You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Sleep-related breathing disorders (SRBDs), such as obstructive sleep apnea (OSA) and upper airway resistance syndrome (UARS), are being recognized as major public health concerns because of their increasing prevalence in the general population,1 and OSA-the most severe SRBD-occurs in an estimated 4% of men and 2% of women worldwide.2 The prevalence of these disorders is of particular concern due to their strong association with morbidity from cardiovascular disease,3 type 2 diabetes,4 and depression,5 among other conditions, as well as their effect on mortality.6
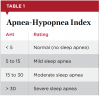
SRBDs are characterized by sleep-disordered breathing that results from the repeated collapse or restriction of the pharyngeal airway during sleep due to structural and functional abnormalities.2 SRBDs are diagnosed through an overnight polysomnogram or a home sleep test and measured using the Apnea-Hypopnea Index (AHI) (Table 1), which associates the number of apneic and hypopneic events per hour with severity.
To promote the wider adoption of regular SRBD screening protocols, this article will focus primarily on the craniofacial anatomic characteristics that can be easily identified or measured during routine dental examinations with patients. To begin, however, it is prudent to discuss two additional risk factors that play a substantial and complementary role in the development of SRBDs.
Age and Obesity
Age and obesity are two primary risk factors that contribute to the development of sleep-disordered breathing. In the United States, the population of Americans aged 65 and older is projected to more than double by the year 2060,7 and nearly 40% of the adult population is obese8; therefore, it stands to reason that the incidence of SRBDs continues to climb to epidemic proportions.
As individuals age, their airways-along with the rest of their bodies-undergo anatomic changes that put them at a higher risk of developing sleep-disordered breathing. These changes include a lengthening of the soft palate, an increase in the size of the pharyngeal fat pads, modifications to the bony structures around the airway, and a diminished response to negative pressure stimulation from the genioglossus muscle. These anatomic changes can contribute to both the narrowing and restriction of the airway and the development of sleep-disordered breathing.
Obesity, which is measured using the body mass index (BMI), exacerbates these airway changes and produces additional structural and functional irregularities that result in apneic events. As a person gains weight, overall corporal fat distribution affects neck and tongue adiposity, creating a narrowed airway and the potential for partial or complete restriction during sleep. Furthermore, increased visceral fat weighs down the stomach and creates a strong tug on the trachea that acts similarly to a "finger trap," causing the airway to become longer, narrower, and more restricted.
Craniofacial Anatomic Risk Factors
Beyond the effects of age and obesity, certain characteristics of the craniofacial anatomy, including neck circumference, lack of cricomental space, a small or recessed chin, an overbite, reduced pharyngeal space, enlarged tonsils, decreased intermolar distance, and a high-vaulted palate, present specific risk factors for the development of sleep-disordered breathing or SRBDs.
Neck Circumference
Neck circumference, which strongly correlates with BMI, is a significant independent risk factor for severe OSA.9 As explained above, increased neck adiposity associated with increased corporal fat deposits in obese or overweight patients creates anatomic changes that inhibit the flow of air through the airway during sleep.
As a general rule, women with a neck circumference of 15.5 in or larger and men with a neck circumference of 17.0 in or larger are at greater risk for developing sleep-disordered breathing and other related disorders.
Conversely, people with smaller-than-normal necks that measure 14 inches or less also tend to have diminished airway room, making them susceptible to breathing abnormalities while sleeping. Although a small neck circumference is much less common than a large neck circumference, both should be considered risk factors when screening for SRBDs.
Lack of Cricomental Space
Known colloquially as a "turkey wattle" or "double chin," a lack of cricomental space is defined by the absence of a curved gap between a patient's chin and throat. Similar to a larger- or smaller-than-normal neck circumference, the presence of excess neck tissue can contribute to the development of sleep-disordered breathing by causing a narrowing of the upper airway. In addition, the weight of the loose neck tissue can contribute to the collapse of the soft airway, especially if the individual habitually sleeps on his or her back.
Identifying a potential lack of cricomental space is easily done through visual assessment. Measurement can also be completed using a ruler or small tape measure. First, while the patient holds his or her head in a neutral position, find the cricomental distance by measuring between the cricoid cartilage and the inner chin. Then, bisect the cricomental distance and measure the perpendicular distance to the skin (Figure 1). If the patient's cricomental space is greater than 1.5 cm, his or her risk of developing an SRBD is very low. If the cricomental space is less than 1.5 cm, then other factors such as increased age, larger- or smaller-than-normal neck circumference, increased weight, overbite, and high pharyngeal grade should also be assessed; the more of these factors that are present, the higher the patient's risk of developing an SRBD.10
Small or Recessed Chin
Many patients with SRBDs have lower-face abnormalities, such as a small or recessed chin, which is also known as retrognathia. Often, a diminutive or receding jaw results in insufficient room for the tongue and decreased room in the upper airway. It may also push the tongue back into the throat cavity. All of these factors can lead to bruxism, snoring, gasping, choking, and abnormal pauses in breathing.
A person is considered to have retrognathia if the lower jaw (ie, mandible) is set further back than the upper jaw (ie, maxilla). These findings may not be obvious in some patients and may require imaging to confirm. However, a receding jaw with 2 mm or more of overbite that results in a prominent mental cleft or curling of the lower lip should be readily discernable during a routine dental examination.11
Overbite
An overbite is sometimes regarded as a purely orthodontic issue, but in addition to the significant impact it may have on a patient's oral health, an overbite can also affect his or her facial structure, speech, and breathing. About two-thirds of Americans have clinically meaningful mandibular incisor irregularity, overjet, and overbite.12 The potential for an overbite to develop increases significantly with age, and the condition is more prevalent among men than women.
In orthodontics, a patient is considered to have an overbite when 50% or 4 mm of the lower incisors are covered when the patient bites down. Another good screening tool to determine a patient's bite is the Shimbashi measurement. The Shimbashi measurement refers to the distance between the cementoenamel junction of the central upper incisors and the cementoenamel junction of the central lower incisors, which should amount to 17 mm to 18 mm.13 Patients with a Shimbashi number that is significantly less than 18 mm are likely to have their lower front teeth nearly completely covered by their upper teeth. Such patients are much more prone to developing sleep-disordered breathing as a result of their uneven bites (Figure 2).
Pharyngeal Grade and Mallampati Classification
For patients in whom OSA or sleep-disordered breathing is suspected, an examination of the soft palate and pharyngeal space is essential in helping to determine their level of risk. Airway obstruction commonly occurs in the portion of the pharynx that lies between the soft palate and the hyoid bone. An elongated soft palate and enlarged uvula may compromise a patient's airway, making it difficult for him or her to breathe at night. In addition, redness on the back of the throat may indicate acid reflux, which is another hallmark of sleep-disordered breathing. Two simple screening tools that can be used to examine the posterior soft tissues include the pharyngeal grading system and the Mallampati classification.
The pharyngeal grading system categorizes the amount of pharyngeal space that is visible or obscured by the tissues in the back of the throat using the following classes14 (Figure 3):
Class I. Palatopharyngeal arch intersects at the edge of the tongue.
Class II. Palatopharyngeal arch intersects at 25% or more of the tongue diameter.
Class III. Palatopharyngeal arch intersects at 50% or more of the tongue diameter.
Class IV. Palatopharyngeal arch intersects at 75% or more of the tongue diameter.
Patients with a pharyngeal grade above class II are at an increased risk for developing SRBDs. Those who have a pharyngeal grade of class III or IV, a cricomental distance of less than 1.5 cm, and an overbite have a 95% chance of experiencing apneic events and should be sent to their primary physician for further evaluation and diagnosis.14
The Mallampati scoring system, which refers to how much of the uvula or soft palate that can be seen or is obscured by the tongue when the patient opens his or her mouth, includes the following classes15 (Figure 4):
Class I. The uvula and tonsils (or tonsillar pillars) are visible.
Class II. The uvula is visible, but the tonsils are not.
Class III. The soft palate is visible, but the uvula is not.
Class IV. Only the hard palate is visible.
Enlarged Tonsils
Abnormally large tonsils are generally associated with sleep-disordered breathing in children; however, adults can also suffer from swollen throat glands and adenoids that block the airway and make breathing difficult or almost impossible, especially when coupled with other factors. For example, an adult with large tonsils and a recessed or small chin has a high probability of experiencing sleep-disordered breathing.
A tonsil grading system is the appropriate screening tool to use when determining whether the size of a patient's tonsils is contributing to his or her risk of SRBDs. The Brodsky tonsil grading scale includes the following grades16:
Grade 0. The tonsils have been removed or are located completely within the tonsillar pillars.
Grade 1. The tonsils are barely visible, occupying less than 25% of the pharyngeal space.
Grade 2. The tonsils occupy 25% to 50% of the pharyngeal space.
Grade 3. The tonsils are large and almost touch the uvula, occupying 50% to 75% of the pharyngeal space.
Grade 4. The tonsils are extremely large, occupying more than 75% of the pharyngeal space.
Patients with a tonsil grade of 3 or 4, whose tonsils protrude past the posterior pillars (Figure 5) or are so large that they are almost vaulted in the middle, are at the greatest risk for the development of sleep-disordered breathing.
Intermolar Distance and Vaulted Palate
Decreased intermolar distance and a high-vaulted palate can also play an important role in the pathophysiology of sleep-disordered breathing and OSA.17 Patients with unusually small intermolar distance or a high-vaulted palate that appears to arch up into the nasal cavity will naturally have less room to accommodate nasal breathing. This is concerning because excessive mouth breathing can cause a high-vaulted palate to become more severe and may ultimately lead to the development of an SRBD.
In order to identify decreased intermolar distance and a high-vaulted palate, dental professionals may look at several intraoral measurements, such as the length, width, height, and arch angle of the roof of the mouth.
Discussion
As healthcare professionals, dental professionals are keenly aware of the importance of detecting the risk for and/or onset of conditions before they result in grave or irreversible consequences. With the increasing prevalence of SRBDs in the general population, dental professionals have a responsibility to assume a greater role in proactively identifying risk factors for these conditions and discussing them with their patients. There are several craniofacial anatomic characteristics, such as those discussed in this article, that can easily be identified during routine examinations without the need for specialized technology or equipment. By being mindful of craniofacial predispositions, general dental professionals can act as the first line of defense against SRBDs and lead the charge in educating patients about the risk factors, symptoms, and comorbidities.
About the Author
Kent Smith, DDS
Diplomate
American Board of Dental Sleep Medicine
President
American Sleep and Breathing Academy
Private Practice
Dallas, Texas
References
1. Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3(4):310-318.
2. Sutherland K, Lee RW, Cistulli PA. Obesity and craniofacial structure as risk factors for obstructive sleep apnoea: impact of ethnicity. Respirology. 2012;17(2):213-222.
3. Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163(1):19-25.
4. Pamidi S, Tasali E. Obstructive sleep apnea and type 2 diabetes: is there a link? Front Neurol. 2012;3:126.
5. Shoib S, Malik JA, Masoodi S. Depression as a manifestation of obstructive sleep apnea. J Neurosci Rural Pract. 2017;8(3):346-351.
6. Pack AI, Platt AB, Pien GW. Does untreated obstructive sleep apnea lead to death? A commentary on Young et al. Sleep 2008;31:1071-8 and Marshall et al. Sleep 2008;31:1079-85. Sleep. 2008;31(8):1067-1068.
7. Mather M, Jacobsen LA, Pollard KM. Population bulletin: aging in the United States. Population Reference Bureau web site. https://assets.prb.org/pdf16/aging-us-population-bulletin.pdf. Published December 2015. Accessed August 21, 2019.
8. Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief. 2017;(288):1-8.
9. Ahbab S, Ataoğlu HE, Tuna M. Neck circumference, metabolic syndrome and obstructive sleep apnea; evaluation of possible linkage. Med Sci Monit. 2013;19:111-117.
10. Persaud N. APNEIC: an easy-to-use screening tool for obstructive sleep apnea. Can Fam Physician. 2010;56(9):904-905.
11. Victor LD. Obstructive sleep apnea. Am Fam Physician. 1999;60(8):2279-2286.
12. Asiri SN, Tadlock LP, Buschang PH. The prevalence of clinically meaningful malocclusion among US adults. Orthod Craniofac Res. 2019. doi: 10.1111/ocr.12328.
13. Sierpinska T, Kuc J, Golebiewska M. Morphological and functional parameters in patients with tooth wear before and after treatment. Open Dent J. 2013;7:55-61.
14. Tsai WH, Remmers JE, Brant R, et al. A decision rule for diagnostic testing in obstructive sleep apnea. Am J Respir Crit Care Med. 2003;167(10):1427-1432.
15. Kanwar MS, Jha RS. Importance of Mallampati score as an independent predictor of obstructive sleep apnea. Eur Respir J. 2012;40(Suppl 56):P3183.
16. Cahali MD, Soares CF, Dantas DA, et al. Tonsil volume, tonsil grade and obstructive sleep apnea: is there any meaningful correlation? Clinics (Sao Paulo). 2011;66(8):1347-1351.
17. Ashok N, Varma NK, Ajith VV, et al. Effect of rapid maxillary expansion on sleep characteristics in children. Contemp Clin Dent. 2014;5(4):489-494.