You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Interprofessional (IP) collaboration amongst healthcare professionals is an important healthcare practice model. Successful IP collaboration, to a large degree, is dependent upon effective interprofessional education (IPE). Defined as occurring when two or more healthcare professionals from different disciplines learn from, with and about each other, the goal of IPE is to improve the quality of patient care and promote team-based and patient-centered collaborative practice.1 When delivering IP care, team members combine their individual expertise and observations into joint decision making. Individuals may assume patient care leadership roles relevant to their discipline.2 The importance of student engagement in IP learning has been promoted for many years.1-7 Interprofessional care is ultimately a method to improve patient outcomes through coordinated care among a variety of disciplines. When given the opportunity to participate in IPE, student healthcare provider skills may be strengthened and enhanced. Students who learn to appreciate and value working in an interdisciplinary team may be more prepared to collaborate across other disciplines as they engage in future practice settings.1-3
Dental hygiene's involvement in IPE is an important aspect of the IP model. Given the preventive nature of the dental hygiene profession, coupled with oral-systemic links and healthcare provider shortages, dental hygienists should be integral members of IP collaborations. Dental hygienists must be able to communicate effectively when working with other primary care providers in the management of patients with chronic health conditions.7 Contemporary patients often present with complex health concerns and a variety of risk factors that can best be managed with an interdisciplinary approach.3,7 Dental hygiene education standards set by the Commission on Dental Accreditation (CODA) also recognize the need for IPE by requiring graduates to demonstrate competency in communicating and collaborating with other members of the healthcare team in order to support comprehensive patient care.8
While there are clearly benefits to IP healthcare, barriers and challenges to the incorporation of IPE into healthcare programs have been identified in the literature.2,9-12 Logistics of time and scheduling in an already crowded curriculum along with the lack of faculty development are frequently cited as IPE challenges from a variety of disciplines.9-13 In a study of respiratory therapy faculty, the most frequently reported barrier was time, followed by attitudes toward IPE, scheduling and logistics, curriculum requirements and administration.12 Amongst nutrition faculty members, attitudes were identified as the most common barrier followed by curriculum, resources and scheduling. Similar results concerning the perceived barriers in other health care disciplines were found by Dallaghan et al and Hinderer et al.2,4 In dental hygiene, surveys of program directors report a lack of experience with IPE as the most common barrier followed by issues related to schedule coordination and curriculum.14 To address some of the challenges and barriers of IP collaboration, the World Health Organization (WHO) framework has provided strategies and ideals to assist professionals in designing and implementing team-approach, action steps.15
Four core competencies have been associated with IPE: collaborative practice; values and ethics, roles and responsibilities, communication, and teamwork.16,17 Values and ethics are related to working with individuals of other professions to maintain a climate of mutual respect and shared values. Roles and responsibilities are linked to the use of knowledge of one's own role and those of other professions to appropriately assess and address the healthcare needs of the population served.16,17 Communication is connected to effective interactions with patients, families, communities, and other healthcare professionals to support a team approach to healthcare.16,17 Working as a team applies relationship-building values and principles of group dynamics to perform effectively in varying roles to plan and implement patient/population-centered care.16,17
Quality oral healthcare can best be achieved when oral healthcare professionals work collaboratively with providers from other disciplines. A multi-professional approach, where dental hygiene students engage with other healthcare providers in the provision of primary care will likely improve patient health outcomes.3,7 Since education plays a critical role in the process of preparing future practitioners to successfully work together, understanding faculty attitudes and values towards IPE is relevant to today's educational model. While multiple levels of academic support are necessary for successful IPE implementation, ultimately it is the individual faculty members providing instruction and modeling positive attitudes towards IPE who will impact its success.2,4-7
Research exploring the knowledge and attitudes of faculty toward IPE has been limited in dental hygiene literature. Furgeson et al surveyed dental hygiene program directors in the United States (U.S.) and found only a little more than half (57%) of the respondents thought IPE was important for the dental hygiene profession, with less than half (40%) indicating that it was important at their academic institutions.18 In a regional study, Casa-Levine investigated IPE attitudes and knowledge of dental hygiene faculty and administrators in the northeastern U.S.19 While the results were favorable toward valuing IPE, only about half of the respondents indicated that they were in the initial stages of using IPE; while only 6% were using IPE as part of a major initiative and almost one quarter of the respondents had not engaged in any type of IPE activities. Results from Casa-Levine indicate the need for a national study of dental hygiene faculty attitudes toward IPE be conducted to enhance the understanding of current IPE practices.19 The purpose of this study was to survey the attitudes, barriers and IPE practices in a national sample of dental hygiene faculty.
Methods
This study was determined to be exempt from Institutional Review Board (IRB) oversight by both Old Dominion and Augusta Universities. An electronic, self-report survey was distributed to the email addresses of 1,800 faculty members from the 335 entry-level dental hygiene programs in the U.S. obtained from the American Dental Hygienists' Association website. Individual faculty email addresses were obtained from the academic program websites. The initial recruitment email provided an explanation of the study and a link to the anonymous web-based survey. Two reminders emails were sent at two and four weeks to increase survey return rate. Participants were given the option to either opt out of the self-report survey or agree to participate.
The survey instrument was a revised version of a validated survey by Vernon previously used to investigate IPE among respiratory therapists and nutrition faculties.12,13,20 Permission was granted to adapt the survey for use with dental hygiene faculty in entry-level programs. Feasibility and functionality of the survey instrument was pilot-tested with a random sample of nine full- and part-time dental hygiene faculty members; the survey was modified for clarity and length based on pilot-test results.
The 25-item survey instrument collected demographic information regarding the specific type of program setting (associate or bachelor degree granting, programs with or without a dental school), faculty appointment (full or part-time) and rank, program length (two, three, four years), enrollment, and amount and type of IPE activity. One question used a ranking system (1="most important" to 4="least important") to assess the importance of four specific IPE competencies (ethics, communication, roles and responsibilities and teamwork). Attitudes and beliefs regarding IPE education were assessed using a 5-point Likert rating system (1="strongly agree" to 5="strongly disagree"). Respondents were asked to rate (always to never) how often specific methods of instruction were used for IPE activities (case studies, on campus and off campus activities, simulation, service learning, standardized patients). One open-ended question asked participants to identify the barriers preventing them from implementing IPE. Data from this question were entered into a software application (TagCrowd, www.tagcrowd.com) to generate a pictorial description of word frequency in a word cloud with the word size proportional to its frequency as well as a numerical representation next to the individual word.
Qualtrics Survey Software (Qualtric Labs; Provo, Utah) was used for the creation of the online survey and distribution. Collected data were downloaded and imported into SPSS 25.0. (IBM; Armonk, NY). Descriptive statistics were computed from closed-ended questions. Response differences between groups by program setting and degrees granted were tested by Chi Square, the Mann Whitney U Test and the Kruksal Wallis Test of Independent Samples (p=.05). Cronbach's alpha was conducted to determine reliability of the survey's edited attitudinal section.13,20
Results
A total of 449 dental faculty (n=449) consented to participate for a response rate of 22%; however, 13% of respondents completed less than half of the survey and were not included in the analysis (n=59) for a final response rate of 22%. Demographic characteristics of the respondents and their associated programs are summarized in Table I. Respondents reported implementing IPE instructional methods (either in classroom, clinic, or community) ranging from one hour (30%), two hours (14%), three hours (5%), or four hours per week (26%); one quarter (25%) of the sample did not know how many hours were used for IPE instruction. Over half the sample (51.2%, n=145) reported having adequate time for IPE instruction. Instructional methods most frequently used separated by the degree granting categories and settings are shown in Figure 1 and Figure 2. Methods of instruction did not differ significantly across groups. Most programs used either on-site or off-site clinical activities for IPE. The range of health disciplines collaborating with dental hygiene programs for IPE are shown in Table II. Nursing (65%, n=221) of responses was identified as the most frequent collaborator; no collaborating discipline was reported by 22 respondents.
Nearly three-fourths (73%, n=281) of the respondents reported incorporating IPE. However, the frequency of IPE activities was statistically different between the type of degree awarded and program settings; a larger percentage of bachelor degree granting programs reporting IPE inclusion (X2=8.739, p=0.013). Programs associated with a dental school reported the highest degree of IPE inclusion (90%) (X2=18.07, p=0.001). A majority (85%, n=327) of respondents agreed that they would like to see a greater emphasis on IPE in curricula, a finding that was not statistically different across the groups.
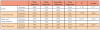
Faculty participants were asked to rank the IPE competencies of ethics, communication, roles and responsibilities, and teams and teamwork, from most to least important. Ethics was most frequently ranked as the most important competency (37%, n=139), followed by communication (23%, n=88) and roles and responsibility (21%, n=79). Overall, teams and teamwork ranked lowest (19%, n=73). Student competencies were ranked and grouped according to degree offered and program setting; however, differences in competency frequencies were not found to be statistically significant (Table IIIa and Table IIIb).
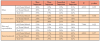
Attitudes towards IPE statements are summarized in Table IV. Mann Whitney/Wilcoxon tests indicated significant differences between faculty responses according to the type of degree offered at their institution. Cronbach's alpha revealed high internal consistency in regards to attitudes towards IPE (0.78), attitudes towards IP learning in the academic setting (0.74), and attitudes towards IP in healthcare teams (0.88).
Respondents reported general support for IPE inclusion. However, the Mann-Whitney test identified significant differences between the degree granting groups on three questions. Respondents from bachelor degree granting programs were less likely to agree that clinical problem solving can only be learned when students are taught within their individual departments/schools (p=0.022). While the majority (96%) of respondents agreed or strongly agreed with the statement "Learning with students in other health professional schools helps students become more effective members of a healthcare team," respondents from bachelor degree granting institutions were more likely to agree with this statement as compared to faculty from associate degree programs (p=0.025). Kruksal Wallis Test of Independent Samples identified significant differences between program settings for the statement, "Patients would ultimately benefit if healthcare students worked together to solve patient problems." (p=0.22).
Attitudes towards IP learning in the academic setting were generally reported as favorable. However, 35% (n=129) of respondents were unsure whether there is room for additional IPE requirements in the current curriculum; this was significantly different between respondents from different program settings (p=0.036) with programs within a dental school more likely to agree. A majority of respondents (85%, n=352) either "strongly agreed" or "agreed" that faculty should be encouraged to participate in IP courses. In regards to the statement, "My program has the resources and personnel to teach IPE courses," respondents from bachelor degree granting programs and those located in dental school settings were more likely to report agreement than those from associate's degree programs (p=0.002), and those in settings outside of a dental school (p< 0.001).
The majority of responses from both groups reflect support for IP practice in healthcare, by agreeing that participating in IPE among teams improves patient care decisions (95%), improves the efficiency of patient care delivery (80%), improves quality with IP practice (97%). The most frequently identified barriers were time (n=190), programs (n=105), faculty (n=87), scheduling (n=74), curriculum (n=70), and students (n=55). Words describing barriers to IPE implementation were displayed in a word cloud.
Discussion
Results of this study are encouraging and important to future dental hygiene education and practice. Nearly three quarters of respondents reported that they are involved in some type of IPE, with a little more than half indicating adequate instructional time in their curriculum, results similar to Casa-Levine, who found about 75% of dental hygiene faculty surveyed in the Northeastern U.S. were involved with IPE.18 One-quarter of respondents reported teaching IP collaborations for at least 4 hours per week. In a national study of U.S. dental hygiene program directors, Furgeson et al found only 57% indicated IPE was important for the dental hygiene profession.19 However, in contrast, 85% of faculty in this study agreed that faculty should be encouraged to participate in IPE and almost all respondents (95%) believed that IPE improves patient care decisions, underscoring their belief in its importance. Differences in responses between faculty members versus program directors may be attributed to the administrative insights of program directors regarding challenges involved in implementing IPE into the curricula.
Inclusion of IPE activities was reported more frequently by programs granting bachelor's degrees and those located within dental schools. This finding is likely explained by increased opportunities for collaboration, as well as more resources available in major healthcare centers where the programs most often cited as IP collaborators are located. The highest rates of IP collaboration were with nursing, occupational therapy, physical therapy, as well as intra-professional collaboration activities with dentistry. While the majority of faculty in this study indicated that there was inadequate time for IPE activities, 1 out of 4 respondents did not actually know how many hours are dedicated to IPE in the curriculum, suggesting a lack of IPE curricular knowledge amongst faculty members. This finding may be attributed to a lack of communication, or that only a small group of faculty were involved in IPE without input from other faculty members. The need for dental hygiene students to engage in IP learning experiences is critical as healthcare practice models evolve. In order to facilitate IPE, faculty may need to assume new instructional leadership roles and develop innovative curriculum.
Most respondents indicated they want a greater emphasis on IPE, demonstrating a recognition of the importance of team-based and collaborative care models, and had the perception that the current curriculum falls short. Respondents most often reported the logistical barrier of "time" when describing IPE barriers. Word cloud frequencies highlighted curriculum, which is likely related to finding time for IPE in already overloaded schedules and requirements. "Faculty" was also used as a word to describe IPE barriers, suggesting that respondents believed co-workers were less likely to support and engage in IPE than themselves. These findings are similar to other studies in both dental hygiene and other healthcare disciplines.9-10,20-22 Innovative curricular designs will be needed for many dental hygiene programs to find both the time and space for IPE activities.22,23
Faculty ranked ethics as the most important of the four IPE competences. In contrast, Vernon et al found respiratory therapy faculty ranked ethics last, while in another study, nutrition faculty ranked ethics second.12,13,20 This difference may be due to ethical practice being taught outside of IP collaborations. Communication was ranked second in importance, indicating respondents valued the importance of responsive and responsible communication within the collaborative practice model. Teams and teamwork were ranked last in this study, which was unexpected since dental hygienists are typically employed in clinical practice settings based on intraprofessional teamwork. This ranking in the context of IPE may be because many programs have practice management courses with a teamwork component. Previous studies have not ranked the specific IPE competencies by dental hygiene faculty members; however, Furgeson et al found that dental hygiene program directors strongly supported the IP competencies in general.19
Significant differences, between faculty respondents in associate vs bachelor degree granting programs, regarding attitudinal statements were found in three areas. Respondents from bachelor degree granting programs were less likely to agree that clinical problem solving can only be learned when students are taught within their individual departments; more likely to agree that learning with other health professional students helps students become more effective members of a healthcare team; and more likely to agree patients benefit from group problem solving if healthcare students worked together. These findings might be related to program setting; bachelor degree granting programs might have more access to institutional resources than associate degree programs, including the availability of more IP faculty and IP workshops.
Results demonstrated that most faculty respondents have favorable attitudes toward IPE, indicating while attitude is not a perceived barrier, nearly one out of four programs are not involved in IPE education. Understanding the barriers to implementation is important for wider incorporation of IPE, while also encouraging administrators to be more proactive in meeting the instructional needs of their faculty. In general, the majority of dental hygiene faculty respondents were supportive of teamwork, collaboration and communication through IPE for optimal patient care and improved quality of healthcare.
Limitations
Survey research has inherent bias related to the nature of self-reporting. Due to the anonymous nature of the study, it was not possible to evaluate each program individually, which may have led to over sampling. Considering that there were significantly more respondents from associate's degree versus bachelor's degree programs, results may be biased due to the degree granting institution and program setting. The low response rate (22%) also limits generalization of the results; it cannot be assumed that these findings represent all U.S. dental hygiene educators. However, it is noteworthy that this response rate is higher than previously published studies with large sample sizes.24-27 Responses may also be limited considering the online survey consisted of close-ended answers with the exception of one open-ended question related to barriers. While word frequencies displayed as a word cloud graphic for open ended questions does not provide evidence for thematic evaluation, they can be a useful first step in qualitative analysis. Future implementation of this survey is recommended to evaluate the sustainability and expansion of IPE collaborations, as well as identifying the attitudes and barriers within dental hygiene programs.
Conclusions
The need for IPE in dental hygiene programs is growing; collaborations with other healthcare professions are essential in an evolving healthcare system. Results of this study suggest that most dental hygiene faculty report positive attitudes toward IPE and a majority of programs are engaged in IPE activities at some level; however, barriers exist that may prevent expansion. Challenges of curriculum overload should also be considered when addressing Commission on Dental Accreditation (CODA) standards. Faculty must be provided with sufficient training as well as time to plan and implement IP content in the curriculum to develop successful and meaningful IPE experiences that will contribute to contemporary healthcare delivery models.
About the Authors
Susan L. Tolle, RDH, MS is a professor; Gayle McCombs, RDH, MS is a professor emeritus; both in the School of Dental Hygiene, Old Dominion University, Norfolk VA.
Marlo M. Vernon, MPH, PhD is an assistant professor; Gianluca De Leo, PhD, MBA, is a professor; both in the College of Allied Health Sciences, Augusta University, Augusta, GA.
Corresponding author: Susan L. Tolle, RDH, MS; ltolle@odu.edu
References
1. Buring S, Bhushan A, Broeseker A, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ. 2009 Jul;73(4).8-14.
2. Dallaghan G, Hoffman E, Lyden E, Bevil C. Faculty attitudes about interprofessional education. Med Educ Online. 2016 Jun 27; 21:32065.
3. Wilder R, O'Donnell J, Barry J, et al. Is dentistry at risk? A case for interprofessional education. J Dent Ed. 2008 Jun;72(11):1231-7.
4. Hinderer K, Klima D, Truong H, et al. Faculty perceptions, knowledge, and attitudes toward interprofessional education and practice. J Allied Health. 2016 Mar;45(1):1E-4E.
5. Hall L, Zierler B. Interprofessional education and practice guide no. 1: developing faculty to effectively facilitate interprofessional education. J Interprof Care. 2015 Jan;29(1):3-7.
6. Jones K, Blumenthal D, Burke J, et al. Interprofessional education in introductory pharmacy practice experiences at US colleges and schools of pharmacy. Am J of Pharma Educ. 2012 Jun;76(5):1-8.
7. Formicola A, Andrieu S, Buchanan J, et al. Interprofessional education in US and Canadian dental schools: an ADEA team study group report. J Dent Educ. 2012 Sep;76(9):1250-68.
8. Commission on Dental Accreditation. Accreditation standards for dental hygiene education programs [Internet]. Chicago: Commission on Dental Accreditation 2018 [cited 2018 Aug 27]. Available from: https://www.ada.org/~/media/CODA/Files/dental_hygiene_standards.pdf?la=en
9. Homeyer S, Hoffmann W, Hingst P, et al. Effects of interprofessional education for medical and nursing students: enablers, barriers and expectations for optimizing future interprofessional collaboration - a qualitative study. BMC Nursing. 2018 April 17(1):1-10.
10. Lash D, Barnet M, Parekh N, et al. Perceived benefits and challenges of interprofessional education based on a mutidisciplinary faculty member survey. Am J Pharm Educ. 2014 Dec; 78(10): 1-9.
11. Lawlis T, Anson J, Greenfield D. Barriers and enablers that influence sustainable interprofessional education: a literature review. J Interprof Care, 2014 Jul; 28(4): 305-10.
12. Vernon M, Moore N, Mazzoli A, De Leo G. Respiratory therapy faculty perspectives on inter- professional education: Findings from a cross sectional online survey. J Interprof Care. 2018 Mar;32(2):235-8.
13. Patton Z, Vernon M, Haymond K, et al. Evaluation of interprofessional education implementation among nutrition program directors in the USA. Top Clin Nutr. 2018 Jun;33(3):193-204.
14. Furgeson D, Kinney J, Gwozdek A, et al. Interprofessional education in U.S. dental hygiene programs: A national study. J Dent Ed. 2015 Nov;79(11):1286-94.
15. World Health Organization. Framework for action on interprofessional education & collaborative practice [Internet]. Geneva: World Health Organization 2010 [cited 2018 Apr 8]. Available from: http://www.who.int/hrh/resources/framework_action/en/.
16. Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: report of an expert panel [Internet]., Washington, DC: Interprofessional Education Collaborative. 2011 [cited 2018 May2]. Available from: https://www.aacom.org/docs/default-source/insideome/ccrpt05-10-11.pdf?sfvrsn=77937f97_2
18. Furgeson D, Inglehart MR. Interprofessional education in dental hygiene programs and CODA standards: dental hygiene program directors' perspectives. J Dent Hyg. 2017 Apr;91(2):6-14.
19. Casa-Levine C. The value of interprofessional education: assessing the attitudes of dental hygiene administrators and faculty. J Dent Hyg. 2017 Dec;91(6):49-58.
20. Vernon M, Moore N, Cummins L, et al. Respiratory therapy faculty knowledge of and attitudes toward interprofessional education. Respir Care. 2017 Jul;62(5):873-81.
21. Furgeson D, Inglehart MR. Interprofessional education in dental hygiene programs and CODA standards: dental hygiene program directors' perspectives. J Dent Hyg. 2017 Apr;91(2):6-14.
22. Mladenovic J, Tilden VP. Strategies for overcoming barriers to IPE at a health sciences university. J Interprof Educ Pract. 2017 Sep;8:10-13.
23. King S, Hall M, McFarlane L, et al. Launching first-year health sciences students into collaborative practice: highlighting institutional enablers and barriers to success. J Interprof Care. 2017 May 4;31(3):386-93.
24. Urban R, Rowe D. Knowledge, attitudes and practices of dental hygienists rgarding caries management by risk assessment. J Dent Hyg. 2015 Feb;89(1):304-62.
25. Humann P, Rowe D. Relationship of musculoskeltal disorder pain to patterns of clinical care in California dental hygienists. J Dent Hyg. 2015 Feb;89(1):55-62.
26. Essex G, Miyahara K, Rowe D. Dental hygienists' attitudes toward the obese population. J Dent Hyg. 2016 Dec;90(6):372-8.
27. Smallidge D, Boyd L, Rainchuso L, et al. Interest in dental hygiene therapy: a study of dental hygienists in Maine. J Dent Hyg. 2018 Jun;92(3):6-13.