You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Prosthodontic Solutions for Edentulism
Thomas M. Bilski, DDS
Edentulism is more common today than many oral practitioners may realize. This article will review and update restoration and maintenance of natural dentition, examine the health of the edentulous population, and focus on the prosthetic treatment model.
Restoring and Maintaining Natural Dentition
With a totally or partially edentulous patient, the initial tasks in the dental office are to complete a thorough medical history review, conduct a caries risk assessment, and determine periodontal classification. After the information-gathering stage involving these factors, the oral practitioner should have an understanding of the patient's lifestyle and attitude in regard to moving forward to maintain remaining dentition or discuss alternative therapies to restore the oral cavity with fixed or removable prosthetics. If the patient chooses to maintain the dentition, the patient should have an understanding of one's state of oral health and a strong commitment to follow therapies to optimize the oral cavity. Improved oral hygiene regimens with instrumentation, increased re-care appointments, and increased home care with floss, oral gels, rinses, and other methods are considerations. The patient should be aware of the need for caries control, periodontal therapy, potential endodontic treatment, and long-term restorations, all of which will result in higher fees and longer treatment time.1Based on socioeconomics and demographics, patients with lower incomes tend to delay treatment, prolonging the eventual progressively destructive nature of caries and periodontal disease and ultimately leaving them with the decision to extract remaining non-restorable natural dentition.2 The most effective therapy is to eradicate the disease process early.3If the patient has the ability and commitment to save the dentition, the oral practitioner may present goals for long-term restorations, emphasizing a strict daily oral hygiene regimen and commitment to in-office re-care appointments for evaluation of oral cavity health and the health of the restorations.
Health in the Edentulous Population
Edentulism interferes with a patient's quality of life. Elderly or disabled patients may become debilitated and require assistance from family or caregivers outside the home. The aging population is prescribed multiple medications that create dry mouth, decrease salivary flow, and increase bacteria that are harmful to systemic health and the oral cavity.4 These factors lower the body's ability to fight infection, potentially creating a more severe oral infection.5
The edentulous population has a lower intake of fruit, vegetables, fiber, and carotene.6 Edentulous patients also have a higher prevalence of obesity, an increase in gastrointestinal disease, and an increase in cholesterol and saturated fats.6 They also have an increased risk of non-insulin-dependent diabetes mellitus and pancreatic cancer.6
Prosthetic Models
Prosthetic treatment options that dentists offer to edentulous patients should include basic principles that meet the desires and needs of the patient. Options that are affordable, comfortable, esthetic, maintainable, and allow for proper linguistics are the primary focus of the prosthetic model. Alternative treatment options for edentulous patients include the following:
• Complete dentures
• Implant-retained complete dentures (including soft-tissue support)
• Removable with prefabricated attachments
• Removable with bar attachments
• Implant-supported complete dentures
• Fixed screw-retained (all on "X")
• Fixed cement-retained, milled, or stock abutments
• Removable bar-supported (bar-retained overdenture)
To achieve success in providing prosthetics to edentulous patients, the dentist must consider the sustainability parameters of occlusion and the balance of bite forces in centric occlusion. What a dentist provides to the patient in regard to prosthetics ultimately impacts the patient's ability to adapt to the teeth chosen and the final vertical dimension. In a study, 50 totally edentulous patients (aged 44 to 86 years, 15 men and 35 women) received new dentures.7 The study began with later cephalometric images with the existing dentures in place and ended with final lateral cephalometric images of the new dentures in place. McNamara-Ricketts analysis was performed along with T-scan III analysis for functional parameters of occlusion. The results of the 3-month T-scan III showed that occlusion time, defined as the time from the first contact of occluding teeth to maximum intercuspation, was longer for the entire group. There was no difference based on gender, age, denture wearing time, or the edentulous period. Overall, the study suggested that a shortening of occlusal time showed progressive adaptation to the new dentures. Edentulous patients who received complete dentures with appropriate vertical occlusal dimension and bite balance in centric occlusion showed progressive adaptation. The time frame for adaptation in the study was 3 months (in practice, adaptation may be longer or shorter and specific to the individual).
Another consideration is the esthetic needs of the edentulous patient. Patients may communicate their esthetic needs based on emotional factors; they may want to attend events with a fabulous smile, to have better lip support, to look younger, and to have their partner be attracted to them and their smile. In a study comparing patient expectations and satisfaction with their complete dentures, 283 subjects were interviewed during the process of complete denture fabrication.8 The median age was 58 years; 48% were men, and 52% were women. Expectations and satisfaction were based on a scale of 1 through 10. The study revealed that men had higher expectations than women, but there was no difference in satisfaction.
Prosthodontic Solutions
The remainder of this article will focus on prosthetic solutions with complete dentures and removable partial dentures, implant-retained soft-tissue-supported dentures, removable complete dentures with prefabricated attachments, implant- and bar-supported removable complete dentures, and fixed screw-retained prosthetics. Socioeconomics and demographics may influence the decisions from patients on the type of final prothesis that they choose.The dentist's duty is to provide guidance so that patients understand what they have chosen, the commitment to oral hygiene care for the prosthesis and the oral cavity, and the solution the prosthesis is providing for them.
Complete Denture and Removable Partial Denture Options
Complete dentures have been fabricated since 700 BC.9Dentures were typically made from animal and human teeth, were relatively easy to produce, and remained popular until the mid-1800s.10These types of materials tended to discolor and deteriorate, which led to the innovation of placing porcelain teeth into Vulcanite rubber, a concept developed by silversmith and goldsmith Claudius Ash.11After the turn of the 20th century, acrylic, resins, and metals were developed to produce less costly prostheses.12Currently available are high-pressure injected resins, polymethyl methacrylate (PMMA) milled and characterized complete dentures, and 3-dimensional (3D) printed complete dentures that can be fabricated from intraoral imaging. As technology and techniques advanced, differences became evident in design of mature and vintage complete dentures and removable partial dentures compared with current times (Figure 1 and Figure 2). Comfort, esthetics, and function are the main concerns and requests from patients; however, different patients have different levels of expectation and satisfaction.13When dentists provide the best principles of midline and vertical dimension, obtain balance in occlusal bite forces, and receive approval of tooth selection from the patient, the patient will have a shorter adaptation time for a removable prosthesis7,8,14(Figure 3).
Implant-Retained Soft-Tissue Supported Complete Dentures
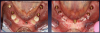
Patients seeking more comfort, better retention, and confidence from implant-retained complete dentures may choose narrow-diameter dental implants in the mandibular arch, primarily making this decision based on the lower fees for mini-implant services.15 Figure 4 and Figure 5 depict a common scenario of a maxillary complete denture opposing an implant-supported (mini-implant) complete denture. Ten years prior, the patient chose to have her mandibular arch treated with narrow-diameter implants and a mandibular removable overdenture. Figure 5 shows significant bone loss and soft-tissue recession around the narrow-diameter implants. The mini-implants serviced the patient well for 10 years but left her with a greater challenge and cost to restore the mini-implants with a new prosthesis. The dentist needed to re-engineer a means for retention other than the current ball and o-ring attachments. Over time the overdenture housings and o-ring assembly created a deformation of the ball shape of the mini-implants, decreasing the retentive nature of the o-ring and ball attachment properties. Ten years of mastication and metal-on-metal lateral movement contributed to this deformation. At 87 years old, this patient did not want to undergo additional surgical implant therapies and was looking for an alternative. The mini-implants still were able to service her. An alternative treatment option requires a cast or a milled retention bar to splint the remaining implants and development of a removable overdenture that will be retained by prefabricated attachments.
Removable Complete Denture With Prefabricated Attachments
Figure 6 represents a patient currently in a maxillary screw-retained fixed and bar-supported hybrid denture. This patient was a one-pack-a-day smoker and had severe periodontal disease and endodontic lesions for several years. The maxillary prosthesis was performing well, but the mandibular natural dentition had been deemed terminal. Consultation and examination revealed that a mandibular screw-retained prosthesis was not an option for the patient due to cost. The treatment alternative option chosen was scheduled serial extractions and immediate implant placement bilaterally in the No. 18, 20, 29, and 31 positions and in the anterior symphysis of the No. 24 to 25 region (Figure 7). An acrylic provisional treatment bridge supported by the remaining natural dentition (teeth Nos. 21, 22, 27, and 28) was fabricated at chairside, derived from a pretreatment diagnostic wax up. Four months were required to verify osseointegration of the immediately placed implants (Figure 8). After successful implant integration, a series of appointments were scheduled following traditional removable prosthetic principles to develop a removable immediate complete overdenture retained by prefabricated attachments. The definitive restoration and attachments were cold-cured intraorally. The patient was evaluated at 1 week, 3 weeks, and 3 months. To increase the stability and long-term goal of this prosthesis, the removable overdenture was reinforced by a milled metal bar for rigidity (Figure 9).
This technique requires additional provisionalization and patient commitment. Oral hygiene and improvement of lifestyle habits are critical considerations in affecting the outcome and maintenance of this treatment option. The patient committed to the cessation of smoking request to optimize osseointegration and oral hygiene health. By working closely with the laboratory and the patient, the patient's expectations and satisfaction requirements were met functionally and esthetically (Figure 10). The occlusal balancing of bite forces allowed a shortened adaptation from her terminal dentition to the new prosthesis. Bilateral occlusal equilibration should be the standard of care.14 Moreover, the occlusion should be checked as part of a re-care/wellness visit yearly.
Implant- and Bar-Supported Removable Complete Dentures (O-ring Ball Attachments)
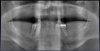
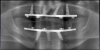
Removable prosthetics, implant dentistry, and 3D technology with cone-beam computed tomography (CBCT)/treatment-planning software have made dentistry more creative, predictable, and exciting for both the patient and practitioner.16 As shown in Figure 11, a panoramic radiograph revealed severe periodontal disease and terminal natural dentition. An option for another set of maxillary and mandibular immovable partial dentures would likely be a short-term solution and not meet the functional and esthetic requests of the patient. The patient was offered traditional removable complete maxillary and mandibular dentures, implant- and bar-supported complete removable dentures, or complete maxillary and mandibular fixed hybrid or zirconia bridges.
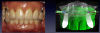
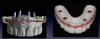
After analog polyvinyl impressions, bite blocks, and esthetic setups were completed, the entire case was developed digitally through CBCT and treatment-planning software (Figure 12 and Figure 13). 3D-printed of surgical guides and prostheses were fabricated before the surgical appointment. Using oral sedation and local anesthetic, the patient had his remaining natural dentition removed, followed by bone reduction, osteotomies, implant placement, and restorative connections; then the bar was placed and was ready to receive the prostheses with the o-ring ball attachment assembly (Figure 14 and Figure 15).
The patient adapted well to the new prostheses. The 4-month postoperative panoramic radiograph showed healthy maturing bone, and a clinical examination demonstrated osseointegration of all implants (Figure 16). Throughout the entire healing process, the patient was seen at 1 week, 3 weeks, and 3 months for occlusal evaluation with bite force balancing, phonetics, and esthetics (Figure 17).
Fixed Screw-Retained Prosthesis
A sophisticated and technologically innovative alternative to rejuvenating a terminal smile and providing a more youthful and natural smile is a complete full-arch fixed screw-retained bridge. The mature-age population that most represents the request for fixed alternative treatment options is the 55- to 75-year-old group17 (Figure 18). Socioeconomics and demographics in any region dictate which alternative is chosen.18 If the patient is determined to have a smile retained in the mouth like the natural dentition, is psychologically prepared to have this procedure, has the resources to afford the therapy, and is committed to oral hygiene care, a 3D digital approach to develop the smile is an alternative, with state-of-the-art technology and materials. Figure 19 shows a digitally designed surgical guide, with implant and restorative elements placed after extractions and bone reduction. The prosthesis can be immediately attached (provided initial stabilization torque values are greater than 35 Ncm).19 As shown in Figure 20, the patient was dismissed with a fixed prosthesis. Osseointegration was to be evaluated over 12 to 16 weeks, and then the final zirconia prosthesis would be fabricated.
Conclusion
Edentulism interferes with a patient's quality of life.Decision-making on treatment for the edentulous population should consider affordability, comfort, esthetics, and maintenance of the prosthesis. Complete dentures with the appropriate vertical dimension and bite-force balance allow the patient to progressively adapt over time. Edentulous patients want to attend events, be confident with their smile, look more youthful, and trust that their partner or spouse is attracted to them.
Socioeconomics and demographics have an impact on what a patient chooses to do or not do (ie, delay treatment). The duty and responsibility of the oral practitioner is to create a relationship with the patient who seeks guidance to improve and optimize oral health.
Alternative treatment options come at a cost that often does not fit the budget of the edentulous patient. An understanding of the patient's desires and reasonable means to obtain therapy is the starting point to develop a treatment that may provide traditional removable prosthetic dental restorations, such as complete dentures, removable implant-supported complete dentures, or sophisticated and highly esthetic prosthetics at a premium cost.
About the Author
Thomas M. Bilski, DDS
Private Practice
Independence, Ohio
References
1.Schwendicke F, Meyer-Lueckel H, Stolpe M, et al. Costs and effectiveness of treatment alternatives for proximal caries lesions. PLoS One. 2014;9(1):e86992.
2.Nimako-Boateng J, Owusu-Antwi M, Nortey P. Factors affecting dental diseases presenting at the University of Ghana Hospital. Springerplus. 2016;5(1):1709.
3.Andrews JM.The philosophy of disease eradication. Am J Public Health Nations Health. 1963;53(1):1-6.
4. Nordqvist C. Everything you need to know about dry mouth. Medical News Today. https://www.medicalnewstoday.com/articles/187640.php. Updated January 2, 2018. Accessed March 28, 2019.
5.Li X,Kolltveit KM, Tronstad L, Olsen I. Systemic diseases caused by oral infection. Clin Microbiol Rev. 2000;13(4): 547-558.
6. Emami E, de Souza RF, Kabawat M, Feine JS. The impact of edentulism on oral and general health. Int J Dent. 2013;2013:498305. doi: 10.1155/2013/498305.
7. Kuć J, Sierpińska T, Gołębiewska M. Evaluation of functional parameters in the occlusion of complete denture wearers before and after prosthetic treatment. J Prosthodont Res. 2017;61(4):480-490.
8. McCunniff M, Liu W, Dawson D, Marchini L. Patients' esthetic expectations and satisfaction with complete dentures. J Prosthet Dent. 2017;118(2):159-165.
9. Mohamad Rasidi MQZ. Review on history of complete denture. Res J Pharm Tech. 2016;9(8):1303-1306.
10. Burns J. Animal teeth, wood, and porcelain: how the first dentures were made. Gizmodo. https://gizmodo.com/animal-teeth-wood-and-porcelain-how-the-first-dentur-1831338161. Published January 4, 2019. Accessed March 28, 2019.
11. Waterloo and its dental legacy. Br Dent J. 2015;
218(12):666.
12. Khindria SK, Mittal S, Sukhija U. Evolution of denture base materials. J Indian Prosthodont Soc. 2009;9(2):64-69.
13. Haas M. The relationship between expectations and satisfaction: a qualitative study of patients' experiences of surgery for gynaecological cancer. Health Expect. 1999;2(1):51-60.
14. Tiwari B, Ladha K, Lalit A, Dwarakananda Naik B. Occlusal concepts in full mouth rehabilitation: an overview. J Indian Prosthodont Soc. 2014;14(4):344-351.
15. Pan YH, Lin TM, Liang CH. Comparison of patient's satisfaction with implant-supported mandibular overdentures and complete dentures. Biomed J. 2014;37(3):156-162.
16. Kumar M, Shanavas M, Sidappa A, Kiran M. Cone beam computed tomography - know its secrets. J Int Oral Health. 2015;7(2): 64-68.
17. Ettinger RL. Treatment planning concepts for the ageing patient. Aust Dent J. 2015;60:(suppl 1):71-85.
18. Patrick DL, Lee RSY, Nucci M, et al. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;6(suppl 1):S4.
19. Javed F, Ahmed HB, Crespi R, Romanos GE. Role of primary stability for successful osseointegration of dental implants: factors of influence and evaluation. Interv Med Appl Sci. 2013;5(4):162-167.