You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
It is an age-old question: When should we incorporate new techniques or maintain our tried-and-true practices? Oftentimes, it is challenging to know, especially in the realm of clinical technology that is constantly evolving in the dental world. Developments are moving rapidly in all areas of the healthcare space. Technology and advancements span such disparate and wide-ranging subjects as CAD/CAM, lasers, implant materials, bonding materials, intraoral cameras, 3D printing, dental turbines, Bluetooth toothbrushes, and more. The parade of innovation in 21st century dentistry never stops. As such, new technology is extremely attractive to the modern dentist. It should be, considering the possibility to improve clinical outcomes, the patient experience, and potentially even the overall financial success of the practice. But when does classic methodology outdo innovation? Is innovation worthwhile for innovation's sake? Where do we draw the line in our own decision making, day-to-day, so that dentists do not sacrifice quality or ease in favor of the latest dental trend or technology?
In the broad landscape of dental techniques, impression making stands out as an area where rapid innovation has made a significant impact on how the modern clinician practices. Digital impressions came onto the radar of dental professionals in the past two decades and almost immediately became a viable option (if not a mainstay for many) in the practice workflow. The quality of an impression is fundamental to the quality of the care that can be provided to patients. For this reason, it is crucial to carefully weigh the pros and cons of analog versus digital impressions. In the clinician's toolbox, there are many reasons to keep a retinue of options including both "old" and "new." This article will review a rigorous methodology for clinical decision making that may help the practitioner decide when analog impressions are preferred over digital ones.
How to Choose for Quality Patient Care
Alongside more technically driven considerations, it is always important to remember the bread and butter of any clinical decision: the patient. What does the patient want and why? There are fundamental conditions that must be met in order to support a rationale for one technique over another. When it comes to patients, these can be categorized according to comfort, efficiency, quality, and overall outcome.
Patient Convenience and Technique Procedural Duration
One initial factor that may be useful to consider is the makeup of the practice's patient population. What is the average age of patients? What is the financial model they expect? How many patients are seen in any given day? How long do patients wait in the waiting room and what factors contribute to this? What are patients used to? What is the point of the innovative technology utilized and how much will it actually improve clinical outcomes? A 2015 randomized crossover trial comparing patient-centered results of digital over conventional impressions for implants (with 20 patients at a mean age of 55.4 years) used a visual analog scale (VAS) questionnaire to determine whether patients preferred intraoral scanning (IOS) versus polyether impressions.1 This study found that mean convenience level was statistically greater for the IOS system versus the analog impressions.1 They found that IOS was also significantly faster, taking 14.8 2.2 minutes versus 17.9 1.1 minutes.1
When deciding on whether to incorporate digital technology, use scientific methods to assess the quality of any given system. How accurate and consistent are the outcomes? Newer is only better if it indicates a statistically significant difference as measured by appropriate statistical analyses of clinical data including t-tests, ANOVA, chi-squared, standard deviation, standard error, relevant post-hoc tests, etc. Consider the size of the tested population as well. The smaller the group, the less representative. Looking back at the aforementioned paper and accounting for the described standard deviations, the data would imply that at its slowest, IOS took 17 minutes, and at its fastest, conventional methods took 16.8 minutes. The study further concluded that "both impression protocols worked successfully for all study participants capturing the 3D implant positions."1 A skilled clinician may look at these numbers and the study conclusion with some apprehension. At most, they could save between six to seven minutes.1 But at worst, they only save one minute in speed.1 Patients may find the digital process generally more convenient, but is it actually faster for a clinician who has done hundreds of analog impressions, considering the difference in clinical outcome may be negligible?
These questions can be difficult to answer. But to start, it is helpful to consider comfort on both sides. If the clinician is a master of the analog impression and has been doing so for at least a decade or more, it may actually be more advantageous (particularly in the short term) to continue offering primarily analog impressions. Consider this: no new investment is required. There is no need to learn the ins and outs of a complicated system, deal with the hassles of hardware and software malfunctions, account for the high start-up costs, or get the office team up to date on how to use, maintain, or ‘sell' the new technology. But digital impressions do offer many benefits over the analog workflow, including but not limited to no longer needing to select trays, ideal material, adhesive, or considerations of dimensional changes.2
Patient vs Physician Preferences for Impression Techniques
A 2013 study of 30 patients' preferences of polyether versus digital impressions for dental implants found that patients rated the experience (preparation, taste, gag reflex, overall preference) of digital impressions better than analog, but that they perceived digital taking longer than analog impressions.3 The researchers concluded that "taste" was one of the most significant contributors to patients preferring the digital scan, though patients perceived the duration of the process as less desirable for digital scans.3 A 2015 within-subject comparison study of patient perception and procedure duration for digital and analog complete-arch impression procedures found that over 80% of 50 participants were in favor of digital over analog impressions.4 They also found that digital impressions took nearly half the time of analog impressions.4 A 2016 randomized controlled trial found a similar comparison of duration for digital versus implant impressions.5 They also found that 64% of the dentists they assessed rated IOS effectiveness higher than analog.5 Taken together, these studies provide both sides of the story: how patients feel and how dentists feel about IOS.
The reality is that there will always be something new in the clinical space. A clever cost-benefit ratio will go a long way in determining whether or not to make the switch. Impressions require clinical expertise and training. Clinicians should not discount their familiarity with analog impressions if they have consistently excellent clinical outcomes, high patient satisfaction (measured anonymously and accurately by patient surveys), and uncontested financial prosperity as a result. But it is also important to note that analog impressions prove challenging to replicate if models are lost or the quality of the initial impression wasn't superb. Ease of replicability may factor into the costs of analog impressions versus digital. Conduct a financial analysis to determine how much faster and cheaper digital impressions can make the process. Additionally, by what ratio can they improve clinical outcomes? If the amount isn't over at least 10% in all cases, then digital impressions may not be the best choice.
Variation in Quality and Relevant Applications in Digital and Analog Systems
Variations between digital systems are also important to factor in. A 2017 in vitro study of four intraoral scanners found significant differences in trueness (how close the mean is to the "true" value), but no significant differences in precision (how well the results agree with one another).6 Another 2017 study, this time assessing the accuracy of multi-unit implant impressions, found that digital impression techniques performed statistically better in accuracy compared to the traditional impressions techniques, which they concluded had greater variability.7 A 2016 study of digital versus polyether analog impression accuracy in completely edentulous patients found no significant differences between their different treatment groups (splinted implant level, digital implant level, splinted abutment level and non-splinted abutment level) and a stone master cast control.8 From their results, they concluded that digital implant impressions from an intraoral optical scanner are as accurate as analog.8
A 2017 literature review noted that pros of the digital system include less discomfort for patients, better time efficiency and simplicity, and improved communication of technicians with patients.9 On the other hand, they found that IOS had purchasing and managing costs, and that there is a learning curve coupled with difficulty in deep margin line detection for prepared teeth or bleeding cases.9 Long-span restorations for IOS may not be supported in the literature, but IOS has many applications for prosthetic restorations, smile design, and guided surgery.9 A 2015 systematic review of accuracy in different implant impression techniques from 32 studies indicated that greatest accuracy was achieved either in a polyether open technique using splinted squared transfer copings or a powder optical intraoral system.10
Consider also how patient anatomy and physiology plays into the issue. Analog impressions are often easier for patients with very small mouths or limited openings. Patient-centered care would dictate that every single patient should receive the highest level of care available. For patients with a limited opening, impressions may be more labor intensive, with methods such as a sectional, locking custom impression tray, a dual-arch impression captured with a modified face-bow fork as a tray, or a modified open tray implant impression technique.11-13 The necessity for even more technical skill and inventiveness in capturing impressions for patients with limited openings makes it an additional challenge to institute digital procedures.
When and How Analog Impressions Can Achieve Greater Accuracy and Efficiency
Alongside the questions of time, patient comfort, and clinician preference described above, it is necessary to review the clinical scenarios where digital impression techniques fall short. Analog impressions are often more accurate for a full arch with multiple preps and more efficient for larger restorative cases, particularly those that utilize an analog articulator. They can be poured in the dentist's office, whereas a printer or milling unit would be required for a digital impression if an analog model is needed. From this point on, there will be discussion and comparison of multiple advanced analog techniques. These include a putty wash VPS hybrid impression technique and full-arch impression technique (to use instead of triple tray).
Putty Wash Hybrid Impression Technique
A putty wash hybrid technique is useful for diagnostic impressions where accuracy is of great importance. Dimensional stability is one characteristic that can have a significant impact on restoration accuracy.14-18 A 2014 study found that a two-step putty-wash impression technique resulted in greater accuracy and reduced size of discrepancies versus a one-step technique.17 Disinfection after getting the impression may be a concern, but there are many routines and materials that will not lead to unacceptable dimensional stability.18 The following technique reduces the amount of material that extrudes down the throat and gives accurate details due to the lower viscosity of the material plus pressure from the putty that has already begun to set.
The first step is to size the disposable impression stray so that the last molar is fully covered, but extra space is given appropriately on the buccal and lingual. Then mix a vinylpolysiloxane (VPS) impression material with a working time of 1 to 2.5 minutes until color uniformity is reached. To do this, start with equal scoops of catalyst and base. Load the tray next, removing excess as needed, forming the putty so as to cover the tray's flange, and creating a channel for the teeth to fit into. To seat the tray in the mouth, seat fully posterior first and roll into the anterior. It's crucial to roll the patients lip over the tray and material's flange. Give a vigorous shake to form space where light body material will be injected later. Do not enable the material to set. This means the tray should be removed as soon as possible while it is still considered "soft."
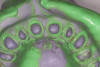
At this point, carefully inject a light body material over the top of the partially unset putty, covering in a single layer across the entire indented surface. Reseat the tray, starting with the posterior and rolling carefully to the anterior. Ensure the patient's lip is rolled over both the material and the tray. Remove the tray once the entire intraoral set time has elapsed. To remove, instruct the patient to close their mouth part way. Release the tray first at the posterior flange on either side (Figure 1).
Triple-Tray vs Full-Arch Analog Impression Technique
The triple-tray impression (Figure 2) may give a strong preparation, clear margins, information about adjunct teeth, and bite at the required vertical dimension, but it is simply not strong enough at capturing the function of teeth in excursive movement. A full-arch technique will make finalizing excursive contacts much easier (Figure 3 and Figure 4). Full-arch impressions may cause a sacrifice on productive chair time, as impressions and records can take between 15 and 20 minutes. But this technique should make up for the front-end chair time with reduced time later on when seating or adjusting both simple and complicated cases.
The clinician must consider their own expertise when determining whether this is the ideal technique to use analog versus digital. A 2017 comparative study found that full-arch digital impressions using intraoral scanners provided significantly greater accuracy over analog impressions using an open-tray splinted method.19 The researchers do note, though, that different digital systems can provide variations in the amount of 3D deviations.19 A 2015 study assessing the surface structure representation completeness of optical 3D scans found that full-arch impression scans were lacking in some critical regions necessary for orthodontic model analysis.20 Thus, just as clinicians can vary in their level of expertise, so too can the technology they hope to leverage.
Both digital and analog techniques lose their accuracy when the complexity of the dental case increases. For example, a 2020 prospective study of 16 edentulous maxillae found that, in comparison of digitized final stone casts from analog impressions with virtual intraoral full-arch digital casts, the increasing implant number was positively correlated with number of 3D deviations.21 They did not find a statistically significant difference between the two techniques though.21 Another 2020 study assessed the precision and trueness of full-arch digital impressions and found that intraoral scanning conditions had a significant effect on both trueness and precision.22 They noted that this was the case for angular and linear metrics, which were both affected by how much the distance between scan bodies had increased.
The best path for an analog full-arch impression is to use facebow transfer. A dentist cannot rely on only hand articulating or placing bite registration on prepared teeth. A full-arch impression mounted using a facebow transfer, which will provide the laboratory with a means to determine teeth interactions in necessary positions. Accuracy gets even better when the clinician is willing to set condylar elements via a semi-adjustable articulator. Options for doing this include either an end-to-end retracted image or a protrusive bite record. To ensure the best possibility of esthetic and functional issue management, full-arch impressions will often provide greater functional and esthetic information at the front-end.
Final Impression Tissue Management
Tissue management is a significant factor in the quality of crown and bridge impressions. Patients with prior long-term restorations (especially those with inadequate margins) may have poor hygiene and noticeable inflammation that makes preparation a challenge. A chlorhexidine varnish can make a big difference to improving the health of the tissue prior to impressions.
If it's clinically reasonable, it may also be a good idea to leave margins supragingival. If not, leave margins equigingival where they meet the crest of the tissue. Avoid bleeding at all costs because it adds another headache to the tissue management process. This can come up when placing subgingival margins. A quick fix is to place the initial margin equigingival, then move on to placement of a primary cord to get the tissue in the proper position. Then, the clinician can move the margin subgingival without excessive tissue trauma.
Retraction is the next step for quality final impressions. To create an ideal emergence profile for a successful restoration, retraction should be used for generation of room where the impression material can seep apically over the margin. One technique that can be used is placement of second cord that has a larger diameter than the initial used for the preparation. Any bleeding tissue can be taken care of with a hemostatic agent. Take the final impression with the clinician's preferred material.
Start by loading heavy body material. Get the top cord wet in order to reduce the possibility of bleeding once the tray is removed. Dry the area well so that the impression material can get excellent contact with surfaces of the tissue and teeth. Finally, it is time to seat the impression tray after injecting with low viscosity material. Keep the tray held carefully throughout the entire intraoral set time duration. The less movement of the patient, the greater the impression accuracy. Take advantage of magnification after the impression has been removed from the mouth and determine if there is adequate flash, voids, pulls, or other evidence of a poor impression. All steps should be undertaken with careful conscientiousness to avoid the need for a retake.
Digital impressions (Figure 5) may have issues replicating the tissue and require unique approaches, such as in the case of replicating peri-implant soft tissue contours or the appropriate emergence profile.23 The complexity of the case in question will determine whether or not a digital technique is merited and what digital technique to use. For some cases, like those will multiple implants, dentists may have issues depending on whether a transfer technique, pick-up technique, or splinted pick-up technique is used.24 A 2017 systematic review of 10 articles on the accuracy of digital impression technique was inconclusive, as they found that five of the articles indicated intraoral scanners would be successful in implant in dentistry, but two of the studies showed lack of reliability.25
Conclusion
The modern dentist can be likened to a highly educated individual in a "candy shop" of technology and advanced materials. This leads to a difficult situation where there are too many options and too many ways in which to make decisions. A dentist may have to consider numerous factors spanning investment costs, office incorporation challenges, patient pushback, team pushback, hardware malfunctions, software malfunctions, inconsistent outcomes, lack of familiarity, high learning curve, and many more. Where the average consumer may find the product landscape overwhelming, a healthcare professional has an even greater difficulty facing them because they must choose for themselves and for others. On top of that, there is far more at stake.
One question that looms large in the clinical decision-making process is when or whether to use digital over analog impressions. Analog impressions provide many benefits such as familiarity, little or no technological investment, ease with limited opening, greater accuracy for full arch with multiple preparations, more efficiency for larger restorative cases, and ability to pour in-office for an analog model. The downsides to analog impressions are longer procedure times (can be up to double the time of digital impressions), the need to retake impressions if they are poor or models are lost, and greater patient discomfort. Dentists will benefit from conducting thorough research into the specific digital system they are considering, including its proven accuracy, reliability, procedure time, patient comfort, and overall clinical outcome. Analog impressions shine when the clinician is highly skilled and leverages their knowledge of the situations where they are preferentially indicated.
About the Author
Lee Ann Brady, DMD
Private practice, Glendale, Arizona
References
1. Joda T, Brägger U. Patient-centered outcomes comparing digital and conventional implant impression procedures: a randomized crossover trial. Clinical oral implants research. 2016;27(12):e185-e189.
2. Al Mortadi N, Jones Q, Eggbeer D, Lewis J, Williams RJ. Fabrication of a resin appliance with alloy components using digital technology without an analog impression. American Journal of Orthodontics and Dentofacial Orthopedics. 2015;148(5):862-867.
3. Wismeijer D, Mans R, Genuchten M van, Reijers HA. Patients' preferences when comparing analogue implant impressions using a polyether impression material versus digital impressions (Intraoral Scan) of dental implants. Clinical Oral Implants Research. 2014;25(10):1113-1118.
4. Schepke U, Meijer HJA, Kerdijk W, Cune MS. Digital versus analog complete-arch impressions for single-unit premolar implant crowns: Operating time and patient preference. The Journal of Prosthetic Dentistry. 2015;114(3):403-6.e1.
5. Joda T, Lenherr P, Dedem P, Kovaltschuk I, Bragger U, Zitzmann NU. Time efficiency, difficulty, and operator's preference comparing digital and conventional implant impressions: a randomized controlled trial. Clinical Oral Implants Research.2017;28(10):1318-1323.
6. Imburgia M, Logozzo S, Hauschild U, Veronesi G, Mangano C, Mangano FG. Accuracy of four intraoral scanners in oral implantology: a comparative in vitro study. BMC Oral Health; London. 2017;17.
7. Menini M, Setti P, Pera F, Pera P, Pesce P. Accuracy of multi-unit implant impression: traditional techniques versus a digital procedure. Clinical Oral Investigations. 2018;22(3):1253-1262.
8. Papaspyridakos P, Gallucci GO, Chen C-J, Hanssen S, Naert I, Vandenberghe B. Digital versus conventional implant impressions for edentulous patients: accuracy outcomes. Clinical Oral Implants Research. 2016;27(4):465-472.
9. Mangano F, Gandolfi A, Luongo G, Logozzo S. Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health. 2017;17.
10. Moreira AHJ, Rodrigues NF, Pinho ACM, Fonseca JC, Vilaça JL. Accuracy comparison of implant impression techniques: a systematic review. Clinical Implant Dentistry and Related Research. 2015;17(S2):e751-e764.
11. Baker PS, Brandt RL, Boyajian G. Impression procedure for patients with severely limited mouth opening. The Journal of Prosthetic Dentistry. 2000;84(2):241-244.
12. Bhansali S, Bhansali SP, Negi P. A modified open tray implant impression technique for limited mouth opening. The Journal of Prosthetic Dentistry. 2017;118(1):116-117.
- 13. Maeda Y, Tsugawa T, Furusawa M, Matsuda S. A method for fabricating an occlusal splint for a patient with limited mouth opening. The Journal of Prosthetic Dentistry. 2005;94(4):398-400.
14. Basapogu S, Pilla A, Pathipaka S. Dimensional accuracy of hydrophilic and hydrophobic vps impression materials using different impression techniques - an invitro study. Journal of Clinical and Diagnostic Research. 2016;10(2):ZC56-ZC59.
15. Rodriguez JM, Bartlett DW. The dimensional stability of impression materials and its effect on in vitro tooth wear studies. Dental Materials. 2011;27(3):253-258.
16. Steinhäuser-Andresen S, Detterbeck A, Funk C, et al. Pilot study on accuracy and dimensional stability of impression materials using industrial CT technology. J Orofac Orthop. 2011;72(2):111-124.
17. Levartovsky S, Zalis M, Pilo R, Harel N, Ganor Y, Brosh T. The effect of one-step vs. two-step impression techniques on long-term accuracy and dimensional stability when the finish line is within the gingival sulcular area. Journal of Prosthodontics. 2014;23(2):124-133.
18. Martin N, Martin MV, Jedynakiewicz NM. The dimensional stability of dental impression materials following immersion in disinfecting solutions. Dental Materials. 2007;23(6):760-768.
19. Amin S, Weber HP, Finkelman M, El Rafie K, Kudara Y, Papaspyridakos P. Digital vs. conventional full-arch implant impressions: a comparative study. Clinical Oral Implants Research. 2017;28(11):1360-1367.
20. Vogel AB, Kilic F, Schmidt F, Rübel S, Lapatki BG. Optical 3D scans for orthodontic diagnostics performed on full-arch impressions. Completeness of surface structure representation. Journal of Orofacial Orthopedics = Fortschritte der Kieferorthopadie : Organ/Official Journal Deutsche Gesellschaft fur Kieferorthopadie. 2015;76(6):493-507.
21. Chochlidakis K, Link to external site this link will open in a new window, Papaspyridakos P, et al. Digital Versus Conventional Full-Arch Implant Impressions: A Prospective Study on 16 Edentulous Maxillae. Journal of Prosthodontics. 2020;29(4):281-286.
22. Rutkunas V, Gedrimiene A, Simonaitis T, et al. Effect of intraoral conditions on precision and trueness of full-arch digital implant impressions. Clinical Oral Implants Research. 2020;31(S20):44-45.
23. Monaco C, Evangelisti E, Scotti R, Mignani G, Zucchelli G. A fully digital approach to replicate peri-implant soft tissue contours and emergence profile in the esthetic zone. Clinical Oral Implants Research. 2016;27(12):1511-1514.
24. Stimmelmayr M, Erdelt K, Güth J-F, Happe A, Beuer F. Evaluation of impression accuracy for a four-implant mandibular model--a digital approach. Clinical Oral Investigations. 2012;16(4):1137-1142.
25. Alikhasi M, Alsharbaty MHM, Moharrami M. Digital implant impression technique accuracy: a systematic review. Implant Dentistry. 2017;26(6):929-935.