You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The first dental hygiene school was founded by Dr. Alfred C. Fones in 1913. Dental hygiene students were educated in "mouth hygiene" and instrumentation techniques to remove "plaque, stain and tartar" accretions on the teeth.1 Fones's vision was for this professional to provide preventive oral health care in a variety of public health settings, such as infirmaries, schools, dental private offices, and public clinics.1 The dental hygiene profession continues to have a primary focus on oral disease prevention in a variety of settings; however, education in mouth hygiene and instrumentation alone is no longer sufficient for oral disease prevention. Significant advances in health science research have identified a multitude of systemic conditions that contribute to oral diseases.2-4 It is now understood that localized biofilm and calculus removal are only one of the factors to consider in oral disease prevention.5-7 Ongoing evidence-based research has established oral-systemic correlations, including bidirectional relationships between diabetes and periodontitis;7,8 cardiovascular conditions and periodontal disease;9,10 increased susceptibility of immunocompromised patients to oral infection;11,12 and increased caries risk due to medication induced xerostomia.13,14 These correlations require dental hygienists to have additional scientific knowledge to understand oral-systemic relationships and host-inflammatory responses in order to make appropriate recommendations for preventing and treating oral disease.
Technology utilized by dental hygienists has changed dramatically since the profession was established in 1913. The available consumer options of a few manual toothbrushes has grown exponentially into an abundance of choices ranging in size, shape, and bristle type. Power toothbrushes are commonly used and require a different brushing technique. Over-the-counter rinses, toothpastes, and whitening products require professionals to be aware of the potential chemical reactions between products and adverse reactions in the oral cavity. Oral cancer screening devices have been created to enhance visualization of abnormalities within the oral cavity,15,16 and salivary diagnostic testing provides a means to identify specific microorganisms associated with oral disease.17,18 Oral health care providers must be able to understand current research in evaluating the scientific evidence and appropriateness of these devices and tests for clinical practice.15,16
Advancements in assessment instruments and treatment procedures require additional training beyond the traditional methods. Periodontal probing devices now allow the dental hygienist to enter information by foot or voice controls.19 Clinical procedures within the oral cavity are enhanced by power driven instrumentation, laser therapy, and perioscopes.20-22 Electronic dental programs are commonly used to record the patient's assessment and treatment information.23
Access to oral health care has increased as a result of technology supported teledentistry enabling patients in rural locations to receive oral health care provided by oral health care professionals while the dentist is in a different location.24 Providing oral health care in remote settings requires an increased emphasis on the development of critical thinking skills as part of the dental hygiene education process.25 These skills are particularly important in teledentistry for the identification of general health conditions requiring medical referrals as well as the oral conditions for review by a virtual dental home dentist.25-27 Looking beyond patient care and the clinical role of the dental hygienist, six other roles or specialty areas for the profession have been identified: research, corporate, public health, educator, administrator, and entrepreneur. These roles provide dental hygienists with increased responsibilities and opportunities to work in a wide range of settings outside of clinical practice.28,29
Advancements in oral health care and technology, as well as expanding professional roles, have required changes in dental hygiene education standards. The Commission on Dental Accreditation (CODA) is the current accrediting body responsible for dental hygiene education. In 1975, the newly formed CODA established the requirements for dental hygiene education programs and identified a two year minimum for completion.30 While CODA has modified and expanded education standards, the commission has not made any changes in the minimum number of years for completion.
Currently, all dental hygiene students are required to meet the same educational standards; however, they are not awarded the same degree. For example, CODA Standard 2.8 refers to the required inclusion of content specific to four areas: general education, biomedical sciences, dental sciences, and dental hygiene sciences. General education content includes oral and written communication, psychology and sociology; and biomedical sciences includes anatomy, physiology, chemistry, microbiology, nutrition, and pharmacology.30 Both the general education and biomedical science coursework would be considered prerequisites prior to beginning a dental hygiene education program. The dental sciences include course content areas related to tooth morphology, oral embryology and histology, oral pathology, radiography, periodontology, and pain management; while health promotion, clinical dental hygiene, community oral health, medical and dental emergencies, legal and ethical issues, and infection and hazard control management fall under dental hygiene sciences, all completed as part of the dental hygiene education program.30 While all dental hygiene programs must adhere to the education content required by Standard 2.8, students receive either an associate's or a bachelor's degree upon program completion.
A recent retrospective study identified dental hygiene students are completing educational requirements exceeding the degrees granted.31 O'Hehir compared the number of educational hours currently required for associate and baccalaureate degree programs in the state of Arizona to those required in 1945. Historically, educational hours were discussed as contact hours. For the purposes of comparison, current credit hour requirements were converted to contact hours. O'Hehir's findings showed that a two-year dental hygiene program required a total of 112 contact hours in 1945 as compared to the current 157 contact hours for associate programs and 170 contact hours for bachelor programs in Arizona.31 Dental hygiene students receiving an associate degree are completing approximately 45 contact hours more than what was required in 1945 and are dedicating nearly the same number of contact hours as baccalaureate degree students. O'Hehir concludes that today's dental hygiene student deserves to be awarded the degree that accurately reflects their education.31
One barrier associate degree students may encounter upon completion of the additional required credits for a baccalaureate degree is the institution in which the dental hygiene program is located. Various educational institutions (i.e., community colleges, technical colleges) may not have the ability to grant a baccalaureate degree. To address this barrier, two current options are available, dual enrollment and degree completion. Dual enrollment is a partnership between the educational institution offering the dental hygiene associate degree and another university.32 Students enrolled in the associate degree program would concurrently enroll in the partnering university to concurrently complete the necessary credits for a baccalaureate degree. A second option is a degree completion program, which does not usually occur concurrently with the associate degree curriculum. Degree completion programs are typically intended for licensed dental hygienist who graduated with an associate's degree and would like to earn a bachelor degree.33
The American Dental Hygienists' Association (ADHA) recognizes the need for dental hygiene education related to increased roles, responsibilities and workforce models. In 2017, ADHA approached the Commission on Dental Accreditation (CODA) and proposed revisions to Standard 2-1 related to entry level dental hygiene education and Standard 3-7 related to faculty education requirements (master's degree or higher) for teaching didactic courses. In their response, CODA requested an impact study related to these proposed changes, including assurance that every CODA accredited dental hygiene program director had an opportunity to provide comment.34 As a means to provide an avenue for all dental hygiene program directors to provide input on the proposed changes, an electronic survey was developed to examine viewpoints of entry-level dental hygiene program directors concerning various aspects of elevating the degree required for entry into dental hygiene practice to the baccalaureate degree within their institution as well as their viewpoints regarding the requirement of a master's degree or higher for teaching didactic courses. The purpose of this study was to identify entry-level dental hygiene program directors' perceptions regarding advancing accreditation standards in dental hygiene education.
Methods
An exploratory, descriptive, cross-sectional study was designed to assess entry-level program directors' perceptions of changes to accreditation standards using an original 19-item survey instrument. Variables addressed included the following: type of entry-level dental hygiene program, program setting, program director demographics, and dimensions related to elevating the degree required for entry into dental hygiene practice to the baccalaureate degree. The survey was reviewed by a subset of expert dental hygiene faculty, researchers, and participants from the American Dental Hygienists' Association (ADHA), to establish content validity. The survey was also reviewed by a measurement expert and biostatistician to ensure congruency with survey items and research questions. Feedback was provided and modifications were made. The study design and survey underwent IRB review and was approved by the Idaho State University Human Subjects Committee (IRB-FY2019-100).
Dental hygiene program directors from 332 entry-level dental hygiene programs (n=332) were invited to participate in the survey. Qualtrics® (Provo, UT) was used to distribute the questionnaire via three electronic mailings during the spring of 2019. All surveys were confidential and included an informed consent form. Descriptive statistics and chi-square analysis were used to analyze results. To hold the familywise error rate to p=.05, the Bonferroni adjusted criterion for statistical significance for each test was established as p=.01. When there were cells with expected frequencies less than 5, the Bonferroni adjusted criterion for statistical significance was established as p=.0125.
Results
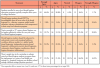
A total of 178 responses were received (n=178) for a response rate of 53.6%. A majority (n=164, 92%) of individuals were female, have been involved in dental hygiene education on average for 20 years (range: 3-45 years), and have been a program director for an average of 8 years (range: 1-38 years). Nearly three-quarters (n=130, 73%) of the program directors held a master's degree. Respondent demographics are shown in Table I.
Program directors were asked to identify the degree awarded upon completion of the dental hygiene program at their school, type of institution, and location of the program. The majority of respondents indicated that their entry-level programs granted an associate degree (n=139, 78%), while one-fifth (n=38, 21%) were from baccalaureate degree programs. The distribution of these results was representative of the available ADHA data on the U.S. dental hygiene programs showing that 82.5% (n=274) offer associate degrees and 17.5% (n= 58) offer baccalaureate degrees. Most programs (n=102, 57%) were housed in a community college (n=102, 57.3%), located in an urban setting (n=75, 42%).
Perceptions of dental hygiene education
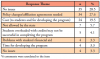
Five items related to dental hygiene education were presented in a Likert format at the beginning of the survey (Table II). Respondents were asked to identify the extent to which they agreed or disagreed with each statement. Most program directors agreed or strongly agreed that students enrolled in dental hygiene education programs typically complete three years of college education (n=152, 85.4%), that students should not be knowledgeable about all seven roles of the dental hygienist in their entry-level education program (n=147, 82.6%), and should be educated to understand current and emerging workforce delivery models (n=166, 93.2%). Respondents were divided in agreement on whether topics essential to 21st century dental hygiene practice can be taught sufficiently within the two-year entry-level dental hygiene program, and more than half of the respondents disagreed regarding the statement that there is ample time in the curriculum to educate entry-level students to prepare them for employment in a variety of oral healthcare settings (n=94, 52.9%). Respondents were provided space within the survey to comment on any of the five statements and over 80 comments were made. The majority of comments were pertaining to the issue of time within the curriculum to adequately educate entry-level dental hygiene students; examples are shown in Table III.
A chi-square test of association was used to determine whether there was an association between the responses to the statements regarding dental hygiene education and degree offered (associate versus baccalaureate) by the entry-level program (Table IV). Program directors from associate degree institutions tended to agree that students enrolled in entry-level programs typically complete three years of college education (89.2% vs 71%) and while more respondents from baccalaureate programs tended to disagree with this statement than those from associate programs (26.4% vs 5.7%). Respondents from associate degree programs also tended to agree that topics essential to 21st century dental hygiene can be taught sufficiently within the two-year entry-level program as compared to cohorts from baccalaureate programs (47.5% vs 7.9%). Lastly, more respondents from associate degree programs agreed that there is ample time in the curriculum to educate students to prepare them for employment in a variety of oral health care settings than those from baccalaureate degree programs (43.9% vs 10.5%).
A chi-square test of association was conducted to identify whether there was an association between responses to the statements about dental hygiene education and type of institution and location of entry-level dental hygiene program. Statistical significance was found for the statement regarding the ability to teach topics essential to 21st century dental hygiene within the two-year entry level dental hygiene program and type of institution (Fisher's Exact Test 13.26, df=4, p=.009, Cramer's V =.28). Significance was set at .01 level, with a familywise error rate equal to .05. No other areas of statistical significance were found between the remaining statements and the demographic variables.
Baccalaureate degree option
Respondents were asked if their educational institution/department offered or have they thought about offering a baccalaureate degree option for their dental hygiene entry-level program. Nearly half of the respondents (n=84, 47.2%) indicated "yes," while one-third (n=58, 32.6%) replied "no," and nearly one-fifth (n=34, 19.1%) chose "possibly." Statistical significance was found regarding the type of degree awarded (associate versus baccalaureate: X2 41.40, df=2, p<.000, Cramer's V = .485) and the responses to this item. More respondents from programs granting a baccalaureate degree have considered offering/offer a baccalaureate degree as compared to those from an associate degree program (94.6% vs 35.3%). Statistical significance was also noted between the responses and type of institution (community college, technical school, university/college with a dental school, university/college without a dental school: X243.70, df=6, p<.000, Cramer's V -.353). In this case more respondents from community college settings chose "no" as compared to the other institution types (77.6% vs 22.3%) and more respondents from community college settings chose "possibly" than respondents from other institution types (73.5% vs 26.5%).
A majority of respondents (n=133, 74.7%) made comments related to considering a baccalaureate degree option for their institution. Of those respondents currently offering a baccalaureate degree option (n=57, 42.9%) and those offering entry-level, degree completion and dual enrollment, comments were in favor of having a baccalaureate degree option (n=46, 34.6%). Conversely about one-fifth (n=30, 22.6%) offered comments against having a baccalaureate degree, entry-level program. Respondent comments were primarily related to their institution being unable to offer a bachelor's degree either due to state regulations or pressure from the dental school, lack of understanding the concepts of articulation agreements/dual enrollments, higher cost of tuition, and concerns about possible lower enrollment.
Respondents were also asked whether there were elements about a baccalaureate entry-level dental hygiene education that would be more valuable than the current entry-level dental hygiene education. Most individuals (n=176) replied to this item with more than half (n=95, 53.4%) responding "yes," and one-fifth (n=35, 19.7%) indicating "no," and one-fourth (n=46, 25.8%) indicating "possibly." Statistical significance was found related to type of degree awarded and responses (X2=27.14, df=2, p<.000, Cramer's V=.393). More respondents from programs offering a baccalaureate degree responded favorably to this item as compared to those from associate degree programs who answered "yes" to this item (91.9% vs 43.9%). Of the open-ended comments (n=119), one-fifth (n=24, 20.2%) indicated feeling that the associate degree was sufficient for clinical practice of an entry-level dental hygienist, and if the graduate wanted to do something outside of clinical practice, they could obtain additional education through a degree completion program. Additionally, several individuals (n=7, 5.9%) stated that the associate degree was more valuable because of its reduced cost to the students. Conversely, slightly more than half (n=65, 54.6%) of respondents perceived the value of a baccalaureate degree to be more beneficial due to the increased time to allow for students to synthesize and apply materials, develop critical thinking and professional skills, and increase career opportunities following graduation. Others (n=23, 19.3%) commented on the added benefits of increased learning opportunities in a variety of settings and populations found through baccalaureate education.
Institutional issues related to the consideration of a baccalaureate degree or a dual enrollment articulation agreement responses and themes are shown in Table V. The range of comments included: no issues, policy changes and/or affiliation agreements would be needed, or there were cost concerns for students and for developing the program if dual enrollment or a baccalaureate degree were to be offered.
Accreditation changes
Another survey item specifically addressed the ADHA proposed accreditation change to Standard 2-1 elevating the required entry-level degree for dental hygiene to the baccalaureate degree. Respondents were asked to indicate whether they could support this advancement in dental hygiene education. Forty-four percent (n=79) of the respondents supported the baccalaureate degree for entry into the profession, while 39.3% (n= 70) did not support the change from the associate's degree level, and 16.3% (n=29) responded "possibly." A chi-square test was conducted to determine if associations existed between responses to this item and demographic variables. Statistical significance found in responses related to type of degree awarded and the respondent's academic institution (X2=40.48, df=2, p<.000, Cramer's V= .478). Respondents from programs offering a baccalaureate degree tended to support the accreditation change more frequently than respondents from programs offering an associate degree (89.5% vs 31.7%).
Program directors were offered an opportunity to add comments (n=114) related to this accreditation change item and nearly half (n=56, 49.1%) were favorable towards the baccalaureate degree for entry into the profession. Most comments related to the need to advance the profession and provide students with additional time for educational learning. Several (n=5, 8.9%) program directors stated that it would be important for students to receive the degree they deserve from the amount of credits required in their programs. Conversely, half of the respondents (n=58, 50.9%) did not support the baccalaureate degree for entry-level. Regarding maintaining the associate's degree for entry-level, 22% (n=13) preferred having both the associate and baccalaureate options for students while an equal number (n=13, 22%) did not support the higher degree due to increased costs to students. Others were concerned that programs would be closed (n=11, 18.6%) or felt that the associate degree provided sufficient education for clinical practice (n=10, 17.0%). Several (n=5, 8.5%) expressed concern that student enrollment would decrease. Selected respondent quotes are displayed in Table VI.
Respondents were asked regarding what changes would be required to maintain CODA accreditation if they were to offer an entry-level dental hygiene baccalaureate degree at their institution. Of the 123 responses, one-third (n=41, 33.3%) focused on the need for a change in curriculum and/or faculty with advanced degrees, while others (n=20, 16.4%) stated they would be unable to offer a baccalaureate degree and their program would close. Some respondents (n=14, 11.4%) indicated that legislative changes and/or affiliation agreements with neighboring institutions would be required while a similar number (n=15, 12.2%) were unsure of what changes would be required.
The survey item asked about revising Standard 3-7 to require all full-time and part-time faculty providing didactic instruction hold a master's degree or higher. Respondents were asked to indicate agreement on the importance of revision; nearly three-fourths (n=130, 73%) agreed while a little more than one-fourth (n=47, 26.4%) were not in agreement. Statistical significance was found only related to the respondents type of institution (X2=12.77, df =3, p=.005, Cramer's V=.270). Respondents from associate degree and technical programs selected "no" more frequently than those from programs in university/colleges with or without a dental school (63.6% vs 15.3%). In general, most individuals supported changing Standard 3-7 and there were no differences between the groups in regard to demographic variables. Over half (65%, n=115) of the respondents offered comments ranging from agreement for this change (n=52, 45.2%), already require a master's degree for faculty providing didactic instruction (n=30, 26.1%), difficult to find qualified educators (n=22, 19.1%), emphasis should be on teaching methodology (n=19, 16.5%).
Discussion
Dental hygiene program directors were provided an opportunity to respond to statements regarding elevating dental hygiene education accreditation standards. While there were variations in agreement and a multitude of comments provided, two key assertions were noteworthy. First, program directors discussed time as an overriding concern. It takes a minimum of three years, not two, to complete the dental hygiene education program and the majority of students earn an associate's rather than a baccalaureate degree for their investment in their education. Furthermore, there is not enough time in the curriculum to adequately teach all of the required concepts. Second, respect is correlated with the degree awarded. Students may come close to earning a baccalaureate degree but are not able to command the respect from other health care professionals because they do not obtain that degree. They are not comparable with other health care disciplines nor can they expect to be without the credentials of a baccalaureate degree. These sentiments have been expressed since the 1980s.28,29,35
Respondents expressed mixed opinions concerning proposed changes to Standard 2-1 (curriculum requirements and degree awarded). Those who responded in agreement identified increased course requirements, insufficient time for students to synthesize and apply educational materials, and increase workforce models as the main reasons for agreeing to the change. It is encouraging that many dental hygiene educators are aware of the need to increase educational requirements and prepare professionals capable of becoming the primary source to address the access to oral health care problem in America. Over 47 million people in the United States live in areas with limited access to dental care.36 Poor oral health increases the risk for a plethora of systemic conditions including diabetes, rheumatoid arthritis, premature births, cardiovascular disease (endocarditis), gastrointestinal disorders, and an increased risk for pneumonia in the elderly.36 Due to these correlations, the medical profession is beginning to identify the need for dental hygienists to be part of collaborative patient care. In the call to action for the inclusion of the dental hygiene profession into the U.S. health care system, Vanderbilt et al underscored the need for educational qualifications that will enable dental hygienists to safely provide the scope of care and services as part of their expanded professional roles, along with the ability to effectively participate as members of interprofessional teams.36
In contrast, program directors from institutions not in agreement with changing the accreditation standards stated the associate's degree is sufficient for a "clinical hygienist" and graduating students would not be paid more by the dentist if they had an advanced degree. In addition, many stated if the student preferred to have a different career besides "clinical dental hygiene" they should have the choice to seek further education. Respondents were clear in expressing the opinion that "clinical hygienists" obtaining associate degrees save money on tuition. Although clinical dental hygiene remains an important aspect of the profession, advances have been made since the time scaling and root planing was considered the primary treatment for restoring and maintaining oral health. Currently, 42 states allow dental hygienists to provide preventive oral health care services without the presence or direct supervision of a dentist.37 This correlates with 84% of the states allowing community-based workforce models. Dental hygiene students should be educated to become primary care providers for underserved populations.28,29 Other comments opposing advancing the required entry-level degree was that the institution cannot offer a baccalaureate degree and would be "shut down." These perceived barriers could be addressed by providing more education to program directors about affiliation agreements, dual enrollment and/or degree completion programs.
Significant support was identified for the proposed changes to Standard 3-7 (requirement of dental hygiene educators to hold a master's degree or higher). Dental hygiene educators holding a master's degree are a valuable asset to students as shown by the Stanley et al study, which identified the importance of evidence-based decision making as a critical component of the dental hygiene curriculum.38 In this study, educators with a master's degree demonstrated an increased ability and confidence to teach evidence-based decision making compared to educators with a baccalaureate degree.38
Discussions regarding the baccalaureate degree as entry-level to the profession have been ongoing since the mid 1980s when the ADHA published its Prospectus for Dental Hygiene and dental hygiene practice workshops were provided to educators and clinicians.35 ADHA policy supporting baccalaureate dental hygiene education has been in existence for 33 years;39 when it was acknowledged that health care and workforce models were changing and dental hygiene education needed to advance so dental hygiene students would be prepared to function in new environments and with other healthcare providers. This scenario has become even more significant, and if ever there was a time for advanced education of entry-level dental hygiene students, it is now. Health care, technology, industry, economy, all will continue to evolve. Other health care professions have adapted their education standards to meet these ever-evolving systems. The question remains when will the profession of dental hygiene recognize the need to change and adapt irrespective of which organization controls accreditation standards.
Although this research provided insight into dental hygiene program directors perspective on the need to advance the entry-level dental hygiene degree, a limitation was the lack of a validated survey instrument. However, content validity was established and opportunities for comments were offered throughout the survey following each item. Additionally, some respondents may not have clearly understood that the purpose of this study was to respond to CODA's request for information about changes to elevate the accreditation standards. Some comments reflected concern that the researchers were trying to change the accreditation standards rather than gather information to assist another organization (CODA) in their decision making. Strengths of the study include the response rate and reflective nature of the comments provided.
This research serves as a reference point for understanding issues related to entry-level baccalaureate dental hygiene education and changes to accreditation standards. Further research should include the perceptions of dental hygiene educators at large regarding this change. Examining the perspectives of key leaders in the profession would provide a dynamic qualitative study. Additionally, a comparison study of the curriculum of entry-level programs offering associate degrees versus baccalaureate degrees would be valuable in determining the extent of differences between courses taught, and preparation to work as primary care providers in various workforce models for diverse populations.
Conclusion
Program directors of entry-level dental hygiene programs were surveyed to determine their perceptions of advancing accreditation standards. Respondents were equally divided concerning changing the accreditation standard for the entry-level degree from an associate's degree to a baccalaureate degree, but were in support of modifying the accreditation standard to requiring educators to have a master's degree for teaching didactic courses. Further research is needed to include dental hygiene educators' and key leaders' perspectives to provide comparative information and a greater understanding regarding increasing accreditation standards.
Acknowledgement
The authors received a research grant from the ADHA Institute for Oral Health to support the conduct of this study.
About the Authors
JoAnn R. Gurenlian, RDH, MS, PhD, is a professor and Graduate Program Director, Department of Dental Hygiene; Rachelle Williams, RDH, MS, is an assistant professor and Senior Clinic Coordinator, Department of Dental Hygiene; both at Idaho State University, Pocatello, ID.
Corresponding author: JoAnn R. Gurenlian, RDH, MS, PhD; gurejoan@isu.edu
References
1. Gadbury-Amyot CC, Nathe CN. The intersection of education and technology at the century mark. J Dent Hyg. Jan; 87: Suppl 1:44-9.
2. Brennan DS, Keuskamp D, Balasubramanian M, Amarasena N. General health and well-being among primary care patients aged 75+ years: associations with living conditions, oral health and dependency. Australas J. Ageing. 2018 Mar;37(1):E1-E6.
3. Critchlow D. Part 3: impact of systemic conditions and medications on oral health. British J Com Nurs. 2017 Apr;22(4):181-90.
4. Lalla E, Papapanou PN. Diabetes mellitus and periodontitis: a tale of two common interrelated diseases. Nat Rev Endocrinol 2011 Jun 28;7(12)738-48.
5. Zhang Z, Zhao D, Lin M et al. Application of health quotient to enhance chronic periodontitis treatments. Patient Preference and Adherence. 2018 Mar;12:359-62.
6. Chatzopoulos GS, Cisneros A, Sanchez M et al. Validity of self-reported periodontal measures demographic characteristics and systemic medical conditions. J Periodontol. 2018 Aug;89(8):924-32.
7. Chapple IL, Borgnakke WS, Genco RJ. Hemoglobin A1c levels among patients with diabetes receiving nonsurgical periodontal treatment. JAMA 2014 May;311:1919-20.
8. Borgnakke WS. Hyperglycemia/diabetes mellitus and periodontal infection adversely affect each other. In Genco RJ & Williams RC. Periodontal disease and overall health: a clinician's guide, 2nd ed. Yardley, PA: Professional Audience Communications, Inc; 2014. p. 99-122.
9. Dhotre S, Jahagirdar V, Suryawanshi N et al. Assessment of periodontitis and its role in viridans streptococcal bacteremia and infective endocarditis. Ind Heart J. 2018. 70:225-32.
10. Souza AF, Rocha AL, Castro WH et al. Dental management for patients undergoing heart valve surgery. J Card Surg. 2017 Oct;32(10):627-32
11. Barreto D, Milo dos Santos M, Gomes Bda S et al. Periodontal conditions in human immunodeficiency virus-positive patients under highly active antiretroviral therapy from a metropolitan area of Rio De Janeiro Luis Paulo. J Periodontol 2016 Apr;87(4):338-45
12. Nobre AVV, Pólvora TLS, Silva LRM, et al. Effects of non-surgical periodontology therapy on clinical and immunological profile and oral colonization of Candida spp in HIV-infected patients with chronic periodontitis. J Periodontol. 2019 Feb; 90:167-76
13. Manlapaz HJ. Implications of xerostomia and caries in community-dwelling older adults. Can J Dent Hyg. 2017 Oct;51(3):126-31
14. Nguyen CT, Lin S, Clark H, Hovan A et al. Salivary flow rate after conventional and intensity modulated radiation therapy. J Am Dent Asso. 2018 Jun;149(6):432-41
15. Lingen MW, Tampi MP, Urquhart O, et al. Adjuncts for the evaluation of potentially malignant disorders in the oral cavity. J Am Dent Asso. 2017 Nov;148(11):797-813.
16. Lingen, MW, Abt E, Agrawal N, et al. Evidence-based clinical practice guideline for the evaluation of potentially malignant disorders in the oral cavity. J Am Dent Asso. 2017 Oct;148(10):712-27.
17. Comstedt R. Tailored treatment: evaluation of salivary diagnostics. RDH. Oct 2018;38(10):37-39.
18. Numan R, Lantz K, Filimon T et al. Patient attitudes regarding salivary genetic biomarker and periodontal pathogen testing. J Dent Hyg. 2017 Apr;91(2):71-2.
19. Renatus A, Trentzsch L, Schönfelder A et al. Evaluation of an electronic periodontal probe versus a manual probe. J Clin Diag Research. 2016 Nov;10(11): ZH03-ZH07
20. Bowen DM. Lasers and nonsurgical periodontal therapy. J Dent Hyg. 2015 Aug;89(4):206-09
21. Hinchman S, Funk A, DeBiase C et al. Ultrasonic instrumentation instruction in dental hygiene programs in the United States. J Dent Hyg. 2016 Apr;90(2):135-42
22. Mangia C. Calculus detection tools- a review. HECS Int J Com Health Med Res. 2018 July-Sep;4(3):53-58
23. Abramovicz-Finkelsztaina R, Barsottinia CGN, Marina HF. Electronic dental records system adoption. Medinfo. IOS Press., Database: Complementary Index 2015:17-20.
24. American Dental Association. ADA guide to under-standing and documenting teledentistry events [Internet] Chicago; American Dental Association; [cited 2019 May 20]. Available from: https://www.ada.org/~/media/ADA/Publications/Files/D9995andD9996_ADAGuidetoUnderstandingandDocumentingTeledentistryEvents_v1_2017Jul17.pdf
25. Summerfelt F. Teledentistry-assisted, affiliated practice for dental hygienists: an innovative oral health workforce model. J Dent Educ. 2011 Jun;75(6):733-42.
26. Daniel SJ, Kumar SK. Teledentistry: a key component in access to care. J Evid Base Dent Pract. 2014 June;14(1):201-08.
27. McFarland KK, Nayar P, Chandak A, Gupta N. Formative evaluation of a teledentistry training programme for oral health professionals. Eur J Dent Educ. 2018 May;22(2):109-14.
28. American Dental Hygienists' Association. Transforming dental hygiene education and the profession for the 21st century [Internet]. Chicago: American Dental Hygienists' Association; 2015 [cited 2019 Sep 9] Available from https://www.adha.org/resources-docs/Transforming_Dental_Hygiene_Education.pdf
29. Brickle CM. Advancing dental hygiene education: what does research tell us about the future of dental hygiene? J Dent Hyg. 2018 Oct;92(5):4-5.
30. Commission on Dental Accreditation. Accreditation standards for dental hygiene education programs. [Internet]. Chicago: Commission on Dental Accreditation; 2018 [cited 2019 May 20] Available from: https://www.ada.org/~/media/CODA/Files/2019_dental_hygiene_standards.pdf?la=en
31. O'Hehir T. Dental hygiene education exceeds the degrees granted: A pilot study. Int J Dent Hyg. 2018 Aug; 16:340-8.
32. ADEA: Bulletin in dental education [Internet]. Washington, DC: American Dental Education Association; c2013-2019 [cited 2019 May 20]. Available from: https://www.adea.org/ADEA/Blogs/Bulletin_of_Dental_Education/Minnesota_State_Launches_Innovative_Dual_Admissions_Dental_Hygiene_Bachelor_s_Program.html
33. American Dental Education Association. Degree completion programs in dental hygiene [Internet]. Washington, DC: American Dental Education Association; c2013-2019 [cited 2019 May 20]. Available from: https://www.adea.org/about_adea/who_we_are/Degree_Completion_Programs_in_Dental_Hygiene.aspx
34. Livingston, Harold M. (Commission on Dental Accreditation, Chicago, IL). Letter to: Ann Battrell (American Dental Hygienists' Association, Chicago, IL). 2017 Aug 23. 6 paragraphs.
35. American Dental Hygienists' Association. Prospectus for Dental Hygiene. Chicago (IL): American Dental Hygienists' Association; 1998 April. 50 p.
36. Vanderbilt AA, Isringhausen KT, Bonwell, PB. Interprofessional education: the inclusion of dental hygiene in health care within the United States - a call to action. Adv Med Educ Pract. 2013;2013 Oct 30;4:227-9.
37. American Dental Hygienists' Association. DHA: direct access map [Internet]. Chicago: American Dental Hygienists' Association; 2018 [cited 2019 May 20] Available from: https://www.adha.org/resources-docs/7524_Current_Direct_Access_Map.pdf
38. Stanley JL, Hanson CL, Van Ness CJ, Holt L. Assessing evidence-based practice knowledge, attitudes, access and confidence among dental hygiene educators. J Dent Hyg. 2015 Oct;89(5):321-9.
39. American Dental Hygienists' Association. Policy manual [Internet]. Chicago: American Dental Hygienists' Association; 2018 [cited 2019 Feb 25]. Available from: https://www.adha.org/resources-docs/7614_Policy_Manual.pdf