The ADAA has an obligation to disseminate knowledge in the field of dentistry. Sponsorship of a continuing education program by the ADAA does not necessarily imply endorsement of a particular philosophy, product, or technique.
Whether for exercise, competition, or the simple enjoyment of recreational activity, increasing numbers of health-conscious Americans are involved in sporting activities.1 Approximately 20 million children participate in various sports programs in the United States and another 80 million are involved in unsupervised recreational sports.2
In addition, 15 million Americans suffer dental injuries and 5 million teeth are lost annually in sports-related injuries. During a single athletic season, athletes have a 1 in 10 chances of suffering a facial or dental injury. In fact, the lifetime risk of such an injury is estimated to be about 45% according to the National Youth Sports Foundation.41 Dentistry plays a large role in treating oral and craniofacial injuries resulting from sporting activities.
Prior to the 1980’s, little was available in the scientific literature in terms of sports-related injury assessment. Several injury surveillance systems have been established in an attempt to track sports-related accidents and injuries. While all injury surveillance systems provide valuable information on generalized sports injuries, very little information is available regarding dental or craniofacial injuries. In terms of data collection and analysis, the field is open for dentistry to assume a major leadership role in assessing dental injuries resulting from sporting activities.3 One reason for such lack of scientific studies regarding this issue is the absence of academic training in sports dentistry. A survey by Kumamoto and others was sent to 69 dental schools in the United States and Canada regarding course offerings, opinions about offering a course, construction of mouthguards, and provision of treatment for trauma. Of the 19 dental schools with sports dentistry courses, 17 taught the course in the undergraduate curriculum, 12 as a required course and the remaining 5 as an elective. Two schools offered the course on a graduate level. Data from the study also concluded that more than half of the schools that teach sports dentistry do not treat any outside athletic group on a regular basis.4
This course is designed to explain the various sports-related dental injuries, discuss the three types of mouthguards utilized and the dental team’s role in sports-related injuries and sports dentistry.
Statistics
More than 5 million teeth are avulsed each year; many during sports activities, resulting in nearly $500 million spent on replacing these teeth each year.1 In an issue of the Journal of the American Dental Association (JADA) it was reported that 13-39% of all dental injuries are sports-related, with 2-18% of the injuries related to the maxillofacial. Males are traumatized twice as often as females, with the maxillary central incisor being the most commonly injured tooth. Studies of orofacial injuries published over the last thirty years reflects various injury rates dependent on the sample size, the age of participants, and the specific sports.30-31 Even in football, a sport requiring protective gear, only about 75% of athletes are in compliance. In soccer, where rules are not uniform on wearing mouthguards, only 7% of the participants wear them.1 In baseball and softball, again only 7% wear mouthguards. Recent studies show basketball had the highest injury rate with both male and female students due to hand or elbow contact or by collision with other players. The close contact of basketball players, as well as the speed of the game increases the potential for possible orofacial trauma.37 Currently, the National Federation of State High School Associations mandates mouthguards for only four sports: football, ice hockey, lacrosse, and field hockey.32 The National Federation of State High School Associations (NFHS) requires the use of properly fitted mouthguards in only 5 sports (field hockey, football, ice hockey, lacrosse, and wrestling [the last if the athlete wears braces or an orthodontic device]) and the National Collegiate Athletic Association (NCAA) mandates them in only 4 sports (field hockey, football, ice hockey, and lacrosse).32
Although not all sports require mouthguard use, a meta-analysis indicated that participants not wearing mouthguards (as is typical in non–mouthguard-mandated sports) were 1.6 to 1.9 times more likely to sustain an orofacial injury than participants who wore mouthguards.43
However, many high school and college administrators continue to support mandatory protective equipment relating to many more high school contact sports.29 It is evident from past research studies there is a need for more research on the topic of sports dentistry. There is also a need to educate communities of interest including more regulations for mouthguard use in sports.
In 1962, high school and collegiate football players were required to wear faceguards and mouth protectors during practice sessions and in competition. Several studies confirm that since this requirement, the percentage of orofacial injuries in football has dropped from approximately 50% to one-half of 1%, depending on the study cited.
The American Academy of Pediatric Dentistry recommends a mouthguard for all children and youth participating in any organized sports activities. The American Dental Association (ADA) recommends wearing a mouthguard for all of the following sports listed in .
A study conducted on high school varsity basketball teams in Florida assessed the benefit of mouthguard use in sports other than football. It was found that 31% of surveyed Florida varsity basketball players sustained orofacial injuries during the season. 53% reported more than one injury during the season. Of the 1,020 players, fewer than half wore mouthguards and only 2 of these sustained oral injuries not requiring professional attention during the season.5 It was concluded by the authors that there is a high risk of orofacial injury competing in basketball without a mouthguard, which would increase a player's chance of orofacial injury almost sevenfold.6 Soporowski and others found that of all the injuries presented to dental offices, 62% occurred while the patient was participating in an unorganized sport. Children between the ages of seven and ten have the highest number of injuries (59.6%). Baseball had the most injury sites, 72 of 159 injuries, biking followed with 59, and hockey and basketball were third and fourth respectively.7 Another study was conducted with 3,411 athletes. The highest incidence of orofacial injury for the male athletes was noted in wrestling and basketball. For females, it was basketball and field hockey. None of the athletes who sustained an injury was wearing a mouthguard.4
A study conducted on high school athletes, in which researchers interviewed 2,470 junior and senior high school football players, showed 9% of all athletes sustained some form of orofacial injury with 3% reporting loss of consciousness. Fifty-six percent of all concussions and 75% of all orofacial injuries occurred while the athlete refrained from mouthguard protection.4 In Alabama, a study on 754 football players revealed that 52% of all orofacial injuries occurred in sports other than organized football. Basketball, baseball and unorganized football were a few of the sports which showed a high incidence of oral trauma and concussions when mouthguards were not used.4 Morrow and Kuebker conducted surveys in selected Texas high schools to determine the incidence of orofacial injuries on approximately 122,000 male and female athletes. They measured the types of mouthguards worn and dental injury experienced in football, and later indicated that soccer and basketball had higher dental injury rates than football. The number and nature of dental injuries experienced by male athletes showed that lip and tongue lacerations were the most frequently reported injuries. In addition, fourteen jaw fractures were reported with as many fractures in baseball and soccer as there were in football.8
All athletes constitute a population that is extremely susceptible to dental trauma. Dental injuries are the most common type of orofacial injury. An athlete has a 10% chance of receiving an orofacial injury every season of play. In addition, athletes have a 33-56% chance of receiving an orofacial injury during their playing career.
Common Athletic Injuries
Soft Tissue Injuries
The face is often the most exposed part of the body in athletic competition and injuries to the soft tissues of the face are frequent. Abrasions, contusions, and lacerations are common and should be evaluated to rule out fracture or other significant underlying injury.10 These usually occur over a bony prominence of the facial skeleton such as the brow, cheek, and chin. Lip lacerations are also common.11
Fractures of the Bone
Fractures of the facial bones present an even more complex problem. The most frequent site of bony injury is the zygoma (cheekbone). Fractures of the zygoma account for approximately 10% of the maxillofacial fractures seen in sports injuries, occurring as a result of direct blunt trauma from a fall, elbow, or fist.12 In a study by Linn and others, of the 319 patients treated for sports-related injuries, males proved to be more prone to zygomatic fractures than females because of the powerful physical contacts during sports.13 Like the zygoma, the prominent shape and projection of the mandible cause it to frequently be traumatized. Approximately 10% of maxillofacial fractures from sporting activities occur in the mandible when the athlete strikes a hard surface, another player, or equipment. In a mandibular fracture, airway management is the most important aspect of immediate care.14 In both children and adults, the condyle is the most vulnerable part of the mandible. Fractures in this region have the potential for long-term facial deformity. Recent data suggest that condylar fractures in children can alter growth of the lower face.11
TMJ Injuries
Most blows to the mandible do not result in fractures, yet significant force can be transmitted to the temporomandibular disc and supporting structures that may result in permanent injury ( and ). In both mild and severe trauma, the condyle can be forced posteriorly to the extent that the retrodiscal tissues are compressed. Inflammation and edema can result forcing the mandibular condyle forward and down in acute malocclusion. Occasionally this trauma will cause intracapsular bleeding, which could lead to ankylosis of the joint.
Tooth Intrusion
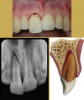
Tooth intrusion occurs when the tooth has been driven into the alveolar process due to an axially directed impact (). This is the most severe form of displacement injury. Athletes with intrusively luxated teeth should be immediately removed from play and transported to a sports emergency dentist.44
Pulpal necrosis occurs in 96% of intrusive displacements and is more likely to occur in teeth with fully formed roots. Immature root development will usually mean spontaneous re-eruption. Mature root development will require repositioning, surgery, and splinting or orthodontic extrusion. Treat relatively quickly since the pulp usually becomes necrotic - this can be treated with temporary filling of calcium hydroxide paste followed by root canal therapy.
Tooth Extrusion
The tooth is displaced partially out of the socket by the trauma (). It is usually displaced palatally. The athlete should then be asked to bite down on a sterile gauze pad to temporarily splint the tooth in preparation for transport. Immediate removal from participation and referral to a trauma-ready dentist or emergency facility.44
Radiographically the tooth appears dislocated and empty at the end of the socket. Treatment is to try to reposition gently - local anesthetic is usually not needed. Check the occlusion to be sure there is no pressure on the tooth and use a non-rigid splint for two weeks. The dentist should periodically monitor the vitality of the pulp and perform root canal therapy if needed.
Crown and Root Fractures
Crown fractures () are the most common injury to the permanent dentition and may present in several different ways. The simplest form is crown infraction. This is a crazing of enamel without loss of tooth structure. It requires no treatment except adequate testing of pulpal vitality.14 Fractures extending into the dentin are usually very sensitive to temperature and other stimuli. The most severe crown fracture results in the pulp being fully exposed and contaminated in a closed apex tooth or a horizontal impact may result in a root fracture. The chief clinical sign of root fracture is mobility. Radiographic evaluation and examination of adjacent teeth must be performed to determine the location and severity of the fracture as well as the possibility of associated alveolar fracture.12 Treatment is determined by the level of injury. If the tooth fragment can be located at the scene, it should be placed in a liquid such as water, saline, or milk and sent with the athlete to the dentist.45
Avulsion
Certainly, one of the most dramatic sports-related dental injuries is the complete avulsion of a tooth (). Two to sixteen percent of all injuries involving the mouth result in an avulsed tooth. A tooth that is completely displaced from the socket may be replaced with varying degrees of success depending largely on the length of time the tooth is outside the socket. If the periodontal fibers attached to the root surface have not been damaged by rough handling, an avulsed tooth may have a good chance of recovering full function. After one hour, the chance for success is greatly diminished. Statistics show that the patient can have a 90% success rate if the tooth is placed back in the socket within twenty minutes. Success decreases 10% for each additional 5 minutes that the tooth is out of the socket.42 The fibers become necrotic and the replaced tooth will undergo resorption and ultimately be lost.11
To prevent additional trauma to the periodontal ligament (PDL), the athlete, parent, coach, or athletic trainer should refrain from handling the tooth by its root, brushing or scrubbing debris from the tooth,or sterilizing the tooth with boiling water or chemicals.46,47 If visible debris is on the tooth surface, the AT or other health care professional can gently rinse (for a maximum of 10 seconds) the surface under a gentle flow of a cold water, milk, or physiologic saline.46,47 Once the tooth has been replanted, the athlete should bite down on a sterile gauze pad to stabilize it before being immediately transported to a trauma-ready dentist for definitive treatment.46 If the avulsed tooth cannot be replanted immediately and completely, the tooth should be submerged in a storage medium to prevent the PDL cells from drying. Hanks’ Balanced Salt Solution is the optimal storage medium for avulsed teeth. However, cold low-fat milk is an acceptable alternative. An avulsed tooth should not be wrapped in dry gauze or a dry paper towel.48,49
Emergency Treatment
Due to the high incidence of sports-related dental injuries, it is vital that primary health care providers such as school nurses, athletic trainers, team physicians and emergency personnel are trained in the assessment and management of dental injuries. Interested dental team members can assist these providers by offering to speak to schools, so that the primary health care providers who will deliver immediate treatment at sporting events understand the proper protocol for orofacial injuries, such as displaced teeth, avulsed teeth, lacerations, and crown fractures. The ADA has urged its members to work together with schools, colleges, athletic trainers and coaches to develop mouthguard programs and guidelines to prevent sports injuries.
The main method for preventing orofacial injuries in sports is the wearing of mouthguards and headgear, consisting of a helmet and face protector. Yet, a study by the National Institute of Dental Research reported that children do not consistently wear mouthguards and headgear during organized sports. Even in football, a sport that requires the use of mouthguards, as earlier noted, only about 75% of students are in compliance.15
Parental perceptions of children's risks to injury, expenses associated with protective gear, and peer pressure may influence use of mouthguards. Interestingly, lower socioeconomic parents are reported to be more aware of threats to their children's safety than are affluent parents.16 The observed patterns of mouthguard wearing by males and females can represent cultural differences, peer pressure, and/or nature of sports played, including the following:
| 1. |
Perceptions that females are less aggressive and thus, a reduced risk of injury may exist, |
| 2. |
Perceptions regarding the absence of long-term commitment to a sport may result in a differential willingness to devote resources to females, |
| 3. |
Aesthetic appeal may influence protective orofacial gear usage, |
| 4. |
Females may play in non-league-based sports with fewer or less stringent rules or may play less combative sports than males.15 |
These perceptions are flawed. The literature indicates the use of mouthguards by athletes is most influenced by their coaches.17 However, studies indicate mouthguard compliance by athletes is usually not insisted upon by their coaches or referees.35 Coaches may feel that they do not have sufficient knowledge of mouthguards. Coaches report most information about mouthguards comes from sales representatives (72%), educational materials (33%), and dentists (11%).18
In 1995, the ADA House of Delegates revised their policy recognizing "the preventive value of orofacial protectors" and endorsed their use "in sports activities with a significant risk of injury at all levels of competition."19
Mouthguards
When athletes are surveyed as to why they don't wear mouthguards, results indicate participants believe their mouthguards will affect their breathing. However, Rapisura, Coburn, Brown, and Kersey recently tested two types of mouthguards with female athletes and found there was no effect on aerobic performance with their subjects with either the custom or prefabricated mouthguards they tested.34
When considering recommendations, an ideal mouthguard should follow the following recommendations outlined by the Academy for Sports Dentistry (ASD):
The fitting of a mouthguard is best accomplished under the supervision or direction of a dentist. The athlete and/or parents should always be advised of the special design for the "properly fitted mouthguard" and the end product should have the following properties and considerations:
| • |
It should be fabricated to adequately cover and protect both the teeth in the arch, and the surrounding tissues. |
| • |
It should be fabricated on a stone model taken from an impression of the athlete. |
| • |
Adequate thickness in all areas to provide for the reduction of impact forces. In particular, a minimum of 3mm thickness in the occlusal/labial area. |
| • |
It should have a seated equilibrated occlusion that is balanced for even occlusal contact. This helps to provide for the ideal absorption of impact energy. |
| • |
A fit that is retentive and not dislodged on impact. |
| • |
Speech considerations equal to the demands of the playing status of the athlete. |
| • |
A material that meets FDA approval. |
| • |
In addition, a properly fitted guard should provide protection and be fabricated to fit on the leading arch.38 |
The properly fitted mouthguard should be routinely and professionally examined for fit and function. Frequency of routine inspection is dependent on factors such as the athlete's age, the demand of the sport that the athlete is engaged in, and the willingness for the athlete to properly care for the appliance. The frequency of the inspection should be determined by the dental professional for each individual situation and athlete.
Mouthguards typically are made of thermoplastic copolymer and designed to fit over occlusal and facial surfaces of the maxillary teeth and gingival tissues.36 The American Society for Testing and Materials and the manufacturers of mouthguards have classified the mouthguards into three types:
Stock Mouthguards Type III
Stock mouthguards () may be purchased from a sporting goods store, pharmacy, or a department store. They are made of rubber, polyvinyl chloride or a polyvinyl acetate copolymer.21 The advantage is that this mouthguard is relatively inexpensive, but the disadvantages far outweigh the advantages. They are available only in limited sizes, do not fit very well, inhibit speech and breathing, and require the jaws to be closed to hold the mouthguard in place.22 Because the stock mouthguards do not fit well, the player may not wear the mouthguard due to discomfort and irritation. Orthodontists will often recommend these because they allow for protection of soft tissues while allowing tooth movement. In doing so, the ASD feels that they do not allow for adequate protection of the teeth. The ASD has stated that the stock mouthguard is unacceptable as an orofacial protective device.23
Mouth-Formed Protectors Thermosetting Type II
There are two types of mouth-formed protectors: the shell-liner and the thermoplastic mouthguard (). The shell-liner type is made of a preformed shell with a liner of plastic acrylic or silicone rubber. The lining material is placed in the player's mouth and molds to the teeth and then is allowed to set. The preformed, thermoplastic type also has a lining that is immersed in boiling water for 10-45 seconds, transferred to cold water and then adapted to the teeth (also known as "boil and bite guard"). This mouthguard seems to be the most popular of the three types and is used by more than 90% of the athletic population.24
Custom Made Mouthguards Thermoplastic Type 1
This is the superior of the three types and the most expensive to the athlete. Dental professionals believe this to be well worth the cost to protect an athlete's teeth from injury. Most parents will spend quite a bit of money on athletic shoes, but might not think about protecting their child's teeth. This mouthguard is made of thermoplastic polymer and fabricated over a model of the athlete's dentition.21 The mouthguard is made by the dentist and fits exactly to the athlete's mouth. The advantages include fit, ease of speech, comfort and retention.20 By wearing a protective mouthguard, the incidence of a concussion by a blow to the jaw is significantly reduced because the condyle is separated from the base of the skull by placing the mandible in a forward position.25
There are two types of custom mouthguards. The most common is a Custom Vacuum Formed Mouthguard (), which is classified as a Class 1. This is the most widely made mouthguard by the dental profession. It offers good protection with the least interference to speaking and breathing. They are fabricated from a single sheet of EVA polyvinyl acetate-polyethylene copolymer. The EVA sheet is heated, placed over the stone model, and suctioned by vacuum to fit to the shape of the mouth and teeth.
Vacuum formed mouthguards have been found to decrease in thickness occlusally by 25%, while the buccal and lingual surfaces can be by more than 50%.40
They have been found to retain their shape for only a few weeks after wearing. They will not provide protection for long periods of time and should be closely monitored.
The other type of custom mouthguards are Pressure-Laminated Mouthguards (), which are classified as Class 2. They are considered to be the best mouthguards available. They are made of multiple sheets of laminating EVA materials that are heated, placed over a stone model, and pressed onto the model or previous laminate with a maximum pressure of 6 atmospheres.
Multiple layers can be fused together to form an adequately thick and protective mouthguard allowing for precise adaptation due to increased pressure. This allows them to remain in place better during sport activity. They allow for a more balanced occlusion and show negligible deformation when worn for prolonged periods of time. There is little to no elastic memory when high heat is combined with high pressure during fabrication. These mouthguards are typically made by dentists or dental laboratories.
In summary, custom pressure-laminated mouthguards allow for effective communication. Interference with breathing is minimized and they show less wear in chewing and biting. They are more comfortable to wear and so are worn more regularly by participants. The laminating machines have 10x the pressure of vacuum systems.
Since pressure is even throughout, it allows for a uniform thickness of guard material.
Pressure-laminated mouthguards are substantially superior to all other types (). They are the only type that can be counted on to offer the best protection for our children's teeth during all types of sporting activities.39
Dental Team's Role
Dentists need to educate patients on the need and benefits of protective devices. The American Dental Association (www.ada.org) publishes brochures, which explain the different types of mouthguards and their advantages. The National Youth Sports Safety Foundation, a non-profit educational research organization working to promote the safety of youth in sports, has published a fact sheet on dental injuries that includes statistics, costs of injuries, resource information regarding standards for mouthguards, videos, and mouthpieces and dental care.9 A field emergency kit is a simple and inexpensive item for the dentist attending a sporting event (see Emergency kit list, ).
"Fitting mouthguards is a perfect activity for a dental society," says Robert Morrow, D.D.S., Professor of Prosthodontics, University of Texas-San Antonio Dental School. "You simply get a group of dentists together at the school and begin making impressions. It spreads out the costs and cuts down on the time. And it's worthwhile."2 "It's a great practice builder," says Robert Donnelly, D.D.S., a general practitioner in San Marcos, Texas, and dentist for the Southwest Texas State University football team. "I don't charge for my time or the materials to make a mouthguard. I do it for free. As a result, we get a lot of referrals."22
Due to the increasing participation in sporting events by children of all ages, a need for mouthguard implementation is of extreme importance. Dental professionals need to develop effective ways of conducting research to determine the prevalence of sports-related injuries in their communities.
By combining research with preventive efforts, legislation can be determined. Mouthguard laws would help to reduce the number of orofacial sporting injuries and protect athletes. The sports dentistry field is a challenging yet rewarding one. With efforts from dentists and dental auxiliaries in the country, a better awareness of the types of injuries, treatment procedures, and mouthguard prevention can be conveyed to parents and athletes.
The role as dental assisting professionals should include:
| • |
Good impression techniques and knowledge of mouthguard materials/manipulations in mouthguard creation. |
| • |
Communications with children and parents/guardians. Dental charting should include questions about involvement in sports and the use of mouthguards. If patients are unwilling or unable to pay for an office-made guard, the dental assistant should educate patients about affordable boil and bite-type guards for minimal protection. |
| • |
Basic instructions on emergency treatments of dental emergencies such as avulsions, fractures, extrusions and intrusions that an adult can perform immediately until dental treatment can be attained.33 |
Sports dentistry should encompass much more than mouthguard fabrication and the treatment of fractured teeth. As dental professionals, a responsibility exists to become and remain educated and pass that education on to the community regarding the issues related to sports dentistry and specifically to the prevention of sports-related oral and maxillofacial trauma. Organizations such as the Academy for Sports Dentistry (www.sportsdentistry.org), which was founded in 1983, contribute to overall efforts to eliminate dental injuries in sporting activities. The ASD conducts educational programs, publishes a biannual newsletter, offers an annual symposium for dentists and other health professionals interested in trauma and preventive therapy, and promotes legislative efforts and encourages research in all dentally-related sports issues.3
Summary
With the many sports that children play, such as soccer, basketball, football, baseball, and all kinds of skating, it is recommended that dentists fabricate mouthguards for all patients - especially children who participate in organized and unorganized sports. Dentistry should be working diligently to require mandatory use of mouthguards in all sports, which starts at the local and state levels.
GLOSSARY
ankylosis - abnormal fusion of the tooth with the bone (joining together)
avulsed - entire tooth is knocked out
axially - referring to the long axis of the tooth
condyle - the posterior bony process that extends up from the mandible
crazing - to become covered with fine cracks
edema - swelling
extrusion - tooth is partially forced out due to injury or purposeful orthodontic treatment
intrusion - tooth is driven into the alveolar process
malocclusion - the contact between the maxillary and mandibular arches, whereby the positioning of the teeth is not in accordance with the usual rules of anatomic form
mobility - state of the tooth being mobile
necrotic - death of living tissue
pulpal necrosis - death of pulpal tissue
sports dentistry - involves the prevention and treatment of orofacial athletic injuries and related oral diseases, as well as the collection and dissemination of information on dental athletic injuries and the encouragement of research in the prevention of such injuries
RESOURCES
| • |
See the Academy for Sports Dentistry website for specific emergency treatment instructions http://www.academyforsportsdentistry.org and http://www.academyforsportsdentistry.org/assets/docs/Treatment_Cards/emergency_treatment_card_english.pdf |
| • |
The American Academy of Pediatric Dentistry website provides information relating to avulsed teeth recommendations for dental professionals called the Decision Tree for an Avulsed Tooth. |
| • |
The website of the International Association of Dental Traumatology has a Dental Trauma Guide. This information can be accessed by going to: http://www.dentaltraumaguide.org |
REFERENCES
1. Olin, W.H. Dentistry and Sport, Meeting the Needs of Our Patients. JADA, June 1996, 127:809-18.
2. Smith, C. The Sporting Life. AGD Impact, 1989:4-8.
3. Elliott, M.A. Professional Responsibility in Sports Dentistry. Dental Clinics of North America, Oct 1991, 35(4):831-40.
4. Kumamoto, DP. Sports Dentistry at the State Level. JADA, June, 1996, 127(6):816.
5. Koch, T., Moavenian, N., Parker, J., Waston, M., Westfall, A. The Use of Mouthguards in High School Contact Sports. U of M School of Dentistry, Class of 1996. Medline Site.
6. Flanders, R.A. The Incidence of Orofacial Injuries in Sports: A Pilot Study in Illinois. JADA. Apr 1995, 126(4):491-6.
7. Soporowski, N.J. Survey of Orofacial Sports-Related Injuries. J Mass Dent Soc., Fall 1994, 43(4):16-20.
8. Morrow, R., Kuebker, W. Sports Dentistry: A New Role. Dent Sch Q (D96), 1986, 2(2):11-13.
9. Glassman, M. The First Line of Defense. NYSDJ, Aug-Sept, 1995:48-50.
10. Crow, R.W. Diagnosis and Management of Sports-Related Injuries to the Face. Dental Clinics of North America, Oct 1991, 35(4):719-732.
11. Guyette, R.F. Facial Injuries in Basketball Players. Clinics of Sports Medicine. April 1993, 12(2):247-263.
12. Padilla, R., Balikov, S. Sports Dentistry: Coming of Age in the ‘90s. CDA Journal, April, 1993:27-37.
13. Linn, E.W., Matthijs, M.A., Virjhoef, J.R., De Wijn, R.P., Coops, H.M., Cliteur, B.F., Meerloo, R. Facial Injuries Sustained During Sports and Games. J Max-fac Surg, 1986, 14:83-88.
14. Camp, J.H. Diagnosis and Management of Sports-Related Injuries to the Teeth. Dental Clinics of North America, Oct 1991, 35(4):733-756.
15. Nowjack-Raymer, R., Gift, HC. Use of Mouthguards and Headgear in Organized Sports by School-aged Children. Public Health Reports, 1996, 3:82-6.
16. Glik, D., Kronenfeld, J., Jackson, K. Predictors of Risk Perceptions of Childhood Injury Among Parents of Pre-schoolers. Health Educ Q, 1991, 18:285-301.
17. Ranalli, DN., Lancaster, DM. Attitudes of College Football Officials Regarding NCAA Mouthguard Regulations and Player Compliance. J Public Health Dent, 1993, 53:96-100.
18. DeYoung, A., Godwin, W., Robinson, E. Comparison of Comfort and Wearability Factors of Boil-and-Bite and Custom Mouthguards. Abstract 1390. J Dent Res, 1993, 72:277.
19. Winters, JE. Sports Dentistry, the Profession's Role in Athletics. JADA, June, 1996, 127(6):810-1.
20. Kopp BP. All Mouthguards are Not Created Equal. Laboratory Digest, Fall, 1996:1.
21. American Dental Association. Mouth Protectors and Sports Team Dentists. JADA, July, 1984, 109:84-7.
22. Kerr, IL. Mouthguards for the Prevention of Injuries in Contact Sports. Sports Medicine, 1986:415-427.
23. Flanders, RA. Mouthguards and Sports Injuries. Illinois Dental Journal, Jan-Feb, 1993:13-6.
24. McCarthy, MF. Sports and Mouth Protection. Gen Dent, Sept-Oct, 1990, 38(5):343-46.
25. Padilla, RR. Sports in Daily Practice. JADA, June, 1996, 127:815-6.
26. Unknown. JADA, July 2004, 135:1061.
27. American Dental Association. Dentists, Pediatricians Urge Mouthguard Use as Kids Head Back to School, August 9, 2005
www.ada.org.
28. American Academy of Pediatric Dentistry. Policy on Prevention of Sports-Related Orofacial Injuries 2006
www.aapd.org.
29. Tesini, DA., Soprowski, NJ. Epidemiology of Orofacial Sports-Related Injuries. Dent Clin North Am 2000;44:1-18.
30. Kumamoto, D., Maeda, Y. Global Trends and Epidemiology of Sports Injuries. J Pediatr Dent Care 2005;11(2):15-25.
31. Kumamoto, D., Maeda, Y. A Literature Review of Sports-Related Orofacial Orofacial Trauma. Gen Dent 2004; 52:270-280.
32. Klossner D, ed. 201314 NCAA Sports Medicine Handbook. 24th ed. Indianapolis, IN: The National Collegiate Athletics Association; 2013.
34. Rapisura, KP., Coburn, JW., Brown, LE., Kersey, RD. Physiological Variables and Mouthguard Use in Women During Exercise. J Strength Cond Res, May 2010, 24(5):1263-8.
35. Ranalli, DN. Dental Injuries in Sports, Cur Sports Med Reports, 2005, 4:12-17.
36. ADA Council on Access, Prevention, and Interprofessional Relations; ADA Council on Scientific Affairs. Using Mouthguards to Reduce the Incidence and Severity of Sports-related Oral Injuries. JADA, December, 2006, 137;1712-1720.
37. Cohenca N., Roges RA., Roges, R. JADA, August 2007, 138;1121-1126.
38. Position Paper on a Properly Fitted Mouthguard Approved by the Academy for Sports Dentistry Board of Directors 04/05/2010.
39. Padilla, R. Twenty-fifth Annual Symposium of the Academy for Sports Dentistry 2006.
40. Park, First International Symposium on dental Materials, August 1993.
41. American Dental Association, Council on Dental Materials, Mouth Protectors and Sports Team Dentists, JADA 1984 109.84-7.
42. Andreasen FM, Andreasen JO. Avulsions. In: Andreasen JO, Andreasen FM, Andersson L, (eds.). Textbook and Color Atlas of Traumatic Injuries to the Teeth (4th ed.). Oxford, Blackwell 2007. 444-488.
43. Knapik JJ, Marshall SW, Lee RB, et al. Mouthguards in sport activities: history, physical properties, and injury prevention effectiveness. Sports Med. 2007;37(2):117–144
44. National Athletic Trainers’ Association Position Statement: Preventing and Managing Sport-Related Dental and Oral Injuries Journal of Athletic Training 2016;51(10):821–839 doi: 10.4085/1062-6050-51.8.01
45. Flores MT, Andreasen JO, Bakland LK, et al. Guidelines for the evaluation and management of traumatic dental injuries. Dent Traumatol. 2001;17(3):97–102.
46. Flores MT, Andreasen JO, Bakland LK, et al. Guidelines for the evaluation and management of traumatic dental injuries. Dent Traumatol. 2001;17(5):193–198.
47. Trope M. Clinical management of the avulsed tooth: present strategies and future directions. Dent Traumatol. 2002;18(1):1–11
48. Harkacz OM, Carnes DL, Walker WA. Determination of periodontal ligament cell viability in oral rehydration fluid, Gatorade, and milks of varying fat content. J Endod. 1997;23(11):687–690.
49. Sigalas E, Regan JD, Kramer PR, Witherspoon DE, Opperman LA. Survival of human periodontal ligament cells in media proposed for transport of avulsed teeth. Dent Traumatol. 2004;20(1):21–28.
About the Author
UPDATED IN 2017:
Rick Knowlton, DMD, MAGD
Rick Knowlton DMD, MAGD, is the 2013-2014 President of the Academy for Sports Dentistry. He practices general and esthetic dentistry in Elizabethtown, Pa. and is the team dentist for numerous local sports teams and lectures on Sports Dentistry and related topics.
ORIGINAL AUTHORS: Connie Kracher, Ph.D, MSD and Wendy Schmeling Smith, RDH, B.S.Ed.