You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
Dental radiographs are an essential component of comprehensive oral care, disease management and diagnosis; however, there are risks associated with the ionizing radiation needed to image teeth and the surrounding bone.1 Ionizing radiation emitted to produce dental radiographs contains enough energy and has the potential to form unstable atoms and damage DNA;2,3 therefore, the As Low As Reasonably Achievable (ALARA) principle was developed to promote awareness and minimization of radiation exposure.1,4-8 Long-term effects of low doses of radiation over time are not well known, but may be associated with embryological defects, low birth-weight babies, cataracts, genetic mutations, salivary gland tumors, and thyroid cancer; thus, making it increasingly important to keep all radiation exposure as low as possible.2-4 ALARA is supported by numerous radiation control and safety professional organizations, including the American Dental Association (ADA), the National Council on Radiation Protection and Measurements (NCRP), and the International Commission on Radiological Protection (ICRP), and is recommended for adoption and implementation by dental professionals.2,4,8
Patient selection
The ADA has provided selection criteria for prescribing and establishing appropriate intervals for dental radiographs as well as the various types of radiographs based on individual needs, giving dental professionals recommendations for application of the ALARA principle.8,9 ADA selection criteria guidelines recommend the use of assessment findings to determine the appropriate radiographic images based on the individual's disease state, risk factors, age, current patient status (new or recall), medical and dental histories, and findings from the comprehensive clinical examination.7-8 Examples of clinical findings used include periodontal involvement and loss of clinical attachment in addition to caries risk status. Periodontal involvement is an important criterion to determine the need for radiographs as the incidence of periodontal disease increases with age.10 Patients may not always exhibit active periodontal disease clinically; however, selected periapical images (PA's) may determine the extent and prognosis of the disease through radiographic bone level present and the widening of the periodontal ligament space.8
Radiation safety
ADA radiographic selection criteria guidelines recommend use of digital image receptors with the ability to limit radiation exposure.6,8 Study results by Berkhout et al. identified up to 55% reduction in radiation exposure when comparing digital imaging to E-speed films.11 Direct digital image receptors (wired sensors) may be considered more ideal in terms of radiation safety as they have a narrower dynamic range as compared to the wider range of photostimulable phosphor (PSP) plates.11-14 It is important to maintain a goal of producing diagnostic radiographs while decreasing patient and clinician exposure to ionizing radiation.
Other safety measures to reduce radiation exposure include equipment factors, such as the shape and length of the position indicating device (PID) on the x-ray tubehead. Rectangular PIDs minimize radiation exposure compared to round; longer PIDs reduce radiation compared to short PIDs.6,8,15 Due to the potential of scatter radiation exposure for dental professionals, all safety measures should be taken to minimize operator radiation exposure.16 Defective x-ray machines may result in drifting of the PID, increasing the need for retakes. Additionally, x-ray equipment must be checked periodically to ensure proper functioning as required by state and federal law.6 Operators should never hold the x-ray unit or have their hand in the path of the primary x-ray beam during an exposure.15
Key safety features also include exposure factors such as: milliamperage (mA), exposure time, and kilovoltage (kV) settings. These exposure factors should be modified depending on varying bone densities within the oral cavity. Higher exposure settings are needed to image areas with greater bone density, while lower exposure settings image less dense areas.17 When exposing pediatric patients to radiation, it is important to consider that bone structures of children under twelve years old are typically less dense than those of adults;8 therefore, exposure times should be reduced by approximately 30%.18 Children may also be more susceptible to radiation injury compared to adults because of their younger, more rapidly dividing cells.7,19 If variable exposure settings for kVp and mA are available on the unit, the dental professional should ensure that the appropriate settings are used based on patient size and area of the oral cavity being exposed. In the absence of variable kVp and mA settings, exposure time may need to be adjusted to compensate for patient size and the area being irradiated.
Lead or lead equivalent aprons are also important safety measures as they protect the patient from scatter radiation that might impact critical organs and tissues. A thyroid collar should be provided in addition to lead aprons for thyroid gland protection and should be used for all children, women of childbearing age, and pregnant women.7,8,15-16,20-21 Thyroid collars have been shown to reduce exposure up to 33% in children and 63% in adults.22-23 The National Council on Radiation Protection and Measurements (NCRPM) states that the patient lead or lead equivalent aprons are not required when all the following safety measures are adhered to: use of rectangular collimation, fast image receptors, and patient selection criteria guidelines.24 Furthermore, the NCRPM states that thyroid collars should be used on all patient exposures except when there is potential of interfering with the examination, which most commonly occurs during the exposure of a panoramic image.21,24
Radiographs during pregnancy
Controversy exists on risks versus benefits associated with exposure of dental radiographs on pregnant women. Current ADA guidelines reference the American College of Obstetricians and Gynecologists (ACOG) in expressing that exposing pregnant patients to necessary dental radiographs during any stage of pregnancy is considered to be safe as long as abdominal and thyroid shielding are used.25 ADA selection criteria guidelines should be referenced and used for determining the type of radiographs for the identified condition and whether dental x-rays are necessary and beneficial for the recommended treatment. Dental professionals should also use digital imaging and fast image receptors to further reduce exposure to radiation in pregnant patients. According to Matteson et al., there is no evidence to support excluding x-rays due to pregnancy;26 however, no studies have been conducted due to safety issues in testing pregnant patients.
Radiographic techniques and handheld devices
Proper radiographic technique is also important in reducing radiation to eliminate retake exposures.20 The paralleling technique should be attempted first, as it is considered the gold standard for acquiring periapical images while reducing radiation exposure.20,24 An alternative approach, the bisecting angle technique, may result in image distortion and increased radiation exposure of the thyroid gland and lens of the eye due to the increased vertical angulation of the tubehead.20,27 To prevent retakes, clinicians should decide on the most ideal technique based on the patient's unique characteristics.
Handheld radiographic devices, such as the NOMAD™ and Nomad Pro 2™ (KavoKerr; Charlotte, NC, USA), are frequently being found in traditional as well as alternative practice settings due to their ease of use and portability.28 These handheld devices are often used when a wall-mounted x-ray machine is not available such as nursing or private home settings or when the patient cannot be moved.29 Practitioners should ensure that the handheld device has been certified by the Food and Drug Administration (FDA) and that all the manufacturer safety precautions are being followed.30 FDA compliance inspections must be performed on all dental x-ray machines within one year of purchase.30 Safety requirements include inherent tubehead shielding, additional shielding around the PID, and a leaded acrylic external backscatter ring shield.31 In general, scatter radiation is reduced with handheld radiographic devices because a smaller area is exposed to radiation; however, the backscatter ring shield must also be affixed to the device for optimal operator protection.8
Manufacturers of the NOMAD™ handheld radiographic devices advise specific instructions in regard to optimal operator protection from backscatter radiation exposure. Operators must stand within the significant zone of occupancy immediately behind the device shield, ensure the backscatter ring shield is placed at the outer end of the PID, and keep the PID as close to the patient's face as possible.8,31 Radiation protection is considered to be minimized when the device is not held at mid-torso, with the PID parallel to the floor;31 any operation outside of the protection zone could result in backscatter radiation exposure.31 Protective thyroid collars and lead aprons are recommended for clinicians when operating handheld radiographic devices.8,31,32
Regular training is important for ongoing reinforcement of radiation safety practices.8 In general, research suggests that up to 44% of knowledge is lost within six to twelve months after information has been learned;34 therefore, clinicians may benefit from review of the safety standards and advancements in radiation practice. Little is known about the radiation safety behaviors of dental hygienists. The purpose of this study was to determine the radiation safety methods currently being implemented by practicing dental hygienists in the United States (U.S.).
Methods
The Institutional Review Board of Old Dominion University granted approval for this investigator-designed survey that utilized a convenience sample of dental hygienists in the U.S. who were subscribers of an online professional journal (Dimensions of Dental Hygiene, Belmont Publications, Santa Ana, CA). An invitation to participate in the survey was emailed by the publisher to the first 1,500 subscribers; Qualtrics (Provo, Utah) administered the online survey. A cover letter was included with the survey explaining the purpose, instructions for survey completion, inclusion/exclusion criteria, and references to contact for questions; survey submission was acknowledged as consent to participate. Inclusion criteria consisted of dental hygienists currently practicing in the U.S. who exposed radiographs. Prior to beginning the study, the survey was pilot-tested for content and validity on 29 dental hygiene faculty members at Old Dominion University.
The survey contained six close-ended demographic questions related to education, number of semesters devoted to radiology curriculum, primary work setting, age, years of experience, and location of current practice. The remaining sixteen questions included use of ADA selection criteria guidelines, policies implemented by practice settings, and use of handheld radiographic devices. Questions regarding the ADA selection criteria guidelines and image receptor use had responses of yes or no for each question item. Respondents answered items regarding their current radiographic technique with a 7-point Likert scale with choices ranging from strongly agree to strongly disagree. Respondents were asked to answer yes or no on whether they ever held the PID in place during an exposure. Those who said yes were asked to provide how many times they did so in the last 10 years and an explanation of the listed situations. Questions regarding the use of a handheld radiographic device were presented as yes or no questions. Respondents were asked to explain whether they aimed the handheld device at their mid-torso level for all exposures. Questions describing individual practice policies were presented in short answer format.
The survey was made available for forty-seven days. Non-respondents were sent email reminders every two weeks. Responses were reported and analyzed in group format to preserve respondents' identities. Statistical analysis was performed using Statistical Analysis Software (SAS®; Cary, NC) version 9.4.35 Data were analyzed for distribution differences and statistical significance using descriptive statistics, logistic regression models, and general linear models.
Results
A total of 566 dental hygienists (n=566) met the inclusion criteria for a response rate of 38%. Over one-third (38%) of the respondents had been practicing dental hygiene for 31 or more years. Sample demographics are shown in Table I. A majority of respondents reported always using a patient lead apron (89%) and including thyroid collars for intraoral exposures (78%). Nearly three-quarters of the respondents (72%) indicated using short PIDs for radiographic procedures and only 4% of respondents reported using a rectangular PID. Respondents reported using the following types of image receptors: film (7%), E speed film (6%), F speed film (7%), PSP plate (24%), and direct digital image receptor (79%). Over half of the respondents (52%) admitted to holding the PID in place during an exposure. Selected explanations of situations for holding the PID in place are shown in Table II.
Regarding radiographic imaging techniques, 61% of the respondents reported they somewhat agreed to strongly agreed to using the bisecting angle technique as the first choice for obtaining periapical images (61%), while 56% reported they somewhat agreed to strongly agreed to using the paralleling technique first. The vast majority of respondents knew that exposure settings should be changed for pediatric patients (90%), and three-fourths believed settings should be altered depending on the area imaged (Table III).
Respondents provided information regarding their practice policies on the radiographic exposure of pregnant patients. Ten respondents reported their practice does not see pregnant patients and were excluded from the statistical analysis. Of the remaining respondents (n=556), 14% had practice policies prohibiting exposure of radiographs during pregnancy, while 50% exposed radiographs on pregnant patients only in cases of pain or emergency. Twelve percent of respondents reported their practice took dental radiographs depending on the patient's trimester, and 8% required written permission from the patient's obstetrician. Two respondents indicated that while they knew that radiographs were safe to take on pregnant patients provided ALARA principles were followed, their supervising dentist did not allow for the radiographs to be taken.
Regarding the use of handheld radiographic devices, 12% (n=67) of respondents indicated using a portable device with 57% reporting that they had received training prior to exposing patients. Respondents reported the following safety measures: kept the PID as close to the patient's face as possible (92%), used an external shield on the device's PID (92%), wore a dosimeter badge (22%), and wore a clinician lead apron (21%). Less than half (38%) of the users reported holding the device at mid-torso level for all exposures.
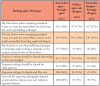
Level of education and the criteria used to determine radiographic need were analyzed and statistically significant relationships in the criteria used to determine need for radiographs based on years of experience were found (p=0.0340). Further analysis identified a statistically significant relationship between a higher level of education (bachelor's degree or higher) and the use of periodontal involvement in particular as a criterion for determining radiographic needs (p=0.0462). Criteria used to determine the need for radiographs and level of education are shown in Table IV.
Safe radiographic techniques and level of education were also analyzed (Table V). Data revealed a significant relationship (p=0.0080) between level of education and radiographic technique used, suggesting clinicians with a bachelor's degree or higher were more likely to use safer techniques as compared to those holding associate's degrees. Statistically significant relationships were found between level of education and the utilization of the paralleling technique as the first choice over the bisecting angle technique (p=0.0052), altering exposure settings depending on the area imaged (p=0.0065), and reducing exposure settings for pediatric patients (p=0.0347).
Forty-one percent of the respondents indicated that they had not completed any continuing education (CE) in dental radiation safety in the last five years, while 34% had taken one course and 25% had taken two or more courses. Frequency of CE courses was analyzed with the PID characteristics used by the respondents. Rectangular PIDs were used more frequently by respondents who had participated in CE courses over the past five years (p=0.0008). Use of clinician lead aprons while using handheld radiographic devices was also shown to be significantly higher based on the number of radiation CE courses taken in the last five years (p=0.0093). Results revealed the chances of using a handheld radiographic device were higher with a lower age range; 23% of respondents using portable devices were between 20-24 years of age (p=0.0025).
Discussion
Dental hygienists should be knowledgeable about implementing safe radiation practices for all patients requiring radiographic examinations. Findings from this study indicated that participants practiced safer radiographic techniques with more years of experience along with higher levels of education. Results from the current study may support the need for more continuing education courses in radiographic technique and safety practices in addition to providing areas of content to be addressed.
Equipment factors
A majority of respondents reported using direct digital image receptors, which have a narrower dynamic range than indirect receptors. Direct digital image receptors are also capable of alerting the operator when exposure settings are outside of the narrow range thus requiring more precise exposure settings and less radiation.29 While the majority of respondents used direct digital image receptors, most were not adjusting the settings to reduce the exposure time, suggesting a need for more education on the dynamic range of direct digital receptors.
Eleven percent of participants reported that they were not using a patient lead apron for all radiographic exposures which may be due to meeting all the NCRP requirements including rectangular collimation, fast image receptors, and following the ADA selection criteria guidelines.24 Rectangular collimation and long PIDs are recommended to decrease the area of the primary x-ray beam and increase the distance from the radiation source in order to reduce the area exposed and minimize scatter radiation.8 Results indicated that about one-fourth of respondents did not use thyroid protection during intraoral exposures which is concerning due to the scatter radiation to the thyroid gland that can result when a circular PID is used. Thyroid collars should be used for all intraoral exposures in the absence of rectangular collimation, fast speed receptors and the use of the paralleling technique.21,24
Radiographic techniques
More respondents used the bisecting angle technique as compared to the paralleling technique, suggesting a higher chance of retake exposures as the bisecting angle technique is less precise compared to the paralleling technique.20,24 The bisecting angle technique also directs the beam toward the thyroid when positioning for the maxillary arch. Using the appropriate radiographic technique is key in reducing patient radiation exposure.
Outside of the radiographic technique utilized, the ALARA principle should be followed to minimize radiation exposure. However, more than one-fourth of respondents indicated exposing radiographs based on third party reimbursement. Determination of when to take dental radiographs should be made based on ALARA principles and the patient's current oral condition, not based on the frequency of a third-party payment for the diagnostic procedure.
Just over half of respondents reported holding the PID in place during an exposure; most frequently while exposing radiographs on pediatric patients. In situations where the child is unable to sit still or occlude on the biteblock, parents and guardians should be asked to hold the image receptor for the child rather than the clinician.
Another reason for holding the PID in place was in cases when the tubehead drifted; however, x-ray machines should require immediate inspection if they are unstable or drifting.15 In addition, operators should be familiar with their state board regulations regarding the frequency of required inspections, as they vary per state. For example, dental x-ray machines are required to be inspected every 3 years in Virginia, every 4 years in Texas, and every 5 years in Utah.30,36-37 Inspection of the machine may help prevent drifting of the tubehead.
Handheld radiographic devices
In general, younger respondents reported use of handheld radiographic devices more frequently, which may be associated with technologically driven devices, preferred by younger dental professionals or due to higher numbers working with homebound patients. However, it was of concern that 43% of respondents using handheld radiographic devices had not received training prior to use on patients and less than half of respondents reported holding the device at mid-torso level. Handheld radiographic devices that are not held at mid-torso level, such as when exposing periapical images with increased vertical angulation, can generate scatter radiation beyond the backscatter ring shield creating increased exposure for the operator. Respondents were either unaware of the importance of the mid-torso guideline or they stated that it was not possible to hold the device at this position for all exposures. Operators cited making exceptions to the mid-torso guideline depending on the difficulty of the patient. Modified positioning techniques such as moving the chin up or down, using image receptor holders, and the paralleling technique should be used to minimize radiation exposure to both the patient and the operator. Increasing the vertical angulation for periapical images can help ensure that the operator is within the significant zone of protection from backscatter radiation exposure.
Manufacturer safety guidelines and Danforth et al. concur regarding use of an operator lead apron and thyroid collar if the handheld devices are being operated outside of what is considered to be the protection zone.8,28,31 Respondents in this study reported that they were not following all the recommended safety measures and, in those cases, should be wearing operator lead aprons as a safety precaution. With the use of handheld radiographic devices increasing,31 operators should be required to have proof of training prior to use, similar to the guidelines outlined by the European Academy of Dento Maxillo Facial Radiology.39
Impact of continuing education courses
Results suggest that CE courses in dental radiation safety had a positive impact on the safety of radiation equipment and the use of protective measures, such as use of rectangular PIDs and thyroid collars. While dental hygienists would benefit from CE courses in dental radiation safety; only about half of respondents had taken at least one dental radiation safety CE course over the past five years.
Responses regarding radiation exposure and pregnant patients also demonstrate the need for regular CE and up to date practice policies. The ACOG states pregnant patients may be exposed to dental radiation during any stage of pregnancy as long as a need exists and a lead apron and thyroid collar are used.25 Responses indicated that many dental hygienists were not following ACOG guidelines. Only 1% of all survey respondents were following current recommendations; this small percentage of respondents indicated knowing that radiographs could safely be exposed on pregnant patients as long as the ADA selection criteria guidelines were followed. Half of the respondents were following old recommendations that do not allow for radiographs unless there is an absolute need.38 Regular CE on radiation safety would be beneficial to keep dental professionals up to date on technological advancements and safety regulations within oral radiology.
Limitations
Limitations to the current study include the convenience sample and the relatively low response rate making it difficult to generalize the results. In addition, there were significantly more respondents from the Eastern (45%) than the Central (34%) and Western (21%) regions of the U.S. Radiographic techniques and safety regulations may vary in different regions of the country. The sample demographics may not be a representative cross-section of the dental hygiene U.S. population since a majority of the respondents had been in practice for at least 31 years, and a majority were aged 55 years or older. The number of radiology courses taken while in dental hygiene school may not have had a direct relationship to the level of radiation safety actually taught and may be a limiting factor in the findings of this study. Future studies may examine the specific radiography course requirements to compare the level of radiation safety taught.
Conclusion
Dental hygienists with more years of experience, a higher level of education, and recent CE course work were more likely to follow ADA radiographic examination selection guidelines and use appropriate radiographic techniques to reduce exposure to ionizing radiation. Future studies are needed to determine effective approaches to improving dental radiation safety.
Content for continuing education courses on radiation safety techniques should be developed to address the technological advances in dental radiography.
About the Authors
Kimberly Lintag, RDH, MS is an adjunct assistant professor; Ann M. Bruhn, RDH, MS is an associate professor and the dental hygiene program chair; Susan Lynn Tolle, RDH, MS is a professor; all in the Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University, Norfolk, VA.
Norou Diawara, PhD is an associate professor in the Department of Mathematics and Statistics, Old Dominion University, Norfolk, VA.
Corresponding author: Kimberly Lintag, RDH, MS; kimberlylintag@gmail.com
References
1. American Dental Association Council on Scientific Affairs. The use of dental radiographs: update and recommendations [Internet]. Chicago: American Dental Association; 2006 Sep [cited 2017 Sept 4]. Available from: https://jada.ada.org/article/S0002-8177(14)64322-1/pdf
2. National Council on Radiation Protection and Measurements. Report no.160 Ionizing radiation exposure of the population of the United States. Bethesda: NCRP Publications; 2009. 387 p.
3. Khare P, Nair P, Khare A, et al. The road to radiation protection: a rocky path. J Clin Diag Res. 2014 Dec 5;8(12):1-4.
4. International Commission on Radiological Protection. ICRP publication 55 optimization and decision-making in radiological protection. Elmsford: SAGE Publications Ltd; 1989. 60 p.
5. Hermsen K, Jaeger S, Jaeger M. Radiation safety for the NOMADTM portable x-ray system in a temporary morgue setting. J Forensic Sci. 2008 Jul 4;53(4):917-21.
6. International Commission on Radiological Protection. ICRP publication 33 - protection against ionizing radiation from external sources used in medicine. Elmsford: Pergamon Press; 1982. 69 p.
7. International Commission on Radiological Protection. ICRP publication 34 - protection of the patient in diagnostic radiology. Elmsford: SAGE Publications Ltd; 1983. 84 p.
8. American Dental Association Council on Scientific Affairs. Dental radiographic examinations: recommendations for patient selection and limiting radiation exposure [Internet]. Chicago: American Dental Association; revised 2012 [cited 2016 Oct 12]. 27 p. Available from: https://www.ada.org/~/media/ADA/Member%20Center/FIles/Dental_Radiographic_Examinations_2012.pdf
9. American Dental Association. Oral health topics: x-rays/radiographs [Internet]. Chicago: American Dental Association; revised 2019 Mar 25 [cited 2018 Mar 9]. Available from: https://www.ada.org/en/member-center/oral-health-topics/x-rays.
10. Hugoson A, Sjodin B, Norderyd O. Trends over 30 years, 1973-2003, in the prevalence and severity of periodontal disease. J Clin Periodontol. 2008 May;35(5):405-14.
11. Berkhout W, Beuger D, Sanderink G, Van der Stelt P. The dynamic range of digital radiographic systems: dose reduction or risk of overexposure? Dentomacillofac Radiol. 2004 Jan;33(1):1-5.
12. Bóscolo F, Oliveira A, Almeida S, et al. Clinical study of the sensitivity and dynamic range of three digital systems, e-speed film and digitized film. Braz Dent J. 2001 May;12(3):191-5.
13. Wenzel A, Sobye I, Andersen M, Friendsson T. Dynamic range and contrast perceptibility in intraoral digital receptors (with an English summary). Tandlægebladet. 2007;111:1085-6.
14. Farman A, Farman T. A comparison of 18 different x-ray detectors currently used in dentistry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005 Apr; 99:485-9.
15. Mupparapu M. Radiation protection guidelines for the practicing orthodontist. Am J Orthod Dentofacial Orthop. 2005 Aug;128(2):168-72.
16. International Commission on Radiological Protection. ICRP publication 57 - Radiological protection of the worker in medicine and dentistry. Elmsford: SAGE Publications Ltd; 1990. 83 p.
17. Chugh T, Jain A, Jaiswal R, et al. Bone density and its importance in orthodontics. J Oral Biol Craniofac Res. 2013 May-Aug;3(2):92-7.
18. Carestream Dental. Exposure guidelines [Internet]. Rochester: Carestream Health, Inc; 2014 [cited 2018 Jan 7]. Available from: https://www.carestream.com/en/us/-/media/publicsite/products_and_solutions/dental/pdf/8641_us_exposure_guidelines_sell_sheet-(1).pdf.
19. Image Gently. Image Gently® and digital radiography [Internet]. Reston: Image Gently; 2014 [cited 2017 Oct 24]. Available from: https://www.imagegently.org/Procedures/Digital-Radiography
20. Rinn Corporation. Intraoral radiography with Rinn XCP/XCP-DS instruments [Internet]. York; DENTSPLY International Inc. Revised 2014 Nov [cited 2017 Sept 4]. Available from: https://www.dentsply.com/content/dam/dentsply/pim/manufacturer/Preventive/X_ray/Arms__Rings/Comfortwand/XCP-Intraoral-Radiography-Education-Manual.pdf.
21. Ad Hoc Committee on Pedodontic Radiology. Guideline on prescribing dental radiographs for infants, children, adolescents, and individuals with special health care needs. Pediatr Dent 2012 Sep-Oct;34(5):189-91.
22. Sikorski P, Taylor K. The effectiveness of the thyroid shield in dental radiology. Oral Surg. 1984 Aug;58(2):225-36.
23. Sinnott B, Ron E, Schneider A. Exposing the thyroid to radiation: a review of its current extent, risks, and implications. Endocr Rev. 2010 Oct;31(5):756-73.
24. National Council on Radiation Protection and Measurements. Report no. 145 - radiation protection in dentistry. Bethesda: Elsevier, Inc; 2005. 191 p.
25. American College of Obstetricians and Gynecologists. Oral health care during pregnancy and through the lifespan [Internet]. Washington, DC: American College of Obstetricians and Gynecologists; 2013 Aug [cited 2017 Dec 20];122:417-22. Available from: https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/Oral-Health-Care-During-Pregnancy-and-Through-the-Lifespan?IsMobileSet=false.
26. Matteson SR, Joseph LP, Bottomley W, et al. The report of the panel to develop radiographic selection criteria for dental patients. Gen Dent. 1991 Jul-Aug;39(4):264-70.
27. Praveen B, Shubhasini A, Bhanushree R, et al. Radiation in dental practice: awareness, protection and recommendations. J Contemp Dent Pract. 2013 Jan 1;14(1):143-8.
28. Danforth R, Herschaft E, Leonowich J. Operator exposure to scatter radiation from a portable hand-held dental radiation emitting device (Aribex™NOMAD™) while making 915 intraoral dental radiographs. J Forensic Sci. 2009 Mar;54(2):415-21.
29. Thomson E, Johnson O. Essentials of dental radiography for dental assistants and hygienists. 10th ed. New York: Pearson Education, Inc; 2018. 466 p.
30. Virginia Department of Health. Dental x-ray machines [Internet]. Richmond: Virginia Department of Health; 2018 [cited 2018 Aug 28]. Available from: http://www.vdh.virginia.gov/radiological-health/radiological-health/x-raymachine-program/dental-x-ray-machines/.
31. Aribex. NOMAD Pro 2 - operator manual [Internet]. Charlotte: KaVo Dental; 2018 Sep 25 [cited 2018 Dec 18]. Available from: https://www.kavo.com/en-us/resource-center/aribex-nomad-pro-2-operator-manual.
32. McGiff T, Danforth R, Herschaft E. Maintaining radiation exposures as low as reasonably achievable (ALARA) for dental personnel operating portable hand-held x-ray equipment. Health Phys. 2012 Aug;103(2 Suppl 2):s179-s185.
33. Williamson GF. Strategies for optimal intraoral digital imaging. Part I: intraoral receptors, techniques, and instrumentation. [Internet]. Chesterland, OH: Academy of Dental Therapeutics and Stomatology; 2009 Aug [cited 2018 Jan 7]:1-11. Available from: http://www.integradent.com.au/pdfs/IntraoralRadiography.pdf
34. Absi E, Drage N, Thomas H, et al. Continuing dental education in radiation protection: knowledge retention following a postgraduate course. Eur J Dent Educ. 2011 Aug 1;15(3):189-92.
35. SAS Institute Inc. SAS/ACCESS® 9.4 Interface. Cary: SAS Institute Inc; 2013. 178 p.
36. Texas Department of State Health Services. Inspections of x-ray machines [Internet]. Austin: Texas Department of State Health Services; 2017 Aug 9 [cited 2018 Dec 31]. Available from: https://dshs.texas.gov/radiation/x-ray/inspections.aspx.
37. Utah Department of Environmental Quality. X-ray dose comparisons: x-ray program [Internet]. Salt Lake City: Utah Department of Environmental Quality; 2018 [cited 2018 Dec 31]. Available from: https://deq.utah.gov/legacy/programs/waste-management-radiation-control/radiation/xray/inspections-registrations-fees.htm.
38. Razi T, Bazvand L, Ghojazadeh M. Diagnostic dental radiation risk during pregnancy: awareness among general dentists in Tabriz. J Dent Res Dent Clin Dent Prospect. 2011 Jun 14;5(2):67-70.
39. Berkhout W, Suomalainen A, Brullmann D, et al. Justification and good practice in using handheld portable dental x-ray equipment: a position paper prepared by the European Academy of DentoMaxilloFacial Radiology (EADMFR). Dentomaxillofac Radiol. 2015 Mar 25;44(6):20140343.