You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Lasers are frequently used in the dental setting and are changing the way many clinicians practice dentistry today because laser treatments offer convenient, precise, effective, and efficient treatment options for dentists and specialists. They are used in periodontal, cosmetic, restorative, and other procedures. Dental lasers also have their place in dental hygiene procedures. This article will briefly examine the history and fundamentals of lasers, provide essential safety information, and describe how lasers are used in dentistry and dental hygiene.
History and Fundamentals of Lasers
Several historical figures contributed to the development of lasers, beginning with Niels Bohr, a Nobel prize-winning Danish physicist who made fundamental contributions to understanding atomic structure and quantum theory.1,2 Another contributor was Albert Einstein; Einstein developed the quantum theory of light, which stated that light or photons consist of both waves and particles and that photons travel around in wavelike patterns, suggesting the concept of stimulated amplified emission of light.2,3 His theories were used for the formation of the laser acronym, which stood for light amplification by stimulated emission of radiation.2,3 Finally, Theodore Maiman created the first laser by inserting a ruby rod into a photographic flash lamp in 1960; the ruby laser was used for research and clinical applications. However, due to issues with scattering the laser beam to adjacent teeth, laser use was delayed in dentistry until the 1980s, when the first CO2 laser was created, followed by the Nd:YAG in 1987, the first diode in 1996, and the Er:YAG in 1997.4,5
Laser light is produced when an excited atom becomes stimulated and emits a photon generating a focused, concentrated monochromatic ray of light. Laser light allows a directed effect on the target tissue at a much lower energy level than would be achieved with natural light.5 This form of energy behaves both like a wave and a particle. Photons are reflected back and forth within an active medium to enhance the stimulated emission. The power increases with each successive pass, creating electromagnetic energy, a kind of radiation. Most dental lasers used today fall within the infrared zone and are non-ionizing, which means they do not have enough energy to remove electrons from atoms.5 A laser light is organized and has just one wavelength, which is key to understanding the fundamentals of lasers. Not all lasers used in dentistry have the same wavelength.5 Increasing the wavelength allows the laser energy to penetrate tissue more deeply.
Lasers in Dentistry
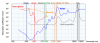
Lasers are used for both hard and soft tissue in dentistry (Figure 1). In endodontics and periodontics, lasers can be used for bacterial reduction, and soft lasers are used for photobiomodulation. It is helpful to understand how laser energy works in that light is attracted to chromophores, which contain water and protein. Lasers interact with tissue in four ways. The first is through transmission, where the laser simply passes through the tissue and nothing happens. Next is dispersion, where the light may disperse or scatter to an unintended area or tissue. Reflection is another interaction, where the light reflects as it would on a mirror, and nothing happens. Then there is absorption, the type that is used in dental procedures. Not all objects absorb wavelengths in the same manner, so it is important to consider the target when using lasers in dentistry, such as enamel, dentin, bone, or pulp. The laser absorption curves are shown in Figure 2. Each type of laser used in dentistry has a different wavelength, and the attraction that each specific laser has to hemoglobin, melanin, and hydroxyapatite will vary accordingly.
Tissue Sources
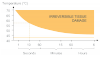
The water content of different tissue will affect the laser's ability when a dental procedure is performed. For example, more power is required for tissue that has less water, such as fibrous tissue. When using a laser on tissue, the type of the tissue is important; granulation and normal tissue will not need as much power due to their higher water content compared with fibrous tissue. The amount of tissue that will be removed depends on the type of tissue. To avoid irreversible damage, the effect of time and temperature of laser exposure on the tissue must be considered (Figure 3). Safety concerns must also be taken into account.
Safety
Laser safety education must be compliant with the American National Standards Institute (ANSI), which provides approved standards for proper laser operation, including the scope and requirements for laser safety, classifications, measurement standards, and hazard evaluation, among other aspects.6 Other important considerations include exposure of the eyes or skin and personal protective equipment for the laser operator, labels, and the need to have a laser safety officer on the premises at the dental practice.6
Lasers are divided into four hazard classes along with their subdivisions, based on exposure times, wavelength, average power, and total energy (Table 1). ANSI also specifies requirements for laser operation, based on the laser's classification-specific training, control measures, a laser safety officer, and engineering controls. Dental lasers are class 4, which means that all the aforementioned requirements must be met if lasers are used in a practice. There are also required labels that state the wavelength and maximum power on class 3 and 4 lasers, along with the potential danger and classification of each laser.
During normal operation, the nominal hazard zone is the area where the level of direct, reflected, or scattered radiation occurs that can pose a risk to the skin and eyes. It is important to wear proper safety equipment, including safety eyewear specific to the laser being used, because unintended contact with the laser beam can cause injuries to the cornea and retina. There are also respiratory concerns due to the laser plume, or airborne laser contaminants; therefore, high-volume evacuation to remove the plume is recommended. Wearing a safety mask is also important because the laser plume could potentially contain strains of human papilloma virus when the tissue is ablated or vaporized.
A final safety factor is that alcohol poses a fire hazard; therefore, no alcohol or combustible material should interact with a laser beam. Alcohol wipes may never be used to remove debris or coagulum from the fiber of the laser; instead, using a 2 x 2 gauze with water is recommended. Nitrous oxide may be used, but it requires the correct scavenging devices.
Infection Control
The Centers for Disease Control and Prevention (CDC) has published recommendations for infection control in dentistry; the guidelines apply to the use of dental lasers as well. According to the CDC, a high-filtration surgical mask and possibly a full-face shield should be used. For minimal laser plumes, a practice will need a central room suction unit with in-line filters, but for substantial laser plumes, a dedicated smoke exhaust system with high-efficiency filters is necessary.7,8
Fibers and handpieces must be autoclaved between each patient, including spools of fibers. Disposable tips, fibers, or cannulas must be discarded properly in a biohazard container after use on each patient. Bending tools and fiber cutters should also be autoclaved if contaminated. The laser unit can be wiped with a disinfectant wipe approved by the Environmental Protection Agency.7,8
How Dentists and Dental Hygienists Use Lasers
The lasers used in dentistry include diode, CO2, Nd:YAG, and Er:YAG. Dental hygienists typically use diode lasers, which incorporate a solid-state semiconductor. Diode lasers9:
• are better for soft tissue management
• can be used by both dentists and hygienists
• offer precise laser ablation and better wound healing with less swelling
• typically result in less bleeding and a reduced amount of infection for laser procedures
• protect healthy tissue
Lasers have multiple functions in dentistry, including surgical, or cutting and excising tissue; decontamination, or hygiene; and photobiomodulation, which is a benefit that makes lasers unique-this cannot be achieved with any other tool or equipment in a dental practice.
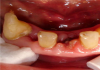
During procedures such as a frenectomy or frenulectomy (tongue-tie release), the dentist uses an ablation process, which requires a back-and-forth motion similar to a sawing motion or using a pencil eraser. Patients often experience minimal to no pain, and often no anesthetic is required, with little to no bleeding. A slower movement of the laser will result in a faster cut to the tissue-one must be trained to perform this technique. Diode lasers are also suitable for biopsies, cosmetic contouring after orthodontics, restorative procedures, and periodontal procedures. Precision is important for these types of procedures for control of bleeding, and the laser also allows the dentist to see the result during the procedure (Figure 4).10
Figure 5 shows a laser being used in a periodontal procedure, in which the fibers went into the gingival pocket and performed the decontamination. Minimal bleeding occurred, and the tissue looked relatively healthy immediately after the procedure. At the follow-up appointment, there was no inflammation or infection, and the area did not require sutures (Figure 6). This procedure is a good example of how dental lasers are used.
Photobiomodulation, also known as low-level laser therapy, soft-tissue laser therapy, or cold laser therapy, is another procedure that can only be accomplished with a laser using light, or photon energy. The laser is applied to tissue on a non-thermal setting, and the light crosses the skin barrier, where it is absorbed into cells. The laser light initiates physiologic reactions in diseased and damaged tissue, creating energy and stimulating cells to accelerate wound healing and tissue regeneration. This therapy has medical applications and is also used in dentistry for reducing inflammation and edema, reducing periodontal and postoperative pain, enhancing healing and tissue repair, dentinal desensitization, oral mucositis, and temporomandibular joint disorder, among other uses.11
Figure 7 and Figure 8 show a patient who received an extraction with and without a laser. The photobiomodulation performed with the laser (Figure 7) shows accelerated healing, and the patient experienced reduced discomfort.
State Regulations and Medical/Legal Considerations
In addition to allowing dentists to use lasers, many states allow laser use by dental hygienists; however, many states also have a written policy on the specific education and training required for dental hygienists to perform laser procedures. Some states require more hours and training than other states; it is the responsibility of the clinician to understand their individual state board regulations.12
There are medical/legal considerations for both dentists and hygienists when a laser is added to a practice. Conservative soft-tissue surgery, for example, is considered within the scope of accepted dental practice and is a covered procedure under most professional liability insurance policies. However, the clinician/practice owner must research the requirements and what is covered for laser procedures under an individual insurance policy.
Summary
There are many benefits to using a laser in a dental practice; lasers are less invasive and more precise, therefore preserving healthy tissue. They offer not only better procedural outcomes but also increase patient satisfaction with little to no pain and bleeding. Because laser procedures reduce discomfort during treatment, they minimize or eliminate the need for anesthesia in many procedures. Although the requirements for training, safety, infection control, and state regulations require some effort for the practice owner/dentist and hygienists as well as the rest of the dental team, the benefits for patients and the practice are worth the effort if the goal is to deliver the best possible patient care.
References
1. Niels Bohr biographical. The Nobel Prize. https://www.nobelprize.org/prizes/physics/1922/bohr/biographical/. Accessed November 1, 2018.
2. The dual nature of light as reflected in the Nobel archives. The Nobel Prize. https://www.nobelprize.org/prizes/themes/the-dual-nature-of-light-as-reflected-in-the-nobel-archives/. Accessed November 1, 2018.
3. Albert Einstein biographical. The Nobel Prize. https://www.nobelprize.org/prizes/physics/1921/einstein/biographical/. Accessed November 1, 2018.
4. Theodore Maiman. American Physical Society. https://www.aps.org/programs/outreach/history/historicsites/maiman.cfm. Accessed November 1, 2018.
5. Parker S. Verifiable CPD paper: introduction, history of lasers and laser light production. Br Dent J. 2007;202(1):21-31.
6. American National Standards Institute - Z136.1 safe use of lasers. Laser Institute of America. https://www.lia.org/resources/laser-safety-information/laser-safety-standards/ansi-z136-standards/z136-1. Accessed November 1, 2018.
7. Guidelines for infection control in dental health-care settings-2003. MMWR Recomm Rep. 2003;52(RR-17):1-61.
8. Summary of infection prevention practices in dental settings: basic expectations for safe care. Centers for Disease Control and Prevention. https://www.cdc.gov/oralhealth/infectioncontrol/guidelines/. Accessed November 1, 2018.
9. Derikvand N, Chinipardaz Z, Ghasemi S, Chiniforush N. The versatility of 980 nm diode laser in dentistry: a case series. J Lasers Med Sci. 2016;7(3):205-208.
10. Verma SK, Maheshwari S, Singh RK, Chaudhari PK. Laser in dentistry: an innovative tool in modern dental practice. Natl J Maxillofac Surg. 2012;3(2):124-132.
11. Hamblin MR. Photobiomodulation or low-level laser therapy. J Biophotonics. 2016;9(11-12):1122-1124.
12. State by state quick reference chart on laser use by dental hygienists. Academy of Laser Dentistry. http://www.laserdentistry.org/uploads/files/Reg%20Affairs/Regulatory%20Chart%20ALL%204_2018%20-%20ALL%20STATES.pdf. Accessed November 1, 2018.