You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Obstructive Sleep Apnea: A Hidden Health Crisis
Ashley Spooner, DDS
Obstructive sleep apnea (OSA) has been increasingly recognized as a significant health problem over the last two and a half decades.2 OSA is characterized by the frequent collapse of the upper airway passage, resulting in temporary cessations of breathing or disruptions in breathing rhythm (apneas). These events lead to intermittent hypoxemia, increased sympathetic tone, cytokine production, metabolic abnormalities, and abnormal sleep structure. This abnormal physiology results in increased health risks, related to the cardiovascular system, cerebrovascular system, and neurocognitive abnormalities.3 OSA is linked to several other co-morbidities such as hypertension, type II diabetes, stroke, congestive heart failure, coronary artery disease, cardiac arrhythmias, and even early mortality.4-13Not only are the undiagnosed and untreated consequences of OSA medically serious, they can be extremely financially burdensome. In 2016, a report commissioned by the American Academy of Sleep Medicine found the annual economic burden of undiagnosed sleep apnea among American adults to be nearly $150 billion, including workplace accidents and motor vehicle accidents.14
OSA affects 5% to 20% of the general population.15 However, OSA may be grossly underdiagnosed, whether because physicians do not have the time to be looking for such symptoms or because patients are not complaining about any symptoms. Dentists are in the unique position to help reduce the undiagnosed aspects of sleep apnea. Reducing the amount of undiagnosed and untreated OSA will improve the quality of life for our patients, reduce their overall health care costs, and even reduce unnecessary premature death.
The first step for dentists to take towards reducing the risks of obstructive sleep apnea is to bring awareness to what it is through conversations with patients. Dentists are a part of the team of healthcare professionals that can screen and manage patients with OSA, but it is important for a physician to also be involved in order to diagnose OSA. In order to be a successful teammate, dentists should learn not only about OSA but also the healthcare language used to contribute and collaborate with other healthcare professionals. Dentists may have more time and more access to a patient's mouth to see signs and symptoms of OSA. Dentists are thus a crucial component in its screening.
Understanding Sleep
Since OSA disrupts sleep, a comprehensive understanding of what sleep is and why humans need it is critical. According to Merriam Webster, sleep is defined as "the natural, easily reversible periodic state of many living things that is marked by…the loss of consciousness of one's surroundings…and is usually considered essential to the restoration and recovery of vital bodily and mental functions." This tells us, for example, that the difference between sleep and a coma is that sleep is reversible. If there is a loud enough noise, if someone shakes us, or if something else disruptive happens, we will wake up, unlike if we are in a coma. This definition also shows that sleep is about more than just conserving energy; it is a restorative process. As a restorative process, sleep influences the homeostatic regulation of the autonomic, neuroendocrine, and immune systems.16,17,18 On the other hand, decrements in natural and cellular immune function coincide with disturbances of sleep architecture and loss of sleep, as well as suppression of natural killer cell activity and cellular immunity.19-22 Thus, disordered or loss of sleep leads to alterations in immune functions that might adversely affect host resistance to infectious disease, increase cancer risk, and alter inflammatory disease progression.23-25
Since there are a variety of sleep disorders, dentists should have a holistic understanding of sleep disorders-both symptoms and treatment options-in order to best collaborate with the medical community. For example, if a patient experiencing nocturia, defined as the need to get up at night on a regular basis to urinate, this could be a sign of a lack of antidiuretic hormone being released during sleep due to OSA.26 Nocturia affects 50 million people in the United States, with 10 million actually diagnosed with nocturia, but only 1.5 million receive specific therapy for it.27 By understanding the possible symptoms of OSA, dentists can more readily screen for OSA in conversations with patients.
Anatomy of Obstructive Sleep Apnea
Apnea means without breath; sleep apnea is without breath during sleep. Obstructive sleep apnea is an anatomic disorder. Obstructive sleep apnea leads to a lack of oxygen saturation and a buildup of carbon dioxide.
Patients with sleep apnea are often either obese or have abnormal upper airway anatomy (retrognathia, tonsillar hypertrophy, macroglossia, enlargement of the lateral peritonsillar folds, and/or enlargement/elongation of the soft palate).28 Other factors that increase vulnerability for the sleep apnea include age, sex (male), family history, menopause, craniofacial abnormalities, and certain health behaviors such as cigarette smoking and alcohol use.29
Obstructive sleep apnea occurs as repetitive episodes of complete or partial upper airway blockages occur during sleep. During an apneic episode, the diaphragm and chest muscles work harder as the pressure increases to open the airway. Breathing usually resumes with a loud gasp or body jerk. These episodes can interfere with sound sleep, reduce the flow of oxygen to vital organs, and cause heart rhythm irregularities. Figure 1 shows what is happeningphysiologically during an apneic episode.
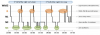
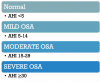
An apneic episode is defined as the complete cessation of airflow for at least 10 seconds.30 Apneas are further classified as obstructive, central, or mixed based on whether effort to breathe is present during the event. A hypopnea is defined as a reduction in airflow that is followed by an arousal from sleep or a decrease in oxyhemoglobin saturation. Commonly used definitions of a hypopnea require a 25% or 50% reduction in oronasal airflow associated either with a reduction in oxyhemoglobin saturation or an arousal from sleep.31Sleep apnea severity is typically assessed with the Apnea-Hypopnea Index (AHI), which is the number of apneas and hypopneas per hour of sleep (Figure 2). The Respiratory Disturbances Index (RDI) measures the number of apneas, hypopneas, and RERAs per 1 hour of sleep (a RERA is a respiratory event that does not meet hypopnea or apnea criteria but does cause an arousal) and the Oxygen Desaturation Index (ODI) is the number of times per hour of sleep that the blood's oxygen level drop by a certain degree from baseline (generally of ≥4% over the last 120 seconds).32
Despite the numerous advancements in our understanding of the pathogenesis and clinical consequences of the disorder, a majority of those affected remain undiagnosed. In addition to primary care physicians, specialists across various medical disciplines, including dentistry, should be sufficiently knowledgeable to identify those affected with this disease.
Screening for Obstructive Sleep Apnea
An effective screening process should begin by taking a comprehensive medical history of each patient. Everyone in the office should be trained on this screening process. It could include an in-depth questionnaire (Figure 3 and Figure 4). By starting a conversation with the patient about their medical history early, the dental team helps create a relationship as a critical part of their medical care team. Simple queries of the patient or bed-partner for the symptoms and signs of the disorder-namely loud snoring, observed apneas, and daytime sleepiness-could help identify those in need of further diagnostic evaluation.33 It is useful to get input from a bed-partner because a patient experiencing OSA might not remember waking in the night, whereas their partner may easily remember their snoring.
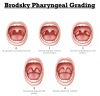
There are many parts of the mouth to consider when looking for possible signs of OSA. One of the most important parts for a dentist to examine is the tongue's position using the Mallampati Classification (Figure 5).34 The pharyngeal anatomy can be observed and graded on a scale of 0 to 4 (Figure 6). Other factors a dentist should look for while examining a patient for OSA are if the patient has a scalloped tongue, an excessive overbite, a high palate, extracted premolars or crowding, abfractions, acid erosion, a mandibular torus, and/or bruxism. Observing one or more of these conditions is not necessarily a sign of OSA, but it may warrant further screening.
OSA Treatment Modalities
Since the approach was introduced in 1981, positive airway pressure (PAP) remains the primary treatment modality for OSA, despite the advent of an array of treatment options.35 This form of treatment applies a constant pressure throughout the respiratory cycle to splint the airway open. Subsequently, bilevel PAP (BiPAP), a modality which delivers a higher inspiratory PAP (IPAP) relative to the expiratory PAP (EPAP), is also found to be effective in the treatment of OSA. A theoretical advantage of BiPAP is that a lower EPAP can be applied that would increase tolerance to PAP treatment of OSA.36 While a CPAP delivers continuous air pressure, adaptive servo-ventilation adjusts pressure to the patient's breathing as it changes during sleep. However, studies have shown some of these methods may not be safe for individuals with heart conditions.37 The effectiveness of CPAP therapy is closely related to the rate of adherence.38,39 CPAP non-adherence (defined as the use of the device for less than 4 hours per night) is a challenge in the management of OSA patients, with rates of CPAP non-adherence ranging from 29 to 83%.40
Another treatment modality option is oral appliance therapy, using a mandibular repositioning device to stabilize the mandible in a protrusive position in order to reduce the collapsibility of the upper airway. When selecting a treatment modality, one should consider both effectiveness and compliance; an extremely effective treatment still will not work if the patient does not utilize it at home.
There are surgical options for the treatment of OSA as well. Uvulopalatopharyngoplasty is a surgery that removes soft tissue at the back of the throat including all or part of the uvula, parts of the soft palate and tissue at the side of the throat, and the tonsil and adenoids in order to open the upper airways. Another option is a mandibular advancement, which is invasive but extremely effective, achieving a success rate of 89%.41 A third surgical option is a hypoglossal nerve stimulator is an implanted medical device that reduces the occurrence of OSA by electrically stimulating the hypoglossal nerve, which causes tongue movement. This stimulation is timed with breathing to relieve upper airway obstruction. Patients must have a certain BMI and AHI range in order to qualify for this surgery.
Orthodontics are most often used for children with mild OSA by expanding the upper arch while continuing to monitor as permanent teeth emerge.
Finally, lifestyle changes are an important component for mitigating OSA. Weight loss, positional therapy, and wearing a nose cone to keep the nose open, are all examples of lifestyle changes that can increase a patient's quality of life by helping them get more oxygen throughout the night.
Dentists should be involved in the collaborative evaluation and treatment of patients with OSA. However, the American Academy of Sleep Medicine and the American Academy of Dental Sleep Medicine have determined that patients with symptoms of OSA must have a face-to-face evaluation by a sleep medicine physician to diagnose OSA and that dentists-even those certified by the American Board of Dental Sleep Medicine-are not qualified to diagnose OSA.42-45 Thus, when conversing with patients about symptoms, dentists should use the term "sleep-related breathing disorder." Through these conversations and comprehensive oral exams, dentists can help to reduce the amount of undiagnosed and untreated sleep disorders, including obstructive sleep apnea. It is important for a collaborative relationship to be established between a qualified dentist and the referring sleep physician so that patients receive the most effective care for their OSA.
References
1. Dempsey JA, Veasey SC, Morgan BJ, O'Donnell CP. Pathophysiology of sleep apnea. Physiol Rev. 2010; 90:47-112.
2.Young T, Palta M, Dempsey J. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993; 328:1230-1235.
3.Knauert M, Naik S, Gillespie MB, Kryger M. Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J Otorhinolaryngol Head Neck Surg. 2015;1(1):17-27.
4.Peppard PE. Young T, Palta M. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378-1384.
5.Nieto FJ, Young TB, Lind BK. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA. 2000;283:1829-1836.
6.Phillips CL, O'Driscoll DM. Hypertension and obstructive sleep apnea. Nat Sci Sleep. 2013;5:43-52.
7.Reichmuth KJ, Austin D. Skatrud JB. Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med. 2005;172:1590-1595.
8.Punjabi NM, Beamer BA. Alterations in glucose disposal in sleep-disordered breathing. Am J Respir Crit Care Med. 2009;179:235-240.
9.Campos-Rodriguez F, Martinez-Garcia MA, Reyes-Nunez N. Role of sleep apnea and continuous positive airway pressure therapy in the incidence of stroke or coronary heart disease in women. Am J Respir Crit Care Med. 2014;189:1544-1550.
10.Arzt M, Young T, Finn L. Association of sleep-disordered breathing and the occurrence of stroke. Am J Respir Crit Care Med. 2005;172:1447-1451.
11.Redline S, Yenokyan G, Gottlieb DJ. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182:269-277.
12.Yaggi HK, Concato J, Kernan WN. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034-2041.
13.Shahar E, Whitney CW, Redline S. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19-25.
14.AASM. Hidden Health Crisis Costing American Billions. Frost & Sullivan. 2016.
15.Wali SO, Abalkhail B, Krayem A. Prevalence and risk factors of obstructive sleep apnea syndrome in a Saudi Arabian population. Ann Thorac Med. 2017;12:88-94.
16.Horne J. Why we sleep: the function of sleep in humans and other mammals. Oxford: Oxford University Press, 1988.
17.Krueger J M, Toth LA. Cytokines as regulators of sleep. Ann NY Acad Sci. 1994;739:299-310.
18.Dinges DF, Douglas SD, Hamarman S, et al. Sleep deprivation and human immune function. Adv Neuroimmunol. 1995;5:97-110.
19.Irwin M, Smith TL, Gillin JC. Electroencephalographic sleep and natural killer activity in depressed patients and control subjects. Psychosom Med. 1992;54:107-126.
20.Irwin M. Immune correlates of depression. Adv Exp Med Biol. 1999;461:1-24
21.Darko DF, Miller JC, Gallen C, et al. Sleep electroencephalogram δ-frequency amplitude, night plasma levels of tumor necrosis factor α, and human immunodeficiency virus infection. Proc Natl Acad Sci USA. 1995;92:12080-12084.
22.Irwin M, Mascovich A, Gillin JC, et al. Partial sleep deprivation reduces natural killer cell activity in humans. Psychosom Med. 1994;56:493-498.
23.Everson CA. Sustained sleep deprivation impairs host defense. Am J Physiol. 1993;34:R1148-R1154.
24.Savard J, Miller SM, Mills M, et al. Association between subjective sleep quality and depression on immunocompetence in low-income women at risk for cervical cancer. Psychosom Med. 1999;61:496-507.
25.Crofford LJ, Kalogeras KT, Mastorakos G, et al. Circadian relationships between interleukin (IL)-6 and hypothalamic-pituitary-adrenal axis hormones: failure of IL-6 to cause sustained hypercortisolism in patients with early untreated rheumatoid arthritis. J Clin Endocrinol Metab. 1997;82:1279-1283.
26.Drangsholt S, Ruiz MJA, Peyronnet B, et al. Diagnosis and management of nocturia in current clinical practice: who are nocturia patients, and how do we treat them? World J Urol. 2019;37(7):1389-1394.
27.Leslie SW, Sajjad H, Singh S. Nocturia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 23, 2020.
28.Schwab RJ, Gupta KB, Gefter WB, et al. Upper airway soft tissue anatomy in normals and patients with sleep disordered breathing: significance of the lateral pharyngeal walls. Am J Respir Crit Care Med 1995;152:1673-1689.
29.Punjabi N. The Epidemiology of Adult Obstructive Sleep Apnea. Proceeding of the American Thoracic Society. 2007;5(2).
30.Memon J, Manganaro SN. Obstructive Sleep-disordered Breathing. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 14, 2020.
31.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force - Sleep. 1999;22:667-689.
32.Temirbekov D, Güneş S, Yazıcı ZM, Sayın İ. the ignored parameter in the diagnosis of obstructive sleep apnea syndrome: the oxygen desaturation index. Turk Arch Otorhinolaryngol. 2018;56(1):1-6.
33.Simmons MS, Pullinger A. Education in sleep disorders in US dental schools' DDS programs. Sleep and Breathing. 2012;16(2): 383-392.
34.Friedman M, Hamilton C, Samuelson CG, et al. Diagnostic value of the Friedman tongue position and Mallampati classification for obstructive sleep apnea: a meta-analysis. Otolaryngology Head Neck Surgery. 2013;148(4): 540-547.
35.Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;317(8225):862-865.
36.Patil SP, Ayappa IA, Caples SM, et al. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. Journal of Clinical Sleep Medicine. 2019;15(2): 301-334.
37.Woehrle H, Cowie MR, Eulenburg C, et al. Adaptive servo ventilation for central sleep apnoea in heart failure: SERVE-HF on-treatment analysis. European Respiratory Journal. 2017;50(2).
38.Barbé F, Durán-Cantolla J, Sánchez-de-la-Torre M, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307(20):2161-2168.
39.Bratton DJ, Stradling JR, Barbé F, Kohler M. Effect of CPAP on blood pressure in patients with minimally symptomatic obstructive sleep apnoea: a meta-analysis using individual patient data from four randomised controlled trials. Thorax. 2014;69(12):1128-1135.
40.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-178.
41.Taub D; Courtney M; Doghramji K. Treatment of obstructive sleep apnea with maxillo-mandibular advancement surgery: evaluation and predictors of success. Thomas Jefferson University Department of Oral and Maxillofacial Surgery Posters. 2018 . https://jdc.jefferson.edu/omsposters/1.
42.American Academy of Dental Sleep Medicine Policy Statement on the Diagnosis and Treatment of OSA. American Academy of Dental Sleep Medicine. 2012. https://aadsm.org/docs/jointpolicy.pdf.
43.Ramar K, Dort LC, Katz SG, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015;117:773-827.
44.American Academy of Dental Sleep Medicine. AADSM treatment protocol: oral appliance therapy for sleep disordered breathing: an update for 2013. Published 2013. https://aadsm.org/docs/Treatment_Protocol_FINAL.pdf.
45.Academy of Dental Sleep Medicine: position statement on dental sleep medicine and portable monitoring. Sleep Breath. 2005;9:189-192. https://doi.org/10.1007/s11325-005-0035-9.