You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Perhaps attributable to popular reality shows and other television programs, there is currently an increased interest in facial injectables used for cosmetic benefits throughout the world. As the number of patient requests to emulate pop culture celebrities increases, the number of medical and dental professionals seeking to help in this trend is also rising. Many states have policies in place that allow dentists to perform facial injections, and that number continues to grow.
There is still much confusion throughout the dental industry in regard to facial injectables. Before implementing facial injections into practice, dental professionals must have a basic understanding of the common injectables, what they are used for, how they work, and how to introduce and discuss them with patients competently and comfortably for use in both therapeutic and cosmetic treatments.
Types of Wrinkles
There are two types of facial wrinkles. Dynamic wrinkles are formed by repetitive movements of the facial muscles and appear when expressing emotions such as fear, worry, joy, sadness, or surprise. Examples of common dynamic wrinkles include frown lines between the eyebrows, forehead wrinkles, "crow's feet," and smile lines. Dynamic wrinkles are created by underlying muscles that contract and create wrinkles.
Although dynamic wrinkles are no longer visible after the face relaxes, dynamic wrinkles generally will turn into static wrinkles over time. Static wrinkles remain on the face even after facial muscles relax; they tend to deepen with age as collagen production declines and causes the skin to lose elasticity. Common static wrinkles include nasolabial folds (marionette lines) around the mouth, across the cheeks, and along the neck.
Common Facial Injectables in Dentistry
Botulinum toxin and dermal fillers are the two most popular types of nonsurgical injectables used for cosmetic procedures performed by dentists in the United States. Both are safe, act quickly, cause few side effects, and are easy to administer.1
Commonly referred to as Botox® (Allergan), botulinum toxin is a neurotoxin produced from the bacterium Clostridium botulinum. Botulinum toxin works on dynamic wrinkles by creating a temporary paralysis of the underlying muscle that causes the wrinkle to form. It prevents the release of the neurotransmitter acetylcholine from axon endings at the neuromuscular junction and thus causes flaccid paralysis.2
Dermal fillers (also known as injectable implants, soft-tissue fillers, or wrinkle fillers) work on static wrinkles by replacing lost volume and stimulating collagen production to promote a healthier-looking, smoother complexion. Dermal fillers can be used to enhance thin lips or increase volume in the cheeks to intensify the natural contours of the face.
Botulinum Toxin in Dentistry
For over a decade, regulatory boards have authorized the use of botulinum toxin by dentists for therapeutic benefits.3 When patients present with migraine headaches resulting from temporomandibular joint disorders (TMJDs), dentists have a comfortable gateway to initiate discussion of botulinum toxin for symptomatic relief. Furthermore, discussing botulinum toxin therapy from a therapeutic standpoint is often a segue into conversation about using facial injectables for cosmetic treatments. Because many patients are familiar with botulinum toxin under the Botox name for cosmetic use, they may proceed to request facial injections for cosmetic benefits in addition to therapeutic treatments.
During their medical history review and examination, patients may exhibit common signs and symptoms of TMJD, such as flattened occlusal surfaces due to clenching and grinding.4 Masseter muscles may be prominent and bulging, the jaw may click on opening and closing, and extraoral examination palpitation may result in pain of the masseter muscles. Dental professionals can initiate discussion by asking about steps the patient has taken to relieve these issues.
Often, TMJD patients have used a nightguard or some sort of occlusal support in the past but discontinued use because they found it to be uncomfortable. When all other conservative treatment options, such as massage therapy and adjustments, also have been unsuccessful, patients may feel hopeless. Offering an alternative solution provides hope and optimism-many patients are unaware that their dentist is authorized to provide botulinum toxin therapy.
For these patients, dentists can initiate discussion about the effectiveness of botulinum toxin in relieving their concerns. In simple terms, it can be explained that due to overactive masseter and temporalis muscles, clenching continues unconsciously. By reducing muscle activity to a normal range with facial injections, the muscle will no longer generate enough force to clench and grind as heavily; patients will experience relief from TMJD discomfort and may even get more peaceful sleep. Moreover, much like a flu shot, muscles targeted with botulinum toxin are very dense, so there is little to no pain on injection.
Indications
Therapeutic indications for botulinum toxin facial injections include TMJD, bruxism, tension and migraine headaches, and repetitive facial expressions such as squinting or making an "angry" face with down-turned eyebrows, which increase tension in the forehead and the back of the neck.5 Cosmetic indications include glabellar frown lines, horizontal forehead lines, crow's feet, radial lip lines, and excessive gingival display.6
Mechanism of Action
Botox is the common trade name for a purified protein called botulinum toxin serotype a, which is derived from the botulinum toxin. When injected in minuscule amounts, it works by preventing the release of acetylcholine from motor nerve endings, causing a temporary paralysis of the muscles.2
Effects
Although it takes approximately 2 to 7 days for the mechanism of action to take effect, botulinum toxin injections can also act as a trigger-point therapy, with some patients reporting immediate relief after injection into overactive facial muscles.7 Much like after exercising, massaging the muscles stretches the lactic acid and provides instant relaxation.
Due to temporary paralysis, after muscles are no longer creating dynamic wrinkles, the skin will regenerate by filling in lines through natural collagen production, and within 2 weeks the skin appears to be smoother.6 In the author's experience, patients who use anti-aging facial creams in combination with botulinum toxin treatments achieve optimal skin regeneration and rejuvenation results. Figure 1 shows a patient with frown lines before and after treatment. Over time, the repeated use of botulinum toxin can cause a cumulative effect. Patients who receive the facial injections for a prolonged period may develop a cumulative effect and may require less-frequent injections.8
In addition, because the same muscles are targeted when injecting both therapeutically and cosmetically, there is no difference in injection location or dosage amount. Consequently, patients should be informed about cosmetic side effects when being treated therapeutically with facial injections. Smoothing of wrinkles will occur at the site of injection, and the jaw line may become slimmer when injecting into the masseter muscles.9 Patients receiving cosmetic treatments often report therapeutic benefits, such as a more relaxed face, which significantly helps improve mood and overall wellness.10 In addition, patients who receive botulinum toxin injections to treat forehead lines often report improved sleep, less headaches, and a generally happier mood.
Onset and Timing
After injection, botulinum toxin binds to the nerve within 1 to 2 hours. Clinical effects will start to be seen within 2 to 10 days and last approximately 3 to 6 months.11 After 6 months, muscle activity returns to normal and sites will require re-injection. This time frame coincides with recall appointments in dentistry, and, moreover, patients who are satisfied with results are typically eager to reschedule appointments for re-injection.
After botulinum toxin facial injections, patients are encouraged to schedule a 2-week follow-up evaluation. Images should be taken before and after treatment in case any enhancements are needed at the follow-up appointment. The clinician should advise scheduling facial injection treatment 3 to 4 weeks before any special events, in case of any swelling, bruising, or complications.
Brands and Packaging
As more products are introduced, the cost for botulinum toxin becomes more affordable for patients and easier for dentists to incorporate into practice. Currently four brands of botulinum toxin products are on the market: Botox (Allergan), Dysport® (Galderma), Jeuveau® (Evolus), and Xeomin® (Merz). Although Botox has immediate brand recognition, all four brands have the same function and mechanism of action, causing a temporary paralysis of the muscles to achieve the desired outcome.
Botulinum toxin is delivered to dental professionals in single-use 50- to 100-unit vials in its purified form, either powder or crystalline structure, and has a shelf life of approximately 1 year. To prepare for injection, botulinum toxin is mixed with bacteriostatic saline. This reconstitution process allows the user to pull the botulinum toxin into injectable syringes so it can be administered into the muscles. After the reconstitution process is complete, the product should be used within 24 hours to avoid decreased potency of the toxin.
Botox and Xeomin are nearly identical in practice in how they are mixed, measured, and injected. Dysport and Jeuveau have different reconstitution measures. Some patients and doctors may have preferences depending on name brand, price, or manufacturer promotions, so it is advisable that dental professionals be familiar with all products.
Routine Botox patients sometimes report a decreased response to the product, in the author's experience. At that time, dental professionals can switch to Xeomin, Dysport, or Jeuveau, and response rates typically revive. It is important for dental professionals to be clear with patients about brand usage. Because many people still refer to all facial injectables as Botox, dental professionals should clarify whether they are injecting another brand.
Facial Muscle Anatomy: Botulinum Toxin Function and Effects
This section presents the most common facial muscles injected with botulinum toxin, identification of each muscle, and guidelines and techniques for administering botulinum toxin injections.
Masseter Muscle
Administering botulinum toxin into the masseter muscle (Figure 2)12,13 is beneficial for patients who experience TMJD pain or migraine headaches in the temple area resulting from bruxism. Patients who experience jaw pain on opening the mouth for extended lengths of time during oral examination and treatment can also benefit from botulinum toxin injections. Injections can be scheduled 2 weeks before visits for a more comfortable experience. Otherwise, the injection, examination, and treatment can be performed concurrently. In addition to therapeutic benefits, slenderizing of the jaw is a common cosmetic side effect of botulinum toxin injections into the masseter muscle.12,13
Dental professionals can identify the masseter muscle by placing the fingers over the back side of the jaw and asking the patient to bite down and clench the teeth. The clinician will then be able to feel the masseter muscle protrude. The masseter muscle is especially easy to identify and feel in patients with masseter hypertrophy, an asymptomatic enlargement of one or both masseter muscles. The masseter can be grabbed between the thumb and index finger to inject extraorally into the muscle. Injection should always be performed bilaterally. The clinician should start with 10 to 15 units per side in a single injection (for a total of 20 to 30 units per patient) and allow up to 4 weeks to assess for effect. If desired results are not achieved within 2 to 4 weeks, additional units may be administered during the follow-up visit.14
Temporalis Muscle
Because of its location and frequent use, the temporalis (Figure 3)12,13 may be a primary focal point for recurring tension and migraine headaches caused by bruxism.15 Patients who suffer from headaches originating in the temple area can benefit greatly from botulinum toxin injections into the temporalis. Botulinum toxin can also be injected concurrently into the masseter muscle for patients who have severe clenching and grinding. In addition to the therapeutic benefits, botulinum toxin injections into the temporalis muscle also slenderize bulging temporals.16
Dental professionals can identify the temporalis muscle by using the index, middle, and ring fingers to outline the temporal fossa while the patient clenches the teeth. The clinician will then be able to feel the temporalis muscle (the temple) protrude. Injections may be directed by trigger-point or tender areas, injecting evenly in the bulkiest part of the muscle. The clinician should start with 5 units on each side (for a total of 10 units), titrating to therapeutic effect. Up to 4 weeks should be allowed to assess for effect. If desired results are not achieved within 2 to 4 weeks, additional units may be administered during the follow-up visit.16
Frontalis Muscle
Botulinum toxin injections into the frontalis muscle (Figure 4)12,13 are therapeutically beneficial for patients who hold tension in the forehead due to repeated raising of the eyebrows, typically caused by stress and resulting in tension and migraine headaches. Botulinum toxin injections into the frontalis muscle also can reduce the appearance of horizontal forehead wrinkles.
Dental professionals can identify the frontalis muscle by having the patient make a "surprised" face. At this point, horizontal forehead lines will become clear, and the frontalis muscle can be seen and felt extending down the forehead, around the eyebrows, and at the top of the nose. The clinician should start with 4 units on each side for women (for a total of 8 units per patient) and 10 units for men (for a total of 20 units per patient). Up to 4 weeks should be allowed to assess for effect. If desired results are not achieved within 2 to 4 weeks, additional units may be administered during the follow-up visit.17
Procerus Muscle
The procerus (Figure 5)12,13 moves the central brow inferiorly and medially, creating horizontal lines at the top of the nose and contributing to expressions of anger. Botulinum toxin injections into the procerus muscle can relieve tension and migraine headaches caused by this repetitive motion. Cosmetically, botulinum toxin injections into the procerus muscle can improve the appearance of frown lines between the eyebrows.17 Therapeutically and cosmetically, botulinum injections should be administered into the entire glabellar region, targeting the procerus and frontalis muscles for even balance when lowering and elevating the eyebrows.
Dental professionals can identify the procerus muscle by having the patient make a frowning face. The prominent procerus muscle can then be clearly seen and felt between the eyebrows. The muscle then can be grabbed between the thumb and index finger to prepare for injection. The clinician should start with 2 to 4 units and allow up to 4 weeks to assess for effect. If desired results are not achieved within 2 to 4 weeks, additional units may be administered during the follow-up visit.17
Corrugator Supercilii Muscle
As part of the glabellar region, tension and migraine headaches also originate from the corrugator supercilii muscle (Figure 6).12,13,18 Botulinum toxin injections can relieve this tension, as well as improve the appearance of frown lines, or "11s," between the eyes.19
Dental professionals can identify the corrugator supercilii muscle by having the patient frown. The corrugator supercilii muscle can then be seen and felt right above the eyebrow. The muscle can then be injected. Therapeutically and cosmetically, botulinum injections should be administered into the corrugator supercilii, procerus, and frontalis concurrently because the corrugator is a complementary muscle of the glabellar region. The clinician should start with 20 units (total includes injection into the frontalis and procerus muscles) and allow up to 4 weeks to assess for effect. If desired results are not achieved within 2 to 4 weeks, additional units may be administered during the follow-up visit.17
Orbicularis Oculi Muscle
Patients with migraine headaches originating from the orbicularis oculi muscle area (Figure 7)12,13 can benefit therapeutically from botulinum toxin injections.18 Injections into this area can also minimize the appearance of crow's feet.19
Dental professionals can identify the orbicularis oculi muscle by having the patient squint the eyes or smile broadly. The radial lines (wrinkles) can then be clearly seen radiating from the side of the eye. The clinician should start with 4 units on each side (for a total of 8 units) and allow up to 4 weeks to assess for effect. If desired results are not achieved within 2 to 4 weeks, additional units may be administered during the follow-up visit.20
The Yonsei Point
Botulinum toxin injections are administered into the Yonsei point (Figure 8)12,13 for the correction of excessive gingival show (more than 2 mm), or "gummy smile."21 Often, botulinum toxin injections can be even more beneficial when used in conjunction with well-planned orthodontics or cosmetic dental treatments, such as gingivectomies, crown-lengthening procedures, and veneers. Botulinum injections help relax the upper lip to prevent excessive raising on smiling; therefore, less gingiva is displayed.
Injection sites of the Yonsei point are determined by palpating the muscles during smiling and relaxing movements to ensure accurate locations of injections. The clinician should start with 2 to 3 units on each side (for a total of 4 to 9 units) and allow up to 4 weeks to assess for effect. If desired results are not achieved within 2 to 4 weeks, additional units may be administered during the follow-up visit.21
Administration Guidelines for Botulinum Toxin
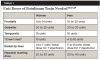
Men typically require a higher dosage of units than women because their muscles are generally stronger and more active (Table 1). Preventive injections for younger patients usually require less botulinum toxin than for older patients. On average, 30 to 50 units are needed per person to inject all muscle regions of the face, depending on the patient's needs.20
Cosmetic and Therapeutic Contraindications
Botulinum toxin injections are generally safe to administer to healthy adults. Although botulinum toxin injections are safe and temporary, some contraindications or precautions are noted for patients who are pregnant or nursing or who have hypersensitivity or allergies to ingredients including albumin human blood products, neurologic disorders such as amyotrophic lateral sclerosis (ALS, Lou Gehrig's disease), myasthenia gravis or Lambert-Eaton syndrome, flu or cold-like symptoms, or infection or dermatitis in areas being treated.22
Patient Injection
A video of a patient receiving botulinum toxin can be seen by clicking here: https://cdn.jwplayer.com/players/cb4UHgbu-Ce7nNl0O.html
Dermal Fillers
Dermal fillers can be used for patients whose cosmetic goals are no longer being addressed with botulinum toxin injections. Dermal fillers are beneficial for older patients with natural signs of aging due to decreased production of hyaluronic acid and collagen in the skin. Natural signs of aging include thinning of the dermis and atrophy of the fat pads; greater visibility of bony landmarks, blood vessels, static wrinkles, and furrows; and prominence of the nasolabial folds.23
Hyaluronic acid dermal fillers counteract signs of aging by replacing lost volume and stimulating collagen production. Common facial locations that can benefit from dermal fillers are down-turned smile lines, marionette lines, lips (enhancements), and cheeks (replacement of volume) (Figure 9). Dermal fillers are technique sensitive, and most states require hands-on training as part of the certification process.
Dermal fillers differ in hyaluronic acid concentration, particle size, cross linking, density, and duration. Some hyaluronic acid fillers contain lidocaine that simultaneously numbs the area on injection. Dentists can also anesthetize patients beforehand with inhalational anesthetics or mental nerve blocks, although it should be noted that pre-anesthetized patients may experience swelling at the site, which can lead to injecting less filler than needed for desired results.24 Depending on site, patient age, and indication, dental professionals should be familiar with all dermal filler materials. High-density, enlarged-particle fillers are recommended for deep dermal injections for deep-set static wrinkles, while low-density, small-particle fillers are recommended for finer lines.24
Dermal fillers are versatile, are degradable, and will dissipate over time, with effects lasting from 6 months to a year. Because they are reversible, dermal fillers are a safe and comfortable introduction to the cosmetic facial arena for both dentists and patients. If a mistake is made, injectable medications called hyaluronidases are available to correct any misapplication.25 Moreover, if clinicians inject into the wrong location or patients are unhappy with the esthetic outcome, concerns will be alleviated as the effects diminish within 6 months.
Conclusion
Dentists are ideal candidates to administer facial injectables. They are extremely knowledgeable in the anatomy of the head and neck and are highly skilled at patient comfort when injecting into these areas. Offering facial injections provides a valuable alternative solution for patients suffering from TMJD issues when traditional therapies have failed.
Facial injections also provide an attractive patient incentive to visit the dentist more regularly, in turn increasing the revenue stream for the dentist. Moreover, patients no longer have to resort to visiting more than one healthcare provider to receive facial injectables for cosmetic and therapeutic treatments; both can take place in one visit in a single office, saving time and money.
Being one of the first dental offices in the area to offer facial injections is a distinguishing factor for a dental practice. It can greatly increase patient referrals and facilitate networking and collaborative care opportunities with local plastic surgeons and chiropractors who deal with TMJD and cosmetic treatments, further establishing dental practitioners as facial injection experts.
About the Author
Bianca Velayo, DMD is a 2015 graduate of Tufts University School of Dental Medicine. She is the owner of Green Valley Smiles Dentistry, Henderson, Nevada. She serves as a subject-matter expert in facial injectables for the PDS University Institute of Dentistry and has been administering facial injectables since 2016.
References
1. International Society of Aesthetic Plastic Surgery (ISAPS). International Study on Aesthetic/Cosmetic Procedures Performed in 2016. ISAPS website. https://www.isaps.org/medical-professionals/isaps-global-statistics/. Published June 2017. Accessed April 5, 2018.
2. BOTOX mechanism of action. Allergan website. https://www.botoxmedical.com/FocalSpasticity/Efficacy/MechanismOfAction. Updated April 2017. Accessed June 3, 2020.
3. Nayyar P, Kumar P, Nayyar PV, Singh A. BOTOX: Broadening the horizon of dentistry. J Clin Diagn Res. 2014;8(12):ZE25-9.
4. Murali RV, Rangarajan P, Mounissamy A. Bruxism: conceptual discussion and review. J Pharm Bioallied Sci. 2015; 7(suppl):S265-S270.
5. Pihut M, Ferendiuk E, Szewczyk M, et al. The efficiency of botulinum toxin type A for the treatment of masseter muscle pain in patients with temporomandibular joint dysfunction and tension-type headache. J Headache Pain. 2016;17:29.
6. Satriyasa BK. Botulinum toxin (Botox) A for reducing the appearance of facial wrinkles: a literature review of clinical use and pharmacological aspect. Clin Cosmet Investig Dermatol. 2019;12:223-228.
7. Casale R, Tugnoli V. Botulinum toxin for pain. Drugs R D. 2008;9(1):11-27.
8. Frick CG, Richtsfeld M, Sahani ND, et al. Long-term effects of botulinum toxin on neuromuscular function. Anesthesiology. 2007;106(6):1139-1146.
9. Aguilera SB, Brown L, Perico VA. Aesthetic treatment of bruxism. J Clin Aesthet Dermatol. 2017;10(5):49-55.
10. Lewis MB, Bowler PJ. Botulinum toxin cosmetic therapy correlates with a more positive mood. J Cosmet Dermatol. 2009;8(1):24-26.
11. Nigam PK, Nigam A. Botulinum toxin. Indian J Dermatol. 2010;55(1):8-14.
12. OpenStax. Axial muscles of the head, neck and back. In: Anatomy and Physiology. Rice University. https://opentextbc.ca/anatomyandphysiology/chapter/11-3-axial-muscles-of-the-head-neck-and-back/. Published March 6, 2013. Accessed June 4, 2020.
13. Mostafa D. Botulinum toxin in dentistry. In: Serdev N, ed. Botulinum Toxin. IntechOpen. https://www.intechopen.com/books/botulinum-toxin/botulinum-toxin-in-dentistry. Published November 5, 2018. Accessed June 4, 2020.
14. Moore AP, Wood GD. The medical management of masseteric hypertrophy with botulinum toxin type A.
Br J Oral Maxillofac Surg. 1994;32(1):26-28.
15. Asutay F, Atalay Y, Asutay H, Acar AH. The evaluation of the clinical effects of botulinum toxin on nocturnal bruxism. Pain Res Manag. 2017;2017:6264146.
16. Kwon KH, Shin KS, Yeon SH, Kwon DG. Application of botulinum toxin in maxillofacial field: part I. Bruxism and square jaw. Maxillofac Plast Reconstr Surg. 2019;41(1):38.
17. Carruthers J, Fagien S, Matarasso SL; Botox Consensus Group. Consensus recommendations on the use of botulinum toxin type a in facial aesthetics. Plast Reconstr Surg. 2004;114(6 suppl):1S-22S.
18. Oliver M, MacDonald J, Rajwani M. The use of botulinum neurotoxin type A (Botox) for headaches: a case review. J Can Chiropr Assoc. 2006;50(4):263-270.
19. Tremaine AM, McCullough JL. Botulinum toxin type A for the management of glabellar rhytids. Clin Cosmet Investig Dermatol. 2010;3:15-23.
20. Anido J, Arenas D, Arruabarrena C, et al. Tailored botulinum toxin type A injections in aesthetic medicine: consensus panel recommendations for treating the forehead based on individual facial anatomy and muscle tone. Clin Cosmet Investig Dermatol. 2017;10:413-421.
21. Srivastava S, Kharbanda S, Pal US, Shah V. Applications of botulinum toxin in dentistry: a comprehensive review. Natl J Maxillofac Surg. 2015;6(2):152-159.
22. Botox [prescribing information]. FDA website. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/103000s5236lbl.pdf. Updated 2011. Accessed June 4, 2020.
23. Coleman SR, Grover R. The anatomy of the aging face: volume loss and changes in 3-dimensional topography. Aesthet Surg J. 2006;26(suppl 1):S4-S9.
24. Walker K, Basehore BM, Goyal A, et al. Hyaluronic Acid. Treasure Island, FL: StatPearls Publishing; 2020. https://www.ncbi.nlm.nih.gov/books/NBK482440/. Accessed June 4, 2020.
25. King M, Convery C, Davies E. This month's guideline: the use of hyaluronidase in aesthetic practice (v2.4). J Clin Aesthet Dermatol. 2018;11(6):E61-E68.
26. Dhaked RK, Singh MK, Singh P, Gupta P. Botulinum toxin: bioweapon & magic drug. Indian J Med Res. 2010;132(5):489-503.
27. Kwon KH, Shin KS, Yeon SH, Kwon DG. Application of botulinum toxin in maxillofacial field: part I. Bruxism and square jaw. Maxillofac Plast Reconstr Surg. 2019;41(1):38.
28. Jankovic J, Albanese A, Atassi MZ, et al. Botulinum Toxin. Philadelphia, PA: Saunders; 2009.