wagers on coronavirus surface protein pay off. Science. 2020 Nov;370(6519):894-5.
3. Centers for Disease Control and Prevention. How CDC is making COVID-19 vaccine recommendations. Atlanta (GA): U.S. Department of Health and Human Services;2020 [updated 8/30/21] [cited 2021 Sept 17]. Available from: cdc.gov/coronavirus/2019-ncov/vaccines/recommendations-process.html.
4. World Health Organization. The power of vaccines: still not fully utilized. Geneva (SW): World Health Organization; 2017 [cited 2021 Sept 17}. Available from: who.int/publications/10-year-review/chapter-vaccines.pdf.
5. Home A, Powell D, Hummel JE, et al. Countering antivaccination attitudes. Proc Natl Acad SCI U S A. 2015 Aug; 112(33):10321-4.
6. Hornsey MJ, Harris EA, Fielding KS. The psychological roots of anti-vaccination attitudes. A 24-nation investigation. Health Psychology. 2018 Apr; 37(4):307-15.
7. World Health Organization. Ten threats to global health in 2019. Geneva (SW): World Health Organization; 2019 [cited 2021 Sept 17]. Available from: who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
8. MacDonald NE. SAGE working group on vaccine hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015 Aug; 33(34):4161-4.
9. Al-Sanafi-M, Sallam M. Psychological determinants of COVID-19 vaccine acceptance among healthcare workers in Kuwait: a cross-sectional study using the 5C and vaccine conspiracy beliefs scales. Vaccine. 2021 June; 9(7):701.
10. Fridman A, Gershon R, Gneezy A. COVID-19 and vaccine hesitancy: a longitudinal study. PLOS One. 2021 April; 16(4):e0250123.
11. Pogue K, Jensen JL, Stancil CK, et al. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines. 2020 Oct; 8(4):582.
12. Kreps S, Prasad S, Brownstein JS, et al. Factors associated with US adults' likelihood of accepting COVID-19 vaccination. JAMA Netw Open. 2020 Oct; 3(10): e2025594.
13. Khubchandani J, Sharma S, Price JH, et al. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. J Community Health. 2021 Apr; 42(2):270-7.
14. Mohanty A, Kabi A, Mohanty AP. Health problems in healthcare workers: A review. J Fam Med Prim Care. 2019 Aug; 8(8):2568-72.
15. Wheeler M, Buttenheim Am. Parental vaccine concerns, information source, and choice of alternative immunization schedules. Hum Vaccin Immunother. 2013 Aug; 9(8):1782-9.
16. Shekhar R, Sheikh AB, Upadhyay S, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. 2021 Feb; 9(2):119.
17. Lucia VC, Kelekar A, Afonso NM. COVID-19 vaccine hesitancy among medical students. J Pub Health (Oxf). 2021 Sep 22;43(3):445-9.
18. Kelekar AK, Lucia VC, Afonso NM, et al. COVID-19 vaccine acceptance and hesitancy among dental and medical students. J Am Dent Assoc. 2021 Aug;152(8): 596-603.
19. Riad A, Abdulqadar H, Morgado M, et al. Global prevalence and drivers of dental students' COVID-19 vaccine hesitancy. Vaccines. 2021 May; 9(6): 566.
20. Belingheri M, Roncalli M, Riva, MA, et al. COVID-19 vaccine hesitancy and reasons for or against adherence among dentists. J Am Dent Assoc. 2021 Sept; 152 (9): 740-6.
21. Shacham M, Greenblatt-Kimron L, Hamama-Raz Y, et al. Increased COVID-19 vaccination hesitancy and health awareness amid COVID-19 vaccinations programs in Israel. Int J Environ Res Public Health. 2021 Apr; 18(7):3804.
22. Estrich CG, Gurenlian JR, Battrell A, et al. COVID-19 prevalence and related practices among dental hygienists in the United States. J Dent Hyg. 2021 Feb; 95(1):6-16.
23. Gurenlian JR, Morrissey R, Estrich CG, et al. Employment patterns of dental hygienists in the United States during the COVID-19 pandemic. J Dent Hyg. 2021 Feb; 95(1):17-24.
24. Kwok KO, Li K-K, Wei WI, et al. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021 Feb; 114:103854.
25. Centers for Disease Control and Prevention. COVID-19 vaccines while pregnant or breastfeeding [Internet]. Atlanta (GA): Centers for Disease Control and Prevention; 2021 [cited 2021 Oct 29]. Available from: cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/pregnancy.html.
26. U.S. Food and Drug Administration. FDA approved first COVID-19 vaccine. Silver Spring, (MD): US Food and Drug Administration; 2021[cited 2021 Dec 14]. Available from: fda.gov/news-events/press-announcements/fda-approves-first-covid-19-vaccine.
27. American Dental Hygienists' Association. Covid-19 vaccine administration by dental hygienists. Chicago (IL): American Dental Hygienists' Association; 2021 [cited 2021 Oct 29]. Availablefrom:adha.org/resources-docs/COVID-19_Vaccine_Administration_by_DH_5_5_2021.pdf.
28. American Dental Hygienists' Association. Code of Ethics [Internet]. Chicago (IL): American Dental Hygienists' Association; 2021[cited 2021 Oct 29]. Available from: adha.org/resources-docs/ADHA_Code_of_Ethics.pdf.
29. Centers for Disease Control and Prevention. Talking with patients about COVID-19 vaccination [Internet]. Atlanta (GA): Centers for Disease Control and Prevention; 2021 [cited 2021 Oct 29]. Available from: cdc.gov/vaccines/covid-19/hcp/engaging-patients.html.