You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
It has been well established in the literature that the origin of gingivitis and periodontitis occurs through the colonization, accumulation and subsequent maturation of a plaque biofilm. Variations to this inflammatory process are thought to be a consequence of differences in the quantity and composition of these microbial deposits in addition to being mediated by systemic and local inflammatory responses and other environmental factors.1 Good oral hygiene practices are considered to be important in maintaining good oral health.2-4 Regular oral care, focused on controlling supra-gingival plaque, can assist in slowing or reducing the tendency of plaque biofilm to shift to a pathogenic environment.5 Current preventive oral health care focuses on thorough removal of plaque biofilm to prevent, reduce or even reverse oral disease processes, such as gingivitis.6-10 Dentists and dental hygienists have commonly recommended daily mechanical plaque biofilm control, specifically toothbrushing for thorough removal of plaque biofilm and prevention of further plaque accumulation.3,5,9,10
Toothbrushing as a means to mechanically remove plaque biofilm is extremely effective, however it has not been shown to be thoroughly effective in cleaning interdental areas when used exclusively.4,6,10,11 Schmid12 classified interdental embrasures, depending upon how much the interdental papilla fills the gingival embrasure and advised that dental floss be used in Type-I embrasures, and the incrementally wider interproximal and unitufted brushes be used in Type-II and III, respectively.12
In a systematic review of twelve studies on flossing, Sambunjak et al.13 concluded that there is some evidence to support the theory that flossing, in addition to toothbrushing, reduces gingivitis and plaque biofilm accumulation as compared to toothbrushing alone. Routine use of dental floss in conjunction with toothbrushing has been shown to reduce the amount of plaque biofilm accumulation especially in the proximal areas.5,6,14 Additionally, plaque biofilm reduction may not only prevent the onset and severity of gingivitis but may also lower the risk of cardiovascular disease.15,16 Flossing is also utilized to clear food impaction from interdental areas.17 However, in regard to compliance, patients frequently exhibit a reluctance or an inability to perform flossing on a regular basis.9,14
Gomes et al.18 have presented a modification in flossing called Knotted Floss (KF) technique and advocated its use in wider embrasure areas. The modification was made to increase the effective width of the floss, thus enabling it to be used in embrasures wider than those recommended for conventional floss. To modify the floss, a knot is tied at any distance in the middle third of the floss length. The floss can then be inserted past the interdental contact point by the conventional finger flossing (CF) technique in the non-knotted area and then during the "to and fro movement" on the tooth surface cervical to the contact, the knotted area is then engaged through the embrasure (Figure 1).18
Asadoorian6 conducted a literature search and critical analysis of studies on the efficacy of manual finger flossing, flossing aids and devices, and other interproximal aids. However, no studies have been identified in the literature that have evaluated either the efficacy, safety, or the patient preferences of the KF technique as an adjunct to toothbrushing.
To assess the efficacy of an interdental cleansing method, one must consider two reference points: theoretical efficacy of the method as determined by its clinical evidence and practical efficacy based upon the acceptability of the procedure, which in turn influences the long-term compliance.6 Theoretical efficacy can be determined by evaluating the effects of the test device or procedure on plaque biofilm accumulation scores and the presence of gingival inflammation and bleeding. The potential of the test device to cause gingival trauma during use must also be evaluated. The purpose of this study was to compare the changes in scores of plaque biofilm accumulation, gingival inflammation, sulcular bleeding and presence of gingival trauma due to flossing using the KF technique versus the CF technique, in Type-I gingival embrasures. Preferences between the two flossing techniques were also evaluated.
Methods
Sample Selection Criteria
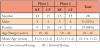
A sample of 30 patients, aged 18 years and above, were randomly selected from the patients visiting Uttaranchal Dental and Medical Research Institute outpatient department, for a dual phase, examiner blinded, crossover clinical trial. A preliminary pilot study with six subjects was conducted in order to estimate the necessary variables required to determine the sample size according to the criteria of Chow et al.19 A sample size of 28 was calculated to achieve a sample power of 80%, and was increased to 30 to adjust for potential attrition.20 Inclusion and exclusion criteria used for subject selection are shown in Table I. The trial was conducted as per the World Health Organization guidelines for good clinical practice23 and was approved by the Uttaranchal Dental and Medical Research Institute Ethics Committee. This study was part of a larger study protocol involving different groups comparing the KF technique with the CF technique, along with the use of interdental brushes and unitufted brushes in Type-II and Type-III embrasures, respectively. No subjects overlapped amongst the sample groups of the larger study protocol.
Study Design
Each potential participant received written and verbal instructions on the two flossing techniques prior to starting in the study. The first and third investigator demonstrated both flossing techniques on typodonts in 30-minute educational sessions over three consecutive days. Each educational session had no more than ten participants. On the third day, the participant's proficiency in both techniques on typodonts was confirmed separately by both investigators, informed consent taken, and the subject was enrolled into the fourteen-week study. Failure to perform the techniques as instructed required an additional 30-minute educational session or exclusion from the study.
In the first phase, half of the subjects were randomly assigned to use either the CF or the KF technique. Only the first investigator was responsible for this allocation and the other investigators were blind as to which technique the subject was assigned to. The treatment phase consisted of six weeks of daily use of the assigned technique and was followed by a 14- day washout period after which the second phase began and the subjects used the other flossing technique. Subjects were given their assigned floss products by the first investigator exclusively at the baseline appointment for each phase. Subjects assigned to the CF technique received 90 pieces of waxed floss (Reach,®Johnson & Johnson Consumer Inc.; New Brunswick, NJ), each piece 15 centimeters in length, equally divided into three plastic bags. Subjects assigned to the KF group received the same bags of floss except that each floss strand had a simple knot tied at approximately the middle of the strand. All participants received a toothbrush (Oral-B® all-rounder soft; Procter & Gamble; India Ltd.) and dentifrice (Colgate® Strong Teeth; Colgate-Palmolive; New York, NY).
Participants were given detailed instructions regarding the oral hygiene study regimen (Table II). As in any 2x2 crossover study, trial phases must be separated by a washout phase sufficiently long enough to rule out any carryover effect of the first treatment procedure prior to proceeding to the second.19,24 Carter-Hanson et al.14 used a 2-week washout period in their crossover study comparing a floss holding device to conventional finger-flossing procedure, while Torkzaban et al.25 used a 7-day washout period in their crossover study comparing brushing and flossing sequencing. Data from the pilot study showed no significant intrasubject differences at the start of each treatment phase, when a 2-week washout period was used, while when a 1-week washout was employed, there was no conclusive evidence that the washout was effective. Hence, a washout of 2-weeks was selected between treatment phases allowing the participants time to return to their original oral status and establish parity in baseline clinical measurements, prior to starting the second treatment phase. Moreover, the same inclusion and exclusion criteria were applied to all participants at the start of each treatment phase. Subjects were instructed to perform their normal oral hygiene practices of toothbrushing with dentifrice and refrain from using any floss or any additional plaque biofilm control aids during the washout period.
Clinical Evaluations
Clinical evaluations of all subjects were performed beginning with baseline, and at 2-weeks, 4-weeks, and 6-weeks of each treatment phase. Adjacent teeth and gingiva at the test sites were scored with the Rustogi Modification of Navy Plaque Index (RMNPI),26 Lobene's Modified Gingival Index (MGI),27 and Barnett's Modified Papillary Bleeding Index (MPBI).28 Sequencing of the examination was specifically chosen as RMNPI, followed by MGI and MPBI, to avoid the possibility of plaque removal during the recording of the other two indices.14,29 A plaque disclosing agent was used to identify the location and quantity of plaque. Gingival trauma (GT) was assessed as the presence or absence of signs of trauma in the marginal and papillary gingiva of adjacent teeth according to methodology proposed by Carter-Hanson et al.14 Facial and lingual surfaces were visually examined for gingival trauma. Presence of lacerations, floss cuts, or demarcation line/indentation at the site was scored as one, while a score of zero was recorded in the absence of any signs of trauma. The score per subject was obtained by totaling all scores and dividing by the number of sites examined.14 Indices were recorded by the second and fourth investigators. Intra- and inter-examiner reliability was calculated prior to the commencement of the study, as well as at two weekly intervals over the duration of the study by utilizing nine additional subjects who were not part of the sample. The study schedule was organized so that no more than six subjects reported for examination on any given day of the week. The two investigators involved in the recording of data were blinded as to which technique the subject was using as well as the amount of unused floss, if any, at the end of the respective treatment phase.
Subject Compliance
Each subject received a compliance diary at the baseline appointment of each treatment phase and the diaries were collected at the end of each phase by the first investigator. Participants recorded each flossing experience along with any other events he/she felt significant. Compliance was further established by dispensing a specific amount (90 pieces) of the assigned floss product per treatment phase. Subjects returned any unused portion of floss product to the first investigator at the end of each phase; thus, non-compliance was estimated. Additionally, a patient satisfaction questionnaire, consisting of specific choice type questions, substantiated compliance. Questions did not require participants to compare specific techniques by name, rather by phase 1 versus phase 2, and were completed by all participants at the completion of study. The first investigator later decoded the sequence of choices as per the random allocation performed at start of study.
Validity and Reliability
Prior to beginning the study, a panel of three experts consisting of senior staff members (two in the field of oral health and one in clinical psychology) evaluated the questionnaire used in the initial pilot study and deemed it to be valid. Intra- and inter-rater reliability was established through the collection of data from subjects who were not part of the sample during pilot testing. Inter- and intra-rater reliability was measured at two-week intervals, using a minimum of nine randomly selected volunteers from the outpatient clinic. These volunteers fulfilled the selection criteria but did not participate in the treatment phases. Reliability was assessed for the RMNPI and MGI.
Statistical Analysis
Data were analyzed using SPSS software version 17.0 (SPSS; Chicago, IL, USA). Gender-wise distributions were compared and the mean age was calculated. A 3-factor analysis of variance (ANOVA) was conducted to examine the effects of sequence of the treatment phase and the possibility of any carry-over of the effects of the first treatment phase into the second, in spite of the 2-week washout phase. Following statistical confirmation that treatment sequencing was not a significant factor, data was further analyzed as at baseline and post intervention. For each of the outcome variables, intra-group differences were analyzed using a paired t-test; inter-group differences were analyzed using the student's t-test. Direct comparisons were performed on the questionnaire responses between the two groups. All results were examined for statistical significance (p ≤ 0.05).
Results
Inter-examiner reproducibility for exact agreement (K = 0.76 ± 0.07, SE) was assessed for readings made between the second and fourth investigators, indicating an excellent level of agreement. An intra-examiner reproducibility for exact agreement (K = 0.81 ± 0.06, SE) and (0.79 ± 0.08, SE) for replicating the readings were recorded by the second and fourth investigators, respectively, also indicating an excellent level of agreement.
Data gathered from one subject was excluded due to non-compliance; the participant introduced a knot into the floss himself during phase-2 when the CF technique was to have been used. Another subject was withdrawn before the start of phase-2 as the plaque and gingival indices were below the sample selection requirements, even after the washout phase, and no longer met the inclusion/exclusion criteria. All clinical data is based on recordings from the twenty-eight subjects who successfully complied with, and completed both the treatment phases of study; no data was included from the two subjects that were withdrawn. Participant demographics are displayed in Table III. Each subject was scored in each of the two treatment phases at baseline, 2-weeks, 4-weeks and 6-weeks for RMNPI, MGI, and MPBI. Areas of GT were also assessed at 2-weeks, 4-weeks and 6-weeks in both treatment phases. Scores recorded from the subjects during use of the KF technique were grouped together and the means and standard deviation recorded. Similarly, scores recorded during use of the CF technique were grouped together, and means and the standard deviation were calculated.
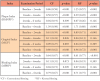
Mean scores at baseline, 2 weeks, 4 weeks and 6 weeks for RMNPI, MGI, MPBI and GT are shown in Table IV. Baseline scores for the first three indices were similar. On comparison of RMNPI scores between the two groups, mean scores for the KF group were found to be significantly lower than those of the CF group at 2-weeks, 4-weeks and 6-weeks. Comparison of MGI and MPBI mean scores did not reveal any statistically significant difference between both the groups at all the time points.
When comparing within respective group the mean difference in RMNPI scores, the differences in scores between baseline and 2-weeks, 2-weeks and 4-weeks, as well as scores between baseline and 6-weeks, were statistically significant for both treatment groups (p = 0.05). There was no significant difference between the mean RMNPI at 4-weeks and 6-weeks for either group (Table V).
When comparing mean differences in MGI within each treatment group, it was noted that the differences within groups at baseline and 2-weeks, as well as baseline and 6-weeks, for both the CF and the KF treatment groups, were statistically significant (p ≤ 0.05). The mean difference between MGI at 2-weeks and 4-weeks was also significant for the CF group but not for the KF group (Table V). No significant differences were found between MGI at 4-weeks and 6-weeks for either group.
Mean differences within groups between MPBI at baseline and 2-weeks and baseline and 6-weeks were statistically significant within both treatment groups (p ≤ 0.05). No significant differences were identified between MPBI at 2-weeks and 4-weeks, and 4-weeks and 6-week intervals for either treatment group (Table V). Patient compliance and satisfaction were estimated by way of the entries made in the compliance diaries, the amount of unused floss and the questionnaire completed at the end of final phase. Over 93% of the subjects reported flossing twice a day, 7 days a week. Participant responses and preferences identified in the questionnaire are seen in Table VI.
Over half of the subjects (54%) completing the study felt that the KF technique was easier to use than the CF technique, while 46% felt that CF was easier to use. An equal number said it took less time to use the CF technique. Three-fourths (75%) subjects were of the opinion that they were able to clean interproximal areas better when using the KF and 71% of the participants expressed a desire to continue using KF as their flossing method of choice in their future oral hygiene practices.
Discussion
Dental flossing is still one of the most effective means for the removal of interproximal plaque biofilm and cleansing of interdental areas post food-impaction.13,30-32 However, investigators have reported that people, in general, do not use dental floss routinely,9,14 creating a need for alternative methods and interdental cleaning aids, to improve acceptability and compliance. In such an endeavor, Gomes et al18 in 2016, proposed a KF technique which helped dislodge plaque biofilm and food debris from wider interdental areas, and therefore probably increased its acceptability. Results from the current 98 day, 2-phase, clinical study indicate a similar ability of the KF technique as compared to CF with respect to removing interdental plaque, decreased gingival inflammation and bleeding. There were no statistically significant signs of gingival trauma arising from either flossing technique. Additionally, the subjects at the end of the study stated a preference towards the KF technique and wished to continue to use it in the future.
In order to obtain an effective level of interdental plaque biofilm removal, the use of a dental floss or any other interdental device should be combined with a good brushing technique.25,33,34 The present trial evaluated the use of brushing combined with each of two techniques of flossing and not of dental floss technique exclusively.
Numerous studies in the literature compare the CF with mechanical flossing devices and other interdental aids.14,33,34 These studies have shown that flossing devices hold no clinical advantage in the reduction of plaque and improved gingival index scores when compared to CF. A study by Carter-Hanson et al.14 is most comparable to the present study with its two-phase, single blind, crossover clinical design, although it was only 74 days in comparison to 98 days of the present study. Carter-Hanson et al.14 reported a significant decrease in plaque, gingival inflammation and bleeding scores over the period of their study with the use of CF and a floss holder. Patients preferred the floss devices in spite of the increased cost in comparison to use of CF.14 In the present study, the KF technique did not involve any increased expenditures by the patient, unlike the floss devices used in previous studies.14,33,35 Carter-Hanson et al.14 had expressed the opinion that such preference for a floss product could increase a patient's compliance to incorporate flossing into their daily oral care routine.
Cronin et al.33 compared the safety and efficacy of a battery-operated interdental cleaning device fitted with either a fork-like floss holder or a pick attachment, versus CF in the reduction of plaque biofilm scores and gingival inflammation when combined with manual toothbrushing over a 30-day period. Participants were split equally into three parallel groups. All three groups showed similar scores at baseline but showed statistically significant reductions after 30 days in gingival inflammation and bleeding scores, while plaque scores reduced significantly in the floss holder device group and the CF group only. Plaque biofilm reduction was reported to be better for the floss holder device group as compared to the pick-attachment group. The present trial has similar results, with the statistically significant reductions seen in scores of plaque biofilm, gingival inflammation and gingival bleeding over a 6-week period after using either the CF or KF technique. The KF group had significantly more reduction in plaque biofilm indices from baseline scores and at time points from 2 weeks, 4 weeks and 6 weeks in comparison with reductions seen in the CF group at identical time-points. Subjects selected for the study had moderate amount of plaque biofilm, gingival inflammation and gingival bleeding, as inferred by their baseline scores. Madan at al.36 concluded that most dental patients do not have an awareness about flossing and hence in this study, patients were chosen who were not regular flossers and didn't have any advanced periodontal disease. Hence, the sample was reflective of a standard population of relatively healthy individuals with gingivitis.
The presence of high compliance in this trial can be attributed to the subject's psychological effect of impending study or the Hawthorne effect.14,37,38 The fact that observance of gingival trauma was negligible may be because of the proper flossing instructions at the start of the study. However, although the subjects demonstrated the flossing technique on typodonts to the satisfaction of the instructors, the actual flossing by the subjects was done unsupervised and with no interference by the instructors. During the time of oral examinations, the subjects were oblivious to the scores and were not given any instructions as to how to modify their flossing habits. Hence, the inference that the KF technique can be used safely for interdental cleansing of Type-1 gingival embrasures, albeit only after proper flossing instructions have been given.
A meta-analysis by Berchier et al.39 explored the impact of adding flossing as an adjunct to brushing, and its effect on the indices of plaque biofilm and gingival health. They failed to find statistically significant improvement in these scores, but at the same time suggested that one has to have proper instructions to achieve a goal of high-quality flossing. In addition, there has been recent press coverage calling into question the recommendation for daily flossing.40 However, even though the average benefit of CF and modified techniques like the KF technique is probably small, there are no documented harms nor increased costs to the patient. Since more than half of all Americans are said to be affected by periodontal disease,41 even a small benefit to their oral hygiene may prove beneficial.32
In the present study, no preference was given to the selection criteria for choosing the test area (upper or lower jaws, left or right sides). Similarly, there was no criteria for inclusion of only left-handed (LH) or right-handed subjects (RH). In a study of 40 subjects, Kadkhodazadeh et al.42 reported that LH subjects have lower plaque biofilm scores in the right quadrants and RH subjects have lower plaque biofilm indices in the left quadrants. Cakur et al.43 studied forty-six adolescents and reported that RH subjects have lower oral hygiene scores and a lower incidence of caries, possibly because of their better manual dexterity and brushing efficiency. These confounding variables do not necessarily affect the present crossover study, as these variables were common during both trial phases.
Limitations
This trial was limited to the evaluation of the KF technique in type 1 embrasures in subjects who otherwise were not regular users of interdental oral hygiene aids and oral irrigators. The sample consisted of individuals of both sexes, different socioeconomic strata, and varied dietary habits. A crossover study on flossing by Torkzaban et al.25 found that there was a significant influence of gender on the plaque scores and bleeding points index. The present trial did not compare the scores between different genders. Similarly, this evaluation of the KF technique was not performed in cohorts comprised of different types of embrasures, a variety of socio-economic groups, and groups with different kinds of eating habits. Hence, there is a need for a larger sample size such that all confounding variables are identified, their influences evaluated and compared. Volunteers who enrolled into the study were given instructions in flossing technique and were thus extra-motivated in diligently performing the procedure as required. It is uncertain whether favorable results in the efficacy of both flossing techniques were achieved by cognitive behavioral intervention, or by the Hawthorne effect.37 This limitation may be diminished in a long-term study. Moreover, it cannot be guaranteed that a recommendation of twice a day flossing, as performed in this study, will not have a negative compliance in the lay public. Hujoel et al.44 have cautioned against the extrapolation of results obtained from professionally supervised flossing to typical floss users since unsupervised self-flossers didn't show any significant reduction in incidence of interdental caries. Conversely, the fact that the subjects were not directly supervised during the flossing procedure per se meant that the verification of their compliance depended only on their honesty.45 It is possible that the presence of a knot in an otherwise smooth dental floss has the increased potential to cause gingival trauma. For ethical reasons, this study excluded subjects with severe inflammatory gingival disease needing urgent professional care. Since severely inflamed gingival tissues are more prone to injury, it is probable such subjects would have had more cases of gingival trauma.
Conclusion
Results from this two-phase, single blinded clinical trial demonstrate that KF is a safe and effective interdental oral hygiene cleansing technique for reducing plaque biofilm accumulation, gingival inflammation and bleeding, as compared to CF techniques in Type I gingival embrasures, when used in conjunction with regular toothbrushing over a 6-week period. The KF technique is an effective alternative to CF provided proper instructions are given regarding its use and the procedure is performed in conjunction with toothbrushing. Patient preference for the KF technique indicates that it can be a viable alternative to CF in assisting patients in establishing regular and cost-effective interdental cleaning habits in Type I gingival embrasures.
About the Authors
Aaron F. Gomes, MDS is a professor and chair of the Department of Periodontology and Oral Implantology; Amit Rekhi, MDS is a senior lecturer in the Department of Public Health Dentistry; S Meru, MDS is a professor and chair of the Department of Oral Medicine and Radiology; Gaurav Chahal, MDS is a senior lecturer in the Department of Periodontology and Oral Implantology; all at the Uttaranchal Dental and Medical Research Institute, Uttarakhand, India.
Corresponding author: Aaron F. Gomes, MDS; draarongomes@gmail.com
References
1. Mombelli A. Microbial colonization of the periodontal pocket and its significance for periodontal therapy. Periodontol 2000. 2018 Feb;76(1):85-96.
2. Cepeda MS, Weinstein R, Blacketer C, Lynch MC. Association of flossing/inter-dental cleaning and periodontitis in adults J Clin Periodontol. 2017 Sep;44(9):866-71.
3. Hayasaki H, Saitoh I, Nakakura-Ohshima K, et al. Tooth brushing for oral prophylaxis. Jpn Dent Sci Rev. 2014 Aug;50(3):69-77.
4. Nightingale KJ, Chinta SK, Agarwal P, et al. Toothbrush efficacy for plaque removal. Int J Dent Hyg. 2014 Nov;12(4):251-6.
5. Imai PH, Yu X, MacDonald D. Comparison of interdental brush to dental floss for reduction of clinical parameters of periodontal disease: a systematic review. CJDH. 2012 Feb;46(1):63-78.
6. Asadoorian J. Flossing: Canadian dental hygienists association position paper. CJDH. 2006 May;40(3):112-25.
7. Pinto TM, de Freitas GC, Dutra DA, et al. Frequency of mechanical removal of plaque as it relates to gingival inflammation: a randomized clinical trial. J Clin Periodontol. 2013 Oct;40(10):948-54.
8. Sälzer S, Slot DE, Van der Weijden FA, Dörfer CE. Efficacy of inter-dental mechanical plaque control in managing gingivitis - a meta-review. J Clin Periodontol. 2015 Apr;42(Suppl16):S92-105.
9. Sälzer S, van der Weijden GA, Dörfer CE, Slot DE. Current evidence on prevention of gingivitis: oral hygiene devices and dentifrices. Int J Evid Based Pract Dent Hyg. 2017; 3(2):118-27.
10. van der Weijden GA, Slot DE. Interdental oral hygiene- the evidence. In: Bartold PM, Lin LJ. editors. Multi- Disciplinary Management of Periodontal Disease. Adelaide: Asian Pacific Society of Periodontology; 2012. p.16-33.
11. Gluch JI. As an adjunct to tooth brushing, interdental brushes (IDBs) are more effective in removing plaque as compared with brushing alone or the combination use of tooth brushing and dental floss. J Evid Based Dent Pract. 2012 Jun;12(2):81-3.
12. Schmid MO. Plaque control. In: Carranza FA, Jr. editor. Glickman's Clinical Periodontology. 6th ed. Tokyo: Igaku-Shoin/Saunders International; 1984. p.671-702.
13. Sambunjak D, Nickerson JW, Poklepovic T, et al. Flossing for the management of periodontal diseases and dental caries in adults. Cochrane Database Syst Rev. 2011 Dec 7;12:CD008829.
14. Carter-Hanson C, Gadbury-Amyot C, Killoy W. Comparison of the plaque removal efficacy of a new flossing aid (Quik Floss) to finger flossing. J Clin Periodontol. 1996 Sep;23(9):873-8.
15. Dhadse P, Gattani D, Mishra R. The link between periodontal disease and cardiovascular disease: how far we have come in last two decades? J Indian Soc Periodontol. 2010 Jul;14(3):148-54.
16. Mathews MJ, Mathews EH, Mathews GE. Oral health and coronary heart disease. BMC Oral Health. 2016 Apr 30;16:122.
17. Li Q-L, Ying Cao C, Xu Q-J, et al. Atraumatic restoration of vertical food impaction with an open contact using flowable composite resin aided by cerclage wire under tension. Scientifica (Cairo). 2016 Jun;2016: 4127472.
18. Gomes AF, Meru S, Rekhi A. Knotted floss technique. J Adv Res Dent Oral Health. 2016 Feb;1(1):6-7.
19. Chow S-C, Shao J, Wang H. Sample size calculations in clinical research. 2nd ed. Boca Raton: Chapman & Hall /CRC; 2008.
20. Sakpal TV. Sample size estimation in clinical trial. Perspect Clin Res. 2010 Apr;1(2):67-9.
21. Silness J, Loe H. Periodontal disease in pregnancy II. correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964 Feb;22:121-35.
22. Loe H, Silness J. Periodontal disease in pregnancy I. prevalence and severity. Acta Odontol Scand.1963 Dec;21:533-51.
23. World Health Organization. Handbook for good clinical research practice (GCP): guidance for implementation [Internet]. Geneva: World Health Organization; 2005 [updated 2012 Jun 16; cited 2015 Apr 6]. Available from: https://apps.who.int/iris/bitstream/handle/10665/43392/924159392X_eng.pdf?sequence=1&isAllowed=y
24. Wellek S, Blettner M. On the proper use of the crossover design in clinical trials: part 18 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2012 Apr;109(15): 276-81.
25. Torkzaban P, Arabi SR, Sabounchi SS, Roshanaei G. The efficacy of brushing and flossing sequence on control of plaque and gingival inflammation. Oral Health Prev Dent. 2015;13(3):267-73.
26. Rustogi KN, Curtis JP, Volpe AR, et al. Refinement of the Modified Navy Plaque Index to increase plaque scoring efficiency in gumline and interproximal tooth areas. J Clin Dent. 1992;3(Suppl C):C9-C12.
27. Lobene RR, Weatherford T, Ross NM, et al. A modified gingival index for use in clinical trials. Clin Prev Dent. 1986 Jan;8(1):3-6.
28. Barnett M, Ciancio S, Mather M. The modified papillary bleeding index: comparison with gingival index during the resolution of gingivitis. J Prev Dent. 1980; 6:135-8.
29. Gomes AF, Meru S, Rekhi A. Re: Reducing dental plaque and gingivitis with 0.6% Cortex Ilicis Rotundae toothpaste: a randomized, double-masked clinical trial. J Periodontol. 2017 Jan; 88(1):1.
30. Bergenholtz A, Brithon J. Plaque removal by dental floss or toothpicks. an intra-individual comparative study. J Clin Periodontol. 1980 Jun;7(6):516-24.
31. Blanck M, Mankodi S, Wesley P, et al. Evaluation of the plaque removal efficacy of two commercially available dental floss devices. J Clin Dent. 2007;18:1-6.
32. American Dental Association. ADA news releases: federal government, ADA emphasize importance of flossing and interdental cleaners [Internet]. Chicago: American Dental Association; 2016 Aug 04 [cited 2018 Apr 20]. Available from: https://www.ada.org/en/press-room/news-releases/2016-archive/august/statement-from-the-american-dental-association-about-interdental-cleaners.
33. Cronin MJ, Dembling WZ, Cugini M, et al. A 30-day clinical comparison of a novel interdental cleaning device and dental floss in the reduction of plaque and gingivitis. J Clin Dent. 2005;16(2):33-7.
34. Azcarate-Velazquez F, Garrido-Serrano R, Castillo-Dalí G, et al. Effectiveness of flossing loops in the control of the gingival health. J Clin Exp Dent. 2017 Jun 1;9(6):e756-e761.
35. Spolsky VW, Perry DA, Meng Z, Kissel P. Evaluating the efficacy of a new flossing aid. J Clin Periodontol. 1993 Aug;20(7):490-7.
36. Madan C, Arora K, Chadha VS, et al. A knowledge, attitude, and practices study regarding dental floss among dentists in India. J Indian Soc Periodontol. 2014 May;18(3):361-8.
37. Choo A, Delac DM, Messer LB. Oral hygiene measures and promotion: review and considerations. Aust Dent J 2001 Sep;46:(3):166-73.
38. Imai PH, Hatzimanolakis PC. Encouraging client compliance for interdental care with the interdental brush: the client's perspective. CJDH. 2010 Mar;44(2):56-60.
39. Berchier CE, Slot DE, Haps S, van der Weijden GA. The efficacy of dental floss in addition to a toothbrush on plaque and parameters of gingival inflammation: a systematic review. Int J Dent Hyg. 2008 Nov;6(4):265-79.
40. Donn J. Medical benefits of floss unproven [Internet]. Holmdel (NJ): Associated Press; 2016 August 2 [cited 2018 Apr 2018]. Available from https://apnews.com/f7e66079d9ba4b4985d7af350619a9e3
41. Eke PI, Dye BA, Wei L, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol. 2015 May;86(5):611-22.
42. Kadkhodazadeh M, Khodadustan A, Amid R, Darabi A. Plaque removal ability in left- and right-handed patients in different parts of the oral cavity. J Periodontol Implant Dent. 2012;4(1):24-8.
43. Çakur B, Yıldız M, Dane S, Zorba YO. The effect of right or left handedness on caries experience and oral hygiene. J Neurosci Rural Pract. 2011 Jan-Jun;2(1):40-2.
44. Hujoel PP, Cunha-Cruz J, Banting DW, Loesche WJ. Dental flossing and interproximal caries: a systematic review. J Dent Res. 2006 Apr; 85(4):298-305.
45. American Academy of Periodontology. More than a quarter of U.S. adults are dishonest with dentists about how often they floss their teeth [Internet]. Chicago: American Academy of Periodontology; 2015 Jun 23 [cited 2018 Apr 30]. Available from: https://www.perio.org/consumer/quarter-of-adults-dishonest-with-dentists