You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Health care services, including dental hygiene care, should be delivered impartially, regardless of race, age or cultural differences. A 2017 report from the National Healthcare Quality and Disparities Agency showed that African Americans, Asians, Pacific Islanders and Hispanics continue to receive poorer health care than Whites.1 The report also suggests that implicit or unconscious bias, a type of racism and stereotyping, contributes to health care delivery disparities in the United States.1 Unconscious biases may operate unintentionally and may be activated quickly and unknowingly by situational cues such as a person's skin color or accent.2,3 Because implicit bias may operate without a person's intent or awareness, controlling it is often difficult.2-4 Many health care professionals may not be aware of their own racist attitudes or stereotyping which may play a role in the impartial delivery of care.5-13
The percentage of racial minorities in America is projected to increase to approximately 50% of the population by the year 2050.5 Further estimates, depending on geographic location or type of practice, suggest that in some urban settings, 84% of caregiver/patient pairings will likely be in cross-racial/cross-cultural dyads.6 Multicultural competence is necessary to provide effective oral health care to increasingly diverse patient populations. The importance of this competence is underscored by Standard 2-15 of the Commission on Dental Accreditation (CODA) Standards for Dental Hygiene Education Programs that requires graduates to be competent in delivering safe and effective provision of oral health care to diverse populations.7,8
Multifactorial racial and ethnic disparities in health care delivery have been well documented.15-19 The need for culturally competent health care delivery systems, including oral health care, has become more critical in light of the future population shift. Cultural competence has been defined as the ability of systems to provide care to patients with diverse values, beliefs and behaviors, including tailoring delivery to meet patients' social, cultural and linguistic needs.14 Diverse cultural beliefs and norms may impact a patient's recognition of signs and symptoms of disease, thresholds for seeking care, preferences for diagnostic and therapeutic procedures and adherence to treatment recommendations.15-19 Language differences can present a significant barrier to the provision of effective health care.15-19 Trust between the provider and patient may suffer without proper communication. Variations in beliefs and norms may be a barrier to the provision of care and ultimately contribute to health disparities.20-23
The United States (U.S.) Surgeon General's Report on Oral Health in America identified race and ethnicity as playing a major role in lack of access to oral health care.24 Following the report, the Department of Health and Human Services (HHS) established action plans to identify racial and ethnic health disparities and develop cultural competence models to improve the delivery of care to these populations. Improving access to oral health care remains a top priority for HHS as identified in the Healthy People 2020 documents depicting an oral health environment that meets the needs of all people.25,26
One aspect of cultural competence requiring further exploration involves the concept of color-blind racial attitudes.9 A color-blind attitude refers to an individual's denial of the social significance of race and the dismissal or depreciation of the existence of racism and its impact on equality.10,11 Individuals exhibiting color-blindness claim a belief that everyone has equal opportunities, preventing them from seeing the historical causes of racial inequality and its persistence in contemporary society. Multiple research studies have indicated that color-blindness is negatively correlated with multicultural knowledge and awareness.9,11-13,27-30
Health care research studies suggest the quality of care in the U.S. varies according to race and ethnicity, with Hispanic and African American populations receiving lower quality health care than the White population.30,31,34,39 Results from a study conducted by Green et al found that while health care providers might not display outright racism, their decisions on prescribing medical treatment to minorities may be unconsciously affected by inherent racial biases.30 Cooper et al examined attitudes and stereotypes about the race of physicians in regard to medical visit communication and patient ratings of care and found more racial bias was associated with Black patients in the form of more clinical verbal dominance, lower patient positive affect, and poorer ratings of interpersonal care.31 Blair et al also explored whether clinicians' explicit and implicit biases were related to Black and Latino patients' perceptions of their care and found clinicians with greater implicit bias were rated lower in patient-centered care by their Black patients as compared to White patients.33 Implicit racial attitudes were even shown to impact patient communication during genetic counseling. Shaa et al found genetic counselors with stronger pro-White bias used less emotionally responsive communication when counseling minority clients.35
Color-blind racial attitudes have been researched in the psychological sciences as well as dental education.9,11,36-40 Chao et al assessed the multicultural competence (MCC) and color-blind racial attitudes of school counselors and identified that both White and racial/ethnic minority school counselors had the lowest MCC scores and highest color-blind attitudes when they had limited cultural competency training.12 The findings suggest a further need for research and professional development related to color-blind attitudes and cultural competency. Burkard et al found psychologists with high levels of color-blindness had significantly less empathy for their African American clients' conditions/situations compared to European American clients. In addition, psychologists who were less color-blind and were willing to acknowledge that race matters in people's lives showed more empathy than those who were more color-blind.27 Bray et al found that postgraduate counseling students who believed individuals were responsible for their own poverty had lower multicultural competence and higher color-blind racial attitudes, suggesting an inability of the students to relate to clients and their disparities.28 In dentistry, Su et al explored color-blind racial attitudes among dental students and faculty using the color-blind racial attitudes scale (CoBRAS) to determine a baseline.9 Results demonstrated faculty and students possessed moderate levels of color-blind racial attitudes.9 Behar-Horenstein et al examined the impact of curriculum interventions on student outcomes associated with ethical sensitivity, stereotypes, cultural competence and color-blindness. Results on the CoBRAS were similar to Su et al, with students possessing moderate levels of color-blind racial attitudes,41 suggesting the need for increased opportunities to assess the role of these beliefs and their potential impact on oral health care.
There is a gap in the literature regarding the color-blind racial attitudes found in dental hygiene students. Awareness of implicit biases, including a color-blind ideology, found within the dental hygiene student population may assist educators in addressing these concerns early in the curriculum. Moreover, awareness of implicit biases found with dental hygiene faculty members may be an important factor in the unbiased cultural education of future oral health care providers. The purpose of this pilot study was to investigate color-blind racial attitudes in a dental hygiene student population and identify whether dental hygiene students were aware of inherent biases and their potential impact on oral health disparities.
Methods
This cross-sectional study was approved by the Old Dominion University Institutional Review Board. Forty-one first and thirty second-year dental hygiene students in the entry-level, baccalaureate degree dental hygiene program at Old Dominion University, in Norfolk, Virginia, received an email invitation to participate in the voluntary, online survey. Informed consent was implied with the completion of the survey as detailed in the invitation and survey instructions. Qualtrics survey software (Provo, Utah) was used to deliver the survey; either a computer or mobile device could be used to complete the questionnaire.
Survey instrument
The Color-Blind Racial Attitudes Scale (CoBRAS), a validated and reliable survey instrument for measuring contemporary racial attitudes and stereotyping developed by Neville et al,10 was used with permission for the study. CoBRAS is a 20-item instrument scored on a six-point Likert scale with higher scores signifying unawareness of how racial attitudes influence social justice and beliefs that an individual's status is due to merit, not discrimination or bias.10 Contemporary racial attitudes and stereotyping are measured in three subcategories: Unawareness of Racial Privilege, Institutional Discrimination, and Blatant Racial Issues. Scoring the CoBRAS instrument is based on total scores ranging from 20 to 120 along with overall scores for each sub-scale; higher scores indicate a respondent's higher level of unawareness of denial of racism. Overall scores ranging from 20-53.3 indicate low unawareness, 53.4-83.7 moderate unawareness and 83.8-120 high unawareness. Additionally, CoBRAS measures racial attitudes and stereotyping on three subscales: unawareness of White racial privilege (7 items), unawareness of institutional racism (7 items), and unawareness of blatant racial issues (6 items). Scoring for the subscales range from 7 to 42 with 7-18.6 indicating low unawareness, 18.7-30.3 moderate unawareness and 30.4-42 high unawareness.
Participants used a 6-point Likert scale ranging from strongly disagree (1) to strongly agree (6) to determine their level of agreement with the survey statements. Four demographic items were added to the instrument pertaining to the respondents' age, gender, race and year in the dental hygiene program.
Descriptive statistics were used to evaluate the means between the groups. ANOVA and t-tests were used to determine statistically significant differences (p>0.05) among the dental hygiene students based on age, race, gender, and year in the program.
Results
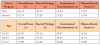
Of the 71 students invited to participate, 70 completed the entire survey (n=70) for a 98.6% response rate. Demographic data revealed that the majority (97%) of respondents were women, 90% were between the ages of 18-29, and 70% were White (Table I). Results revealed an overall average score of 64.89 on the CoBRAS questionnaire. When comparing the first and second-year student groups, there were no statistically significant differences between the student groups for their overall scores (p>0.05). Overall scores and scores broken down by year in the program indicated that the students in general possessed moderate levels of color-blind racial attitudes regardless of their year in the program.
CoBRAS subscales were compared between the first and second-year student groups using t-tests. No statistically significant differences were found between the first and second-year students for the three subscales (p>0.05). Average overall scores and subscale scores of racial privilege, institutional discrimination and blatant racial issues broken down by year in the program and respondent age are displayed in Table II.
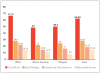
Scores for the subscales of unawareness of White racial privilege, unawareness of institutional racism, and unawareness of blatant racial issues range from 7-42. The average score among both groups of students was 28.86 for the first subscale, indicating moderate levels of unawareness of White racial privilege. Both groups of students had a combined average score of 21.51 for the second subscale, demonstrating moderate levels of unawareness of institutional racism or discrimination. The average scores from the third subscale, unawareness of blatant racial issues, was 14.5 for both groups, indicating low levels of unawareness in this subcategory (Figure 1).
No statistically significant differences were found when comparing the means among the group demographics of age, race, and gender (p>0.05). Mean overall scores broken down by race were White (x=67.25), African American (x=49), Hispanic (x=50.5), and Asian (x=62.83). These scores indicate that both White and Asian student groups had moderate levels of overall unawareness of denial of racism as compared to low levels in African American and Hispanic student groups. White and Asian student groups scored highest on all three subscales when compared to African American and Hispanic student groups, although the small number of participants in these subgroups limit validity of these findings (Figure 2).
Discussion
Research suggests implicit bias and color-blind racial attitudes impact clinician competency and the delivery of health care.13,27-39 In contrast to overt racism, which implies racial superiority and social inequality, color-blind attitudes represent denial about the existence of racism. High levels of color-blind beliefs and pro-White ideals may ultimately impact patient communication and the quality of patient care.9,12,27,29 Dental hygienists will encounter diverse populations in increasing numbers as the landscape of the American population continues to diversify.5,7,8 Therefore, they must be prepared to effectively work with this diversity in patients. Results of the CoBRAS questionnaire indicate moderate levels of denial of racism among the dental hygiene students surveyed in this study. Overall mean scores and the average scores for two of the subscales (unawareness of White racial privilege and unawareness of institutional dis- crimination) indicate moderate levels of unawareness among the participants. However, it is noteworthy that the third scale, measuring awareness of blatant racial issues, had an average score in the low range. These results suggest that participants were more aware of overtly obvious acts of racism rather than inherent biases associated with White privilege and institutional discrimination. Findings from this study are similar to the research Su et al and Behar-Horenstein et al conducted among dental students, with overall moderate levels of unawareness and low scores in the subcategory of blatant racial issues.9,41
In this study nearly three-quarters of participants identified as White. Ancis et al studied student perceptions of campus climate by race and found that White students experienced less racial biases and lacked a recognition that interracial conflicts even existed among students of differing races.43 White students were described as being immune from hostile climates associated with racial tension and conflict.43 This concept could explain the findings of moderate levels of unawareness related to racial privilege and institutional discrimination among these White dental hygiene student respondents.
Participants demonstrated moderate levels of unawareness on the first subscale assessing White privilege, indicating that most of the student participants were unaware of the advantages White people hold in society.44 This finding is of concern as it can influence the delivery of care from these future oral health professionals. It has been well documented in literature that there are disparities in overall health care due to race, and these social determinants are also applicable to oral health care.39,45-47 Dudzinki addressed White privilege and its implications on bioethics in health care and stressed the importance of health care faculty members to openly discuss implicit biases with students and create discussion on how racial bias is a factor in the delivery of clinical care.48 These same teaching principles could also be applied in the dental hygiene curriculum.
The second CoBRAS subscale addressed unawareness of institutional racism. This type of racism has been described as operating at a societal level;49 the structures, policies, practices and norms resulting in differential access to goods, services and opportunities of society by race.50 Both respondent groups scored moderately on this subscale, indicating a lack of recognition regarding the ways Institutional racism can result in differential access to health services, resulting in poorer well-being for ethnic minorities.50-53 Because oral health care services may be impacted by institutional racism, dental professionals should be aware of these societal biases and their potential impact on oral health care. In addition, dental hygiene students themselves can be negatively affected by institutional discrimination.52
The final subscale, blatant racism, in contrast to color-blind racial attitudes, is racism conducted in a more obvious and offensive manner. Within this subscale the CoBRAS survey includes the statement, "Racial problems in the U.S. are rare, isolated situations," which is indicative of overt racism. Respondents' average scores for this subscale were low, indicating awareness of such racial issues and their impact on society. The lower scores could be attributed to wording of the statement and its explicitness related to racism, rather than inherent bias. Subscale results from this study were similar to those found among dental students.9,41
Incorporating curricular interventions aimed at reducing health disparities due to race and ethnicity, including color-blind ideology and awareness of cultural bias, are important in fostering cultural competence in dental hygiene students. Training modules and workshops incorporated into dental hygiene curriculum and development of continuing education courses on colorblindness may help dental hygienists recognize color-blind racial attitudes and unconscious bias. The color-blind racial attitudes scale (CoBRAS) may be an excellent tool for faculty and students as well as practitioners to determine their personal levels of inherent bias. Dental hygiene educators could consider using this tool to bring awareness to these issues and provide interventions early in dental hygiene students' education. Fostering strategies that promote cultural competence via an understanding of color-blind racial ideology might improve culturally sensitive communication and play an important role in addressing oral health disparities.
This pilot study had several limitations. The convenience sample included dental hygiene students from a single program, located in the Mid-Atlantic region of the U.S., limiting the generalization of the results. The lack of ethnic and racial diversity among the participants is also a limiting factor. Also, the majority of students fell into the age range of 18-29 which may have influenced the results based on the number of experiences they may have had with racial tension and conflict.43 A larger sample size using students and practicing clinicians from various locations throughout the United States may demonstrate significant differences among the various groups. Further research is needed with a larger sample size from more varied geographic locations, representing a broader population with greater variation in age, gender, ethnicity.
Conclusion
Results from this pilot study suggest dental hygiene student participants were unaware of their inherent biases as measured by the Color-Blind Racial Attitudes Scale; denial of the existence of racism was common in participants. Participants, regardless of their year in the dental hygiene program, were moderately unaware of the advantages of White racial privilege and institutional discrimination. Findings underscore the need for more research to better understand colorblind ideology in dental hygienists as well as how color-blind racial attitudes affect multicultural competence in dental hygiene students. Further research with a larger and more diverse pool of participants is recommended to enhance understanding of the role of color-blind attitudes in dental hygienists and improved delivery of oral care to diverse populations.
About the Authors
Emily A. Ludwig, RDH, MSDH is a lecturer; Jessica R. Suedbeck, RDH, MSDH is an assistant professor; Susan L. Tolle, RDH, MS is a professor; all in the Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University, Norfolk, VA.
Corresponding author: Emily A Ludwig, RDH, MSDH; eludw003@odu.edu
References
1. Agency for Healthcare Research and Quality. 2017 National health care quality and disparities report. [Internet]. Rockville, MD: Agency for Healthcare Research and Quality. 2017 Nov [cited 2019 Jan 31]. Available from: https://www.ahrq.gov/research/findings/nhqrdr/nhqdr17/index.html.
2. Blair IV, Banaji MR. Automatic and controlled components. J Pers Soc Psychol. 1996 Jan;70(6):1142-63.
3. Devine PG. Stereotypes and prejudice: their automatic and controlled components. J Pers Soc Psychol. 1989 Jan;56(1):5-18.
4. Fazio RH, Jackson JR, Dunton BC, Williams CJ. Variability in automatic activation as an unobtrusive measure of racial attitudes: A bona fide pipeline? J Pers Soc Psychol.1995 Dec;69(6):1012-7
5. U.S Census Bureau. Quick Facts Table. [Internet]. Washington, DC: U.S. Department of Commerce; 2017 Jul [cited 2019 Jan 31]. Available from: https://www.census.gov/quickfacts/fact/table/US/PST045217.
6. Constantine MG. Predictors of satisfaction with counseling: racial and ethnic minority clients' attitudes toward counseling and ratings of their counselors' general multicultural counseling competence. J Couns Psychol. 2002 Apr;49(2):255-63.
7. Commission on Dental Accreditation. Accreditation standards for dental hygiene education programs [Internet]. Chicago, IL: American Dental Association; 2018 Feb [cited 2019 Feb 2]. Available from: https://www.ada.org/~/media/CODA/Files/dental_hygiene_standards.pdf?la=en.
8. Commission on Dental Accreditation. Accreditation standards for dental education programs [Internet]. Chicago, IL: American Dental Association; 2016 [cited 2019 Feb 2]. Available from: https://www.ada.org/~/media/CODA/Files/Advanced_Education_General_Dentistry_Standards.pdf?la=en.
9. Su Y, Behar-Horenstien LS. Color-blind racial beliefs among dental students and faculty. J Dent Educ. 2017 Sep;81(9):1098-1107.
10. Neville H, Lilly R, Duran G, et al. Construction and initial validation of the color-blind racial attitudes scale (CoBRAS). J Couns Psychol 2000 Jan;47:59-70.
11. Neville H. Exploring the association between color-blind racial ideology and multicultural counseling competencies. Cultur Divers Ethnic Minor Psychol. 2006 Apr;12(2):275-90.
12. Chao RC. Race/ethnicity and multicultural competence among school counselors: Multicultural training, racial/ethnic identity, and color-blind racial attitudes. J Couns Dev. 2013 Apr;91(2):140-51.
13. Katz AD, Hoyt WT. The influence of multicultural counseling competencies and Anti-Black prejudice on therapists' outcome expectancies. J Couns Psychol. 2014 Apr;61(2):299-305.
14. Betancourt JR, Green AR, Carrillo JE, Ananeh- Firempong II O. Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health Care. Public Health Rep. 2003 Jul;118(4):293.
15. Meuter RFI, Gallois C, Segalowitz NS, et al. Overcoming language barriers in health care: A protocol for investigating safe and effective communication when patients or clinicians use a second language. BMC Health Serv Res. 2015 Sept;15(1):1-5.
16. Chu C. Cross-cultural health issues in contemporary Australia. Ethn Health. 1998 Feb:3(1-2);125-34.
17. Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited english proficiency? A systematic review of the literature. BCM Health Serv Res. 2007 Apr;42(2):727-54.
18. Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000 Nov;57(3):181.
19. Murray SB, Skull SA. Hurdles to health: immigrant and refugee health care in Australia. Aust Health Rev. 2005 Feb;29(1):25-9.
20. Anderson LM, Scrimshaw SC, Fullilove MT, et al. Culturally competent health care systems. A systematic review. AM J Prev Med. 2003 Apr;24(3):68-9.
21. Betancourt JR, Green AR, Carrillo JE, Park ER. Cultural competence and health care disparities: key perspectives and trends. Health Aff. 2005 Mar;24(2):499-505.
22. Einbinder LC, Schulman KA. The effect of race on the referral process for invasive cardiac procedures. Med Care Res Rev. 2000 Nov;57(3);162.
23. van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians' perceptions of patients. Soc Sci Med. 2000 Mar:50(6):813.
24. U.S. Department of Health and Human Services. Oral Health in America: a report of the Surgeon General. [Internet] Rockville, MD: U.S. Department of Health and Human Services; 2000 Jul [cited 2019 Jan 30]. Available from: https://www.nidcr.nih.gov/research/data-statistics/surgeon-general
25. U.S. Department of Health and Human Services. HHS action plan to reduce racial and ethnic disparities: a nation free of disparities in health and health care. [Internet] Rockville, MD: U.S. Department of Health and Human Services; 2011 Apr [cited 2019 Jan 30]. Available from: http://www.minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf
26. Office of Disease Prevention and Health Promotion. Healthy people 2020 [Internet] Washington, DC: U.S. Department of Health and Human Services; 2013 Mar [cited 2019 Jan 30]. Available from: https://www.healthypeople.gov
27. Bukard AW, Knox S. Effect of therapist color-blindness on empathy and attributions in cross-cultural counseling. J Couns Psychol. 2004 Oct;51(4):387-97.
28. Bray S, Balkin RS. Master's-level students' beliefs concerning the causes of poverty, implicit racial attitudes, and multicultural competence. J Prof Couns. 2013 Jun;40(2):33-44.
29. Gushue GV. Color-blind racial attitudes and white racial identity attitudes in psychology trainees. Prof Psychol Res Pr. 2007 Jun;38(3):321-28.
30. Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007 Apr;22(9):1231-38.
31. Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012 May;102(5):979-87.
32. Penner LA, Dovidio JF, West TV, et al. Aversive racism and medical interactions with Black patients: A field study. J Exp Soc Psychol. 2010 Mar;46(2):436-40.
33. Blair IV, Steiner JF, Fairclough DL, et al. Clinicians' implicit ethnic/racial bias and perceptions of care among Black and Latino patients. Ann Fam Med. 2013 Jan-Feb;11(1):43-52.
34. Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012 May;102(5):979-87.
35. Schaa KL, Roter DL, Biescecker BB, et al. Genetic counselors' implicit racial attitudes and their relationship to communication. Health Psychol. 2015 Feb;34(2):111-9.
36. Blair IV, Havranke EP, Price DW, et al. Assessment of biases against Latinos and African Americans among primary care providers and community members. Am J Public Health. 2013 Jan;103(1):92-8.
37. Schnieder EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in Medicare managed care. JAMA. 2002 Mar; 287:1288-94.
38. Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000 Nov; 9:1156-63.
39. Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. [Internet] Washington, DC: The National Academies Press; 2002 Aug [cited 2019 Jan 30]. Available From: https://cdn.ymaws.com/www.aptrweb.org/resource/collection/0B76BF46-69A2-4560-BF7C-98682BBA60C1/Unequal%20Treatment_IOM%20Report.pdf
40. Stone J, Moskowitz, GB. Non-conscious bias in medical decision making: what can be done to reduce it? Med Educ. 2011 Aug;45(8), 768-76.
41. Behar-Horenstein LS, Garvan C. Relationships among knowledge, efficacy, and practices instrument, color-blind racial attitudes scale, Deamonte Driver survey, and defining issues test 2. J Dent Educ. 2016 Apr;80(3):355-64.
42. Zamudio MM, Rios F. From traditional to liberal racism: living racism in the everyday. Sociol Perspect. 2006 Dec;49(4):483-501.
43. Ancis JR, Sedlacek WE, Mohr J. Student perceptions of campus cultural climate by race. J Couns Dev. 2000 Apr;78(2):180-5.
44. Stewart TL, Latu IM, Branscombe NR, et al. White privilege awareness and efficacy to reduce racial inequality improve White Americans' attitudes toward African Americans. J Soc Issues. 2012 Mar;68(1):11-27.
45. Nelson, A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002 Aug;94(8):666.
46. Hobbs J. White privilege in health care: following recognition with action. Ann Fam Med. 2018 May;16(3):197-8.
47. Ayanian JZ. The costs of racial disparities in health care. N Engl J Med. 2015 Oct;93(10).
48. Dudzinski DM. White privilege and playing it safe. Am J Bioeth. 2018 Jun;18(6):4-5.
49. Cobbinah SS, Lewis J. Racism & health: A public health perspective on racial discrimination. J Eval Clin Pract. 2018 Oct;24(5):995-8.
50. Chaney C. Institutional racism: perspectives on the department of justice's investigation of the Ferguson police department. Western J Black Stud. 2015 Winter; 39(4):312-30.
51. Jones CP. Confronting institutionalized racism. Phylon. 2002 Jan;50(1/2):7‐22.
52. Romano MJ. White privilege in a white coat: how racism shaped my medical education. Ann Fam Med. 2018 May;16(3):261-3.
53. Yearby R. Racial disparities in health status and access to health care: the continuation of inequality in the united states due to structural racism. Am J Econ Soc. 2018 May;77(3-4):1113-52.