You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Dental patients are looking for guidance regarding their own smiles. Once the patient understands and accepts that their terminal smile must be treated with partial or full mouth extraction, then the responsibility is back on the doctor to provide options for removable dental appliances or other alternative therapies. Providing dentures for dental patients may seem simple, but when the denture does not fit well and the patient is dissatisfied, their dentist is often seen as 100% responsible for this outcome. This article is a review of anatomical considerations and field judgements within the denture fabrication appointments.
Patient Requests and Attitudes
Patients may not always be able to articulate exactly what they want with the fit of their existing dentures or know what they want when moving forward with extractions and receiving a new denture(s). The clinician's explanation to the patient should be simple and concise. The retention of a denture is determined by its resistance to movement away from the tissue. Maximum tissue coverage routinely increases the factors of retention.1Regarding stability, the quality of the denture that resists movement of the prosthesis in a horizontal direction. Finally, support is determined by the denture that resists movement toward the tissue.2,3
The patient's attitude can help a clinician in the delivery of information and educate the patient understand what the steps are in order to create a new smile with a removable prosthesis. The four most common personalities or attitudes of patients are as follows.4 Hysterical personality is characterized by superficiality, egocentricity, vanity, dependence, and manipulation, as shown by dramatic, reactive, and intensely expressed emotional behavior. A dentist best be attentive to this type of personality and be clear. A person with an exacting personality expects things to be precise. For this reason, the exacting patient can generally be thought of as demanding. They will be sure express their displeasure when you are late or if the set up must be returned to the laboratory for reset. Indifferent patients are apathetic and do not express much interest or concern, for example, towards differences in tooth shade. They show no bias, prejudice, or preference, and therefore it can be very difficult to know if the patient is pleased or not. A philosophical patient shows a calm attitude toward disappointments of difficulties. They understand that their smile is terminal and deal calmly with the steps necessary to the process of denture fabrication.
Impressions
There are differences in what is required of a diagnostic cast for a patient who is retaining teeth versus one for a complete denture patient.5 Diagnostic casts with inaccurate or partially missing vestibules are often acceptable when creating a treatment plan for the routine dental patient. The goal is to capture soft and hard tissues for dentate and edentulous patients. Diagnostic casts for the latter should incorporate all the vestibules present and have accurate extensions. Accurate vestibular extensions are necessary for the fabrication of acceptable custom impression trays. The goal when making a final impression is to make a replica of the soft and hard tissues, with maximum coverage of supporting tissues and minimal extension onto the surrounding movable tissues and muscle attachments. To capture this detail, a well-formed custom tray is required. This tray material should be rigid, stable, easily adjusted as necessary, and not bulky with accurate extensions. Accurate vestibular extensions are necessary for the creation of acceptable custom impression trays. Border molding technique can ensure properly extending the flange length of an impression tray prior to making the final impression.
For proper tray fabrication, the clinician has to choose from three final impression techniques-mucostatic, functional, and selective pressure. The selective pressure technique differs from the other two techniques. With the selective pressure technique, the clinician attempts to place light pressure on specific areas of the arches and minimal-to-no pressure on other areas. With the mucostatic technique, an attempt is made to place little to no pressure on the supporting structures. With the functional technique, pressure to the supporting structures is desirable.
Analyzing the final impressions for dentures is critical. Check to make sure the impression is not overextended. The term "overextended" usually applies to an impression tray or impression that is excessively long or deep and may eventually lead to the final denture being overextended and creating denture irritation. "Underextended" refers to an impression tray or impression that is excessively short or shallow, creating inadequate borders that result in a denture with less stability or retention.
Anatomy
Review of the oral cavity anatomy may provide more insight to the structures involved following extractions and the fabrication of dentures, as well as the newly remodeled supporting structures. Understanding the borders of the dentures and the positions they occupy in consideration of anatomy can help the clinician provide a better prosthesis. For example, the location and name of the site where the mucous membrane lining of the cheeks and lips reflects and joins the unattached gingiva or alveolar mucosa is known as the fornix of the vestibule; it would be incorrect to refer to it as the muco-buccal fold. It is always important to use correct terminology when discussing anatomy and how relates final prostheses.
Regarding the maxillary arch, there is one major difference between the upper medial labial frenum, or frenulum, and the buccal frenula. The upper medial labial frenum does not contain muscle fibers, unlike to the buccal frenula (Figure 1). This gives insight to the outcome and evaluation within final impressions, such as understanding that the buccal frenulum space and muscle fiber attachment creates a defined space within the flange of the denture and affects the retention of the denture in function. The medial labial frenum does not have muscle fibers and typically does not influence the denture retention or stability with the denture during function.
Following full-mouth extractions, the alveolar ridges undergo significant bone loss in most patients. Studies indicate that the mandibular ridge resorbs approximately four times as much as the maxillary arch.6 This is important to discuss with a dental patient regarding alternative dental therapies, if dental implants will be a consideration in the future.
Maxillary Landmarks
There are several landmarks that are important in the maxilla. One is the incisal papilla (Figure 2) when contouring occlusion rims and positioning the denture teeth. The facial surfaces of the natural central incisors, when present, are approximately 8 to 10 mm anterior to the middle of the incisal papilla,7 and the tips of the canines are approximately in line with the middle of the incisal papilla. The location of the fovea palatini is also important to note in the edentulous patient. The fovea palatini are two depressions that lie bilateral to the midline of the palate, at the approximate junction between the soft and hard palate and denote the sites of opening of ducts of small mucous glands of the palate (Figure 3). They are often useful in the identification of the vibrating line because they generally occur within 2 mm of it.8
Additionally, the maxillary complete denture should not cover the hamular process. The location of the hamular process, or hamulus, is important because it is a bony projection of the medial plate of the pterygoid bone and is located distal to the maxillary tuberosity. Lying between the maxillary tuberosity and the hamulus is a groove called the hamular notch (Figure 4). This notch is a key clinical landmark in maxillary denture construction because the maximum posterior extent of the denture is the vibrating line, which runs bilaterally through the hamular notches.9
Mandibular Landmarks
Among landmarks in the mandible, the structure located distal to the last mandibular molar is important in the making of a complete mandibular denture. In the lower arch, a triangular area of thick mucosa is found distal to the last molar, basically on the crest of the ridge, and is referred to as the retromolar pad. This pad is important in denture construction from both a denture extension and plane of occlusion standpoint. It should be covered by the denture, and the plane of occlusion is generally located at the level of the middle to upper one-third of this pad (Figure 5).
Just buccal to the crest of the mandibular ridge in the distal-buccal corner of the arch is an area known as the masseter notch, or groove area (Figure 6). This area is important in mandibular denture fabrication because of its influence on impression making. Because of the fatty roll of tissue often overlying the masseter muscle, this cheek area must often be lifted to eliminate the fatty roll, particularly when making the final impression. If the clinician does not properly evaluate this area, the resultant completed mandibular denture could be overextended, causing denture instability and tissue irritation.10
The buccal shelf is important in the fabrication and wearing of mandibular complete dentures because it is the primary stress-bearing area in the mandibular arch. It is an area bounded on the medial side by the crest of the residual ridge, on the lateral side by the external oblique ridge, in the mesial area by the buccal frenulum, and on the distal side by the masseter muscle. It is just anterior to the masseter notch area (Figure 7).
The area that determines the most distal lingual extent of a mandibular complete denture and creates difficulties for the clinician is an area called the retromylohyoid area. This area is the most distal extension of the mandibular denture, and the opposing retromylohyoid areas are usually undercut in relation to each other. The bone structure of the mandible bilaterally in the region of the molars is where the mylohyoid muscles attach. The mylohyoid muscle maintains a critical role in day-to-day activities, including the mastication and swallowing of food and the production of speech. When the mylohyoid muscle contracts during swallowing, it functions to elevate the base of the tongue and the hyoid bone anterosuperior with the mandible fixed. These undercuts may greatly complicate the process of acquiring the preliminary and final impressions.11 The dentures may also require considerable adjustments in these areas at the time of the insertion and post-insertion with patient mastication and swallowing. The action and anatomy occurring in the undercut areas can be quite irritating and painful to the patient.
Processing
There are four methods of polymerizing denture base resin: heat, chemical reaction, microwave energy, and light. Polymerization techniques create denture base resin shrinkage. The approximate shrinkage of a denture base resin during polymerization (processing) is approximately 0.3% to 0.5%.12 Also, denture resin will absorb water from its storage fluid and expand slightly (0.1% to 0.2%). This is important due to absorption of water by the denture and compensates for the shrinkage during polymerization, making the final dimensions almost the same as those of the mouth.
Regarding tooth selection, the advantages of resin denture teeth over porcelain denture teeth are that they have better retention to the denture base, are easier to adjust, do not place as much occlusal impact to the underlying tissues, and are less likely to fracture, as acrylic is less brittle.13,14
Considering denture relines, there are advantages to laboratory relines as opposed to chairside relines. The polymer resulting from a laboratory polymerization is much stronger, bonds more tenaciously, and resists fluid absorption and color change better than the resins polymerized directly in the patient's mouth with chairside products. The frequent replacement of tissue conditioners is primarily due to the soft reline material hardening over extended periods of wear. If allowed to remain too long, the hardened tissue conditioner may cause the same irritations to the residual ridges that were observed prior to conditioning.15
Managing Speech Complications
Managing pronunciation difficulties from full-arch removable prosthetics can be challenging. Because of changes in vertical dimension, the esthetics and arch form from the original natural tooth position to the artificial replacement (denture) are not always resolvable, contributing to speech complications. Nonetheless, improvements should be attempted through troubleshooting by checking each patient's pronunciation of certain sound groups.16-18
"L" sounds position the tongue to lingual of anterior teeth. The word "lolly" or "lullaby" are good the test words. When anterior teeth are to forward or too lingual, the "L" sounds are not clear; then, the anterior teeth should be repositioned until speech is clearer.
"Th" sounds position the tongue between the upper and lower anterior teeth. If the test terms such as "thirty-three" and "ethel thayer" are unclear, then check freeway space. There should be a minimum of 2 to 3 mm between maximum intercuspation and the rest position. If there is not enough freeway space (too much VDO), then adjust the occlusal of the posterior teeth on either arch or both to provide more.19 Of course, check the anterior teeth position as well.
"S" and "Z" sounds can be tested using the word "Mississippi" for teeth-to-teeth position. If the maxillary teeth are in the correct esthetic position, then shorten the mandibular anterior teeth until the "S" sound is correct. If there is a lisp, then the maxillary and mandibular teeth are in heavy contact. Adjust the length of both anterior maxillary and mandibular teeth until the "S" and "Z" sounds are corrected.
"Sh" sounds for tongue to posterior teeth boundary can be tested with terms like "shush- busha." If speech is not correct, then the arch form is too narrow or there is too much VDO. Grind the lingual flanges of the mandibular prosthesis in order to provide more tongue space. It may be necessary to reduce the lingual of the teeth as well. If there is not adequate tongue space, consider a posterior cross-bite to create more tongue space.
"F" and "V" sounds require contact between the upper incisors to the lower lip. If a test term like "fifty-five" is not correct, the maxillary anterior teeth are set too high or too low. Reaching with the lower lip to contact the maxillary anterior incised edges is an obvious sign of a problem. Reset the maxillary incised edges until the "F-V" sound is distinct.
"B," "M," and "P" sounds require lip-to-lip contact, as shown when pronouncing the word "bump." Patients with problems making these sounds are experiencing the problem that irks many female denture wearers of not being able to roll their lips together when applying lipstick. Close the patient's VDO and increase the freeway space. Also, verify that the anterior teeth are not too far forward; bring teeth lingually to allow for normal lip function.
Alternatives for Full-Arch Removable Prosthetics
When attempting single maxillary dentures opposing natural dentition, the primary reason for failure is that the optimum occlusal scheme may be compromised (Figure 8 and Figure 9).20One way to increase stability and retention of single maxillary dentures is to incorporate adjunctive treatment, such as dental implants and attachments with overdentures.21 Overdentures usually cover and rest on natural teeth, implants, and the roots of natural teeth. Another option for full-arch prosthetics is an immediate denture. However, a large problem with immediate dentures is sometimes the denture cannot be assessed for esthetic results prior to the insertion appointment. There are other alternatives, such as implant-supported removeable dentures utilizing locator abutments with attachments, bar-supported dentures with Hader clips (Figure 10), or screw-retained fixed bridges fully supported by dental implants (Figure 11).
Posterior Occlusion
Centric relation is a positional relationship between the maxillary and mandibular arches. Centric occlusion is the occlusion of the denture teeth when the patient is in the centric relation position. The two major posterior occlusal schemes for complete denture patients are balanced and nonbalanced.22 The primary indications for a balanced occlusion are to establish significant vertical overlap of the anterior teeth. If semi-anatomic or anatomic opposing posterior denture teeth are required because of esthetic concerns, the clinician believes they would improve the masticatory efficiency, the patient had existing dentures with anatomic or semi-anatomic denture teeth, or a vertical overlap of the anterior teeth is needed. However, a contraindication for selecting a balanced occlusion is that the patient cannot achieve a repeatable centric relation position.
Anterior disclusion of the posterior teeth is preferred for natural teeth but is contraindicated in complete dentures. The natural anterior teeth anchored in bone can bear strong excursive forces and eliminate or at least greatly reduce these destructive forces on the posterior teeth. Edentulous patients do not have natural teeth anchored in bone; rather, they have denture bases fitted to the residual ridges. Therefore, any forces limited to the anterior teeth are immediately directed almost exclusively to the anterior ridges. Because these forces are not spread over a wide area of the edentulous ridges, soft tissue abuse and bone loss are common.
Lingualized occlusion is recommended for patients whenever possible. Both balanced and nonbalanced lingualized occlusions are easily achieved occlusal schemes. They reduce some of the disadvantages and increase some of the advantages of conventional schemes.23 Centric relation position, too, is the starting reference point for complete denture fabrication, repeatable and can be verified and a functional position for denture occlusion. Complete dentures should be fabricated so that the initial and complete final occlusal positions coincide with the centric relation arc of closure. At the proper occluding vertical dimension, this position becomes the centric occlusion position for the patient.
Consider the direction in which the crests of the residual ridges resorb following extractions-the mandibular residual ridge resorbs downward and outward, while the maxillary residual ridge resorbs upward and inward. Because of these resorptive patterns, it is often necessary to create a crossbite for the posterior teeth (Figure 12).6,24
Tooth Selection and Set-Up
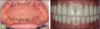
Determining tooth shape and shade selection begins with the introduction of the dentist and patient. Certainly, photographs of the patient's smile, pre-extraction study models, existing dentures, and occlusal rims are all great sources of information to help the patient achieve an esthetic end state. Determining the lip line on a full smile can be transferred into the wax occlusal rim and help to minimize inciso-gingival length of maxillary anterior teeth and avoid a "gummy smile." In this author's experience, the most common errors in denture tooth selection are too light in shade and too small in size. For most patients, the position of the incisal edge of the maxillary anterior teeth determines esthetics, while the cervical portion, or necks, of the teeth and the fullness of the maxillary denture base determine lip support. Most patients desire symmetrical arrangement of the anterior teeth with minimal variations that might provide a more natural look (Figure 13). The alignment of the canines is important from an esthetic standpoint.
Some may think that recently extracted teeth may aid in shade selection. However, this is not accurate due to the dehydration of the teeth following extraction or the effects of disinfection solutions in which the teeth are stored.
The long axis of the maxillary canines may be set vertically or distally inclined with the cervical portion prominently oriented because of its labial position in relation to the lateral incisor. For esthetic purposes, canines should be rotated so that the distal facial surface of the tooth is not visible when viewed for the anterior. The plane of occlusion is related to the retromolar pad, the interocclusal space between the ridges, and the ridge crests themselves. The plane of occlusion ideally splits the distance between the maxillary and mandibular ridges, is parallel to both ridges, and is level with the middle to upper one-third of the retromolar pad. If an adjustment is necessary to the vertical position of the plane of occlusion and interarch space or if esthetics are problematic, the position of the plane of occlusion may be adjusted either superiorly or inferiorly to a small degree. When adjusting the height of the occlusal plane, the mandibular arch should be favored whenever possible because of the decreased stability of the mandibular denture.
Posterior horizontal buccal overlap of the posterior teeth, especially second molars, is a consideration when arranging the opposing teeth. An arrangement that results in the buccal surfaces of both the maxillary and mandibular teeth being aligned end-to-end is contraindicated due to potential cheek-biting situation. A choice to not set second molar teeth is an option if adding them is obviously going to be uncomfortable for the patient.
The esthetic and functional try-in appointment is to assess the esthetic position of the denture teeth, facial support, phonetics, occlusion, vertical dimension, occlusal scheme, and centric occlusion. The procedure allows the patient to see the esthetic results from the previous records appointment and the tooth selection process. If the interocclusal distance is limited and the teeth touch at the resting vertical dimension, remove the posterior teeth of either arches to provide room for the new bite registration material. If the anterior teeth prevent the proper occluding vertical dimension position from being obtained, then the teeth must be removed from the same occlusal rim from where the posterior teeth were removed.
Conclusion
Dentures are not a replacement for teeth; dentures are a replacement for no teeth. A principled and disciplined review of oral cavity anatomy may perhaps help create a result better than the patient's expectations. It is important to understand the process of dental record acquisition, medical history review, radiographic imaging, occlusion, and the end-state occlusal scheme when handling complex phonetics and meeting esthetic expectations. The dentist's job is to take extreme ownership within the process of complete denture fabrication and delivery of the prosthesis. Inform the patient of all viable options before beginning prosthetic procedures. Providing alternative therapies such as removable dentures that are implant- and tissue-supported by locator, Hader clip attachments, or screw-retained implant-supported fixed long-term prosthetics is advised.
About the Author
Thomas Bilski, DDS
Private Practice
Independence, Ohio
References
1. Jacobson TE, Krol AJ. A contemporary review of the factors involved in complete denture retention, stability, and support. Part I: Retention. J Prosthet Dent. 1983;49(1):5-15.
2. Bláhová Z, Neuman M. Physical factors in retention of complete dentures. J Prosthet Dent. 1971;25(3):230-235.
3. Stamoulis S. Physical factors affecting the retention of complete dentures. J Prosth Dent. 1962;12:857-869).
4. Gaikwad AV, Singh KP, Hazari P, et al. Different classification systems of complete denture patients based on mental attitude: a review. Int J Oral Care Res. 2015;3:28-31.
5. Grippo JO, Kristensen GJ. The importance of making and retaining diagnostic casts. Dent Econ. 2015;2:2-4.
6. Samyukta AG. Residual ridge resorption in complete denture wearers. J Pharm Sci & Res. 2016;8(6):565-569.
7. Jain AR. Review on Incisive papilla: A solution to prosthetic dentistry. Drug Invent Today. 2018;10(5):677-683.
8. Bahagyalakshmi P, Manne P, Gopal H, Kunta M. Evaluating the position of fovea palatinae in relation to posterior palatal seal in completely edentulous patients. IOSR Journal of Dental and Medical Sciences. 2018;17(11):1-4.
9. Roumanas E, Lauciello F. Complete Dentures Anatomy of the Denture Foundation Areas. Foundation of Oral-facial Rehabilitation. Accessed February 26, 2021. https://www.ffofr.org/education/lectures/complete-dentures/anatomy-of-denture-foundation-areas
10. McCord JF, Grant AA. Identification of complete denture problems: a summary. Br Dent J. 2000;189(3):128-134.
11. Basit H, Tariq MA, Siccardi MA. Anatomy, Head and Neck, Mastication Muscles. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 10, 2020. Accessed February 26, 2021. https://www.ncbi.nlm.nih.gov/books/NBK541027/
12. Pow EH, Chow TW, Clark RK. Linear dimensional change of heat-cured acrylic resin complete dentures after reline and rebase. J Prosthet Dent. 1998;80(2):238-245.
13. Spratley MH. An investigation of the adhesion of acrylic resin teeth to dentures. J Prosthet Dent. 1987;58(3):389-392.
14. Clancy JM, Boyer DB. Comparative bond strengths of light-cured, heat-cured, and autopolymerizing denture resins to denture teeth. J Prosthet Dent. 1989;61(4):457-462.
15. Jang DE, Lee JY, Jang HS, et al. Color stability, water sorption and cytotoxicity of thermoplastic acrylic resin for non metal clasp denture. J Adv Prosthodont. 2015;7(4):278-287.
16. Howell PG. Incisal relationships during speech. J Prosthet Dent. 1986;56(1):93-9.
17. Spear F. Positioning maxillary central incisal edges: phonetics. Spear Esthetics Blog. Spear Education website. Published October 24, 2013. Accessed February 26, 2021. https://www.speareducation.com/spear-review/2013/10/positioning-maxillary-central-incisal-edges-phonetics
18. Hodges J. Managing phonetic complications arising in full-arch All-On-4 hybrid cases. Dentistry IQ web site. Published July 6, 2016. Accessed February 26, 2021. https://www.dentistryiq.com/dentistry/article/16352782/managing-Phonetic Complications Arising in Full-Arch All-On-4 Hybrid Cases.
19. Johnson A, Wildgoose DG, Wood DJ. The determination of freeway space using two different methods. J Oral Rehabil. 2002;29(10):1010-1013.
20. Bhandan S. Outcome of single maxillary complete dentures opposing mandibular teeth: A need to introspect on the prosthodontic treatment protocol. J Indian Prosthodont Soc. 2016;16(1):15-19.
21. Scherer MD, McGlumphy EA, Seghi RR, Campagni WV. Comparison of retention and stability of implant-retained overdentures based upon implant number and distribution. Int J Oral Maxillofac Implants. 2013;28(6):1619-1628.
22. Abduo J. Occlusal schemes for complete dentures: a systematic review. Int J Prosthodont. 2013;26(1):26-33.
23. Clough HE, Knodle JM, Leeper SH, et al. A comparison of lingualized occlusion and monoplane occlusion in complete dentures. J Prosthet Dent. 1983;50(2):176-179.
24. Atwood DA. Reduction of residual ridges: a major oral disease entity. J Prosthet Dent. 1971;26(3):266-279.