You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
An estimated 178 million Americans are missing at least one tooth, and approximately 40 million Americans are missing all teeth.1 Dentists are constantly searching for the best methods to provide esthetic and durable prostheses to their patients. The clinical decision as to which retention system best suits the individual patient depends on several factors. These factors include the individual indication, esthetics, retrievability, advantages and disadvantages of the different retention mechanisms, the retention provided, and clinical performance, including failures and complications. Recent technological innovations in implant dentistry have the potential to change how retention is achieved.
Traditionally, when it comes to implant restorations, the two main options are to cement a restoration or to screw it down (Figure 1). Now there is a third option that is cement-free and screwless. This new technology combines the esthetic benefits of cemented restorations with the ease of removable screw restorations. Some companies now offer this cement-less and screwless technology; product examples will be discussed later in this article.
Traditional Options for Retaining Implant Restorations
First, however, this article will review the advantages and disadvantages of cement and screw restorations. The topic of screw-retained versus cemented implant restorations has been debated by many authors. Factors affected by different methods of retention of the prostheses to the implants include ease of fabrication, cost, esthetics, access, occlusion, retention, incidence of loss of retention, retrievability, passivity of fit, restriction of implant position, effect on peri-implant tissue health, immediate fracture, and clinical performance.2 Whether cemented or screwed restorations are best remains undecided and controversial among practitioners. The choice of retention seems to primarily depend on the clinician's personal preference.3 Although literature on this topic does not provide definitive evidence regarding which method is superior, it is known that cementing is more popular. In dental offices across the country, 65% to 70% of restorations are cemented and 35% to 40% are screw retained. Cement restorations are more popular because of the simpler control of occlusion, versatility in esthetics, and elimination of screw-access holes.4-6 One major drawback with cemented restorations is the possibility of leaving excess cement in the peri-implant tissue.7 Excess cement left behind inadvertently is a chief concern that can result in soft-tissue damage, bone loss, and chronic inflammation.8 In a 2006 study, soft tissue surrounding screw-retained implant crowns was found to be healthier than soft tissue surrounding cemented restorations.9To help address this issue, custom abutments can now be designed with supragingival margins that facilitate simple and complete cement removal.
Screw-retained implant restorations enable a retrieval that allows effortless inspection of underlying components. Retrievability of implant restorations can provide simple solutions to problematic situations, such as food packing from opened proximal contact, unstable occlusion from porcelain fracture, and discomfort in chewing from loosened abutment screws. However, in practice, screw retrieval is typically only performed to repair damaged or fractured components because screw removal, reinsertion, and restoration of occlusal holes can be time-consuming.10 For some practitioners, the predictable retrievability of screwed implant crowns outweighs the initial high fabrication cost by decreasing the repair cost when biologic and technical complications occur.11 In addition to higher laboratory cost, disadvantages of screwed implant prostheses include esthetic and structural screw-hole concerns, as well as a relative lack of passive fit.7,12 Furthermore, the composite resin materials covering the screw-access holes are prone to wear and do not offer stable control over occlusion.13,14
According to a study that assessed the 5-year survival rates and incidences of complications for both cemented and screw-retained implants, neither method was clearly advantageous over the other. The study found cemented reconstructions exhibited more serious biologic complications, including implant loss and bone loss of greater than 2 mm. However, screw-retained reconstructions exhibited more technical concerns. The study also found that screw-retained reconstructions were more easily retrievable than cemented reconstructions, and therefore, technical and eventually biologic complications could be treated more easily. For this reason and for their apparently higher biologic compatibility, according to Stevens et al, screw-retained reconstructions seemed to be preferable over time compared with cemented restorations.15
However, many clinicians find screw-retained restorations more technically problematic than cement. The most frequently cited complications of screw-retained implants include prosthetic screw loosening, fracture, and failure of the prosthetic materials.16-18 In addition to providing better control over occlusion, cement enables improved anterior esthetics and permits a restoration when implant angulation would place the access hole on the labial surface.19 With cement, a passive fit for multiunit prostheses becomes less critical because the cement fills in the misfit regions between the abutment and the restoration.20 Abutment height is an important factor for proper retention and resistance of cemented restorations. Longer abutment walls will have more surface area and thus higher retentiveness. At least 5 mm of abutment height is needed for proper retention and resistance of cement-retained crowns.8
The length of the abutment wall also plays an important role in the resistance to tipping forces. To prevent tipping forces from dislodging the cemented restoration, the length of the abutment wall must be great enough to interfere with the arc of the casting, pivoting about a point on the margin on the opposite side of the restoration.20
Contrary to the aforementioned study, other studies have found that cement-retained, fixed implant-supported restorations show less marginal bone loss than screw-retained. One such study, a meta-analysis of studies from 1995 to 2015, with the follow-up periods ranging from 12 to 180 months, found the mean difference for marginal bone loss showed statistically significant differences in favor of the cement-retained prosthesis, and the implant survival rate was higher for the cement-retained prosthesis. However, the small difference between the mean values may not show clinical significance.21 These differing results show the difficulty in reaching consensus over screw- versus cement-retained restorations; both options have disadvantages.
Other Options for Retaining Implant Restorations
There are now alternatives to both cement and screws to retain prostheses. The advantages of the new cement-less, screwless restoration techniques include precise marginal adaptation with a cement-less interface, a bacterially sealed implant-abutment connection, a crown material with a similar wear rate and hardness value to human enamel, a simple laboratory method, and a reduced number of prosthetic components.11
The Bicon® dental implant (bicon.com) is a screwless implant system that connects the implant and implant-abutment unit with a 3.0° locking taper. A high clamping force between abutment and implant is generated through elastic deformation of both parts. During engagement, the high friction force resulting from the relative slip between the friction surfaces yields high contact forces. This interaction results in the surface oxide layers breaking down and the asperities fusing, commonly referred to as cold welding.22
The Integrated Abutment Crown™ (IAC) (Bicon) is a technique for the fabrication of single-tooth implant-supported crowns where the abutment and the crown are one chemo-mechanically bonded unit.23 The abutment-crown complex is connected to the implant with a locking taper. The clinical outcome of screwless and cement-less systems for single implant restorations compares favorably with the experience of screw and cement retained single and multiple implant restorations.24
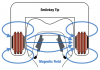
Smileloc® (Rodo, rodomedical.com) is another screwless, cement-less, retrievable abutment system. The Smileloc, combined with the proprietary Rodo abutment and coping, uses the shape memory material nickel titanium to create an entirely new attachment between a restoration and a dental implant (Figure 2). This abutment system offers retrievability by replacing the cement layer with a precision-engineered nickel-titanium sleeve that switches between shapes that lock and unlock the prosthesis when induction (electromagnetic) energy is applied.25 This implant retention technology was developed to combine the advantages of screw and cement technology while eliminating the disadvantages of composite resins and residual cement. The technology consists of a precision-machined abutment that fits onto most commercial dental-implant fixtures. It can be used in conjunction with compatible implant systems in the upper and lower jaw to retain crowns, bridges, and overdentures. The abutment accepts a shape memory sleeve that features two sets of movable flaps that switch between the "engaged" and "disengaged" positions to lock and unlock the restoration (Figure 3).20 The inner flaps of the sleeve engage with the abutment undercut. When a crown is inserted over the sleeve, the outer flaps engage the coping undercuts, thus connecting the abutment, sleeve, and coping into one mechanically interlocking system. The restoration must be seated properly to ensure the flaps engage.
Figure 4 through Figure 6 show the intraoral Smilekey® (Rodo) and how it works. Figure 7 through Figure 11 show a case restored using this system. An edentulous site at tooth No. 19 was prepared and an implant was placed. The veneering overlay and dental implant framework were designed using digital data from the intraoral scan defining the appropriate tooth contours, gingiva contours, and implant locations (Figure 7). The veneering overlay duplicates the anatomy provided in the digital data, defining the appropriate tooth position and gingival contours of the final prosthesis.26 The memory metal sleeve is shown in place on the abutment in Figure 8. The restoration was seated (Figure 9) and locked into place with no holes, no cement, and no screws. Figure 10 and Figure 11 depict the final result. To remove the crown for hygiene purposes or whatever need may arise, electromagnetic energy is provided by the hand-held intraoral induction device to the restoration coping sleeve complex; this returns all flaps to the disengaged position, thus freeing the crown, sleeve, and abutment from the undercuts.20
Conclusion
Implant dentistry is evolving to meet the high demands of various challenging clinical scenarios. A variety of abutment designs and material are now available. The decision on which methods and materials to use is based on the patient's individual situation and the clinician's personal preference. New technology may provide an appealing alternative to classic cemented and screw-retained restorations.
References
1. Bidra A, Wu J. Talking points: missing teeth. American College of Prosthodontists. https://www.prosthodontics.org/assets/1/7/ACP_Talking_points_for_Missing_Teeth_1-12-15.pdf. Accessed November 6, 2018.
2. Shadid R, Sadaqa N. A comparison between screw- and cement-retained implant prostheses. A literature review. J Oral Implantol. 2012;38(3):298-307.
3. Vigolo P, Mutinelli S, Givani A, Stellini E. Cemented versus screw-retained implant-supported single-tooth crowns: a 10-year randomised controlled trial. Eur J Oral Implantol. 2012;5(4):355-364.
4.Gervais MJ, Wilson PR. A rationale for retrievability of fixed, implant-supported prostheses: a complication-based analysis. Int J Prosthodont. 2007;20(1):13-24.
5. Chee W, Felton DA, Johnson PF, Sullivan DY. Cemented versus screw-retained implant prostheses: Which is better? Int J Oral Maxillofac Implants. 1999;14(1):137-141.
6. Freitas AC Jr, Bonfante EA, Rocha EP, et al. Effect of implant connection and restoration design (screwed vs. cemented) in reliability and failure modes of anterior crowns. Eur J Oral Sci. 2011;119(4):323-330.
7.Guichet DL, Caputo AA, Choi H, Sorensen JA. Passivity of fit and marginal opening in screw- or cement-retained implant fixed partial denture designs. Int J Oral Maxillofac Implants. 2000;15(2):239-246.
8. Campbell W, Herman MW. Choosing between screw-retained and cement-retained implant crowns. Inclusive Magazine. 2011;2(2):20-26.
9. Weber HP, Kim DM, Ng MW, et al. Peri-implant soft-tissue health surrounding cement- and screw-retained implant restorations: a multi-center, 3-year prospective study. Clin Oral Implants Res. 2006;17(4):375-379.
10. Rajan M, Gunaseelan R. Fabrication of a cement- and screw-retained implant prosthesis. J Prosthet Dent. 2004;92(6):578-580.
11. Kim S-Gy, Chung C-H, Son M-K. Effect of cement washout on loosening of abutment screws and vice versa in screw- and cement-retained implant-supported dental
prosthesis. J Adv Prosthodont. 2015;7(3):207-213.
12. Keith SE, Miller BH, Woody RD, Higginbottom FL. Marginal discrepancy of screw-retained and cemented metal-ceramic crowns on implants abutments. Int J Oral Maxillofac Implants. 1999;14(3):369-378.
13. Beumer J, Faulkner RF, Shah KC, Moy PK. Fundamentals of Implant Dentistry: Prosthodontic Principles. Hanover Park, IL: Quintessence Publishing, 2015;1:201-226.
14. Zinner ID, Panno FV, Small SA, Landa LS. Implant Dentistry: From Failure to Success. Hanover Park, IL: Quintessence Publishing, 2003;1:96-97.
15. Stevens PJ, Fredrickson PJ, Gress ML. Implant Prosthodontics: Clinical and Laboratory Procedures. St. Louis, MO: Mosby, 1999;2:10.
16. Sailer IS, Mühlemann S, Zwahlen M, et al. Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. Clin Oral Implants Res. 2012;23(suppl 6):163-201.
17.Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90(2):121-132.
18. Goodacre CJ, Kan JY, Rungcharassaeng K. Clinical complications of osseointegrated implants. J Prosthet Dent. 1999;81(5):537-552.
19. Watanabe F, Uno Y, Hata Y, et al. Analysis of stress distribution in a screw-retained implant prosthesis. Int J Oral Maxillofac Implants. 2000;15(2):209-218.
20. Shah KC, Young SR, Wu BM. Clinical application of a shape memory implant abutment system. J Prosthet Dent. 2017;117(1):8-12.
21. Shillingburg HT, Hobo S, Whitsett LD. Fundamentals of Fixed Prosthodontics. 2nd ed. Chicago, IL: Quintessence; 1981:79-96.
22. Khraisat A, Jebreen SE, Baqain ZH, et al. Multicenter retrospective study of cement-retained implant-supported anterior partial prostheses: success and restoration evaluation. Int J Oral Maxillofac Implants. 2008;23(4):705-708.
23. Urdaneta RA, Marincola M. The Integrated Abutment Crown, a screwless and cementless restoration for single-tooth implants: a report on a new technique. J Prosthodont. 2007;16(4):311-318.
24. Keating K. Connecting abutments to dental implants: an engineer's perspective. Irish Dent. 2001;43-46.
25. Urdaneta A, Marincola M, Weed M, Chuang S-K. A screwless and cementless technique for the restoration of single-tooth implants: a retrospective cohort study. J Prosthodont. 2008;17(7):562-571.
26. Schulter D, Schulter C, Fraysur K, et al. Overdenture and dental implant framework. Patent Application US20180250102A1.