You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The proliferation of resin composites and adhesive systems has met the increasing demand for esthetic restorations in both anterior and posterior teeth.1 Depending on the respective clinical indication, resin composite materials are suitable for both direct and indirect restorations.2 Although direct resin composites have replaced other restorative options, there are a number of issues associated with their use in the posterior region. These include: high polymerization shrinkage; gap formation; poor resistance to wear and tear; color instability; and insufficient mechanical properties.3 Direct restorations can result in contact area instability, difficulty in generating proximal contour and contact, lack of marginal integrity, and postoperative sensitivity.4 All of these factors impact the longevity and clinical success of restorations.5-7 Despite efforts to reduce the issue of marginal infiltration associated with direct techniques, to date, no method has produced acceptable results.8,9
Posterior indirect restorations are widely used in modern restorative dentistry to overcome the problems resulting from direct techniques.2 The adhesive concepts that have been used for direct restorative procedures are now being applied to indirect restorations and have been incorporated into daily practice.10 Indirect composites offer an esthetic alternative to ceramics for posterior teeth.10,11 The clinical performance of composite resin restorations is comparable to ceramic restorations, but the relatively low cost associated with composites has resulted in increased use of composite resin-based indirect restorations in the posterior region.12-14 Ceramic materials exhibit a very high elastic modulus, thus they cannot absorb most of the occlusal forces. Since polymeric materials absorb a significant amount of occlusal stress, they should be considered the material of choice.10,15
The success of adhesive restorations depends primarily upon the luting agent and adhesive system.16 Several authors investigated the properties of resin luting materials such as bond strength, degree of conversion, and wear, in order to predict their clinical behavior.17-22 Among the parameters that may influence the clinical success of indirect restorations is a proper degree of polymerization of the resin luting agent, which should be taken into account.23 Moreover, successful adhesion depends on proper treatment of the internal surfaces of the restoration as well as the dentinal surface.2,16
This article discusses materials and techniques used in adhesive cementation for indirect composite resin restorations.
The Adhesive Systems A Historical Overview
Because the microscopic structure of two different contact surfaces presents irregularities, an adherent is necessary. The introduction of adhesive materials as alternatives to traditional retentive techniques has greatly revolutionized restorative dentistry.24 In the development of dental adhesives, the ultimate goal is to achieve strong, durable adhesion to dental hard tissues.25 In 1955, Buonocore showed how the treatment of enamel with phosphoric acid increases the exposed enamel surface by producing micro-irregularities on it, resulting in improved adhesion potential. The modern concept of enamel bonding can be traced to his published findings.26
In 1965, Bowen formulated the first generation of dentinal adhesive.27 The increasing interest in adhesion in dentistry led to the development of four generations of adhesive systems, with the 4th generation achieving good results for dentin bonding in the 1990s.28
Modern Adhesive Systems
The modern formulation of an enamel-dentin adhesive system includes the following three components29:
Etchant—an organic acid with the function of demineralizing the surface, dissolving hydroxyapatite crystals, and increasing free surface energy.
Primer—an amphiphilic compound that increases the wettability of the hydrophilic substrate (dentin) to a hydrophobic agent (bonding or resin).
Bonding agent—a fluid resin used to penetrate the etched and primed substrate and, after curing, to create a real and stable adhesive bond.
In order to obtain an optimal infiltration of enamel and dentin substrates, the ideal features of an adhesive material are: low viscosity; high superficial tension; and effective wettability. The fundamental requisite is wettability, which depends on the intrinsic properties of fluid and dental substrate.30
The classification of the respective adhesive systems is based on their etching characteristics and the number of steps they require.31
Etch-and-Rinse Systems—The etch-and-rinse technique is characterized by the etching of the enamel and/or dentin with an acid agent (orthophosphoric acid at 35% to 37%), which needs to be subsequently washed away. The etch-and-rinse adhesive systems can be further classified into three-step and two-step systems. Three-step systems require separate etching, priming, and bonding. Two-step adhesives are instead characterized by an application of an etching compound and then an agent that combines a primer and a bonding. The etching application removes the smear plugs, demineralizes the dentin, and exposes the intertubular dentin collagen fibers, obtaining an ideal micromechanical anchor for the adhesive.32,33
Self-Etch Systems—Self-etch refers to an adhesive system that dissolves the smear layer and infiltrates it at the same time, without a separate etching step.31 The self-etch adhesives have been further classified into two-step systems and one-step systems, which simultaneously provide etching, priming, and bonding.34
Self-Adhesive Systems—In the past few years, new resin cements, so-called “self adhesives,” have been introduced. This particular resin cement needs only to be applied on tooth substrate, without any etching, priming, or bonding phases.35
Tooth Preparation
After caries and/or failed restoration removal, a cavity with slightly occlusal divergent walls (5° to 15°) and round internal angles is prepared by using decreasing grit (from 60–70 µm to 15–20 µm grit) cylindrical round-ended diamond burs. Preparation margins are not bevelled but prepared via butt joint.2 After cavity preparation and before cavity finishing, adhesive procedures are performed36 using a rubber dam in order to achieve an immediate dentin sealing.37,38 In keeping with rubber dam placement for subsequent restoration placement, the interproximal margin must be supragingival. To avoid a dual marginal leakage, no direct composite is used for gingival margin rebuilding.39 If any deep subgingival margin persists after cavity preparation—thus precluding proper rubber dam placement—the feasibility of a surgical crown-lengthening procedure and/or an orthodontic extrusion must be considered.40 A light-curing composite filling material is used to block out defect-related undercuts.2,41 The finishing phases are performed with diamond burs with a slight taper and with silicone points (Table 1). The teeth are protected with temporary eugenol-free restorations after impression making.42
Dentin Treatments
Research on adhesive systems is focused mainly on increasing bond strength and simplifying application. The application of phosphoric acid increases the surface energy of the dentin by removing the smear layer and promoting demineralization of surface hydroxyapatite crystals. The resin monomers, by means of the primer agent’s amphiphilic properties, infiltrate the water-filled spaces between collagen fibers, which results in a “hybrid layer” composed of collagen, resin, residual hydroxyapatite, and traces of water. It results in an ideal micromechanical anchor substrate for adhesive systems on dentin.16,43,44
Immediate dentin sealing (IDS) is a strategy in which a dentin bonding agent is applied to freshly cut dentin and polymerized before making an impression.45 The recommended technique focuses on the use of the “etch-and-rinse” systems. Etching should extend slightly over enamel to ensure the conditioning of the entire dentin surface. The use of either two-step or three-step dentin bonding agents is equally effective. Self-priming resins, however, generate a more excess resin layer, which may extend over the margin and require additional bur corrections. IDS can be immediately followed by the placement of composite in order to block out eventual undercuts and/or build up deep cavities, reducing restoration thickness and ensuring the light-cured polymerization of the luting agent. Finally, enamel margins are usually reprepared before final impression to remove excess adhesive resin and provide ideal taper.45
When the preparation exposes no dentinal areas—eg, in veneered indirect restorations—neither immediate dentin sealing nor primer agent applications are necessary, since the etching and bonding phases ensure an optimal bond for enamel adhesion.46 Immediate dentin sealing should be followed by air blocking and pumicing to generate ideal impressions.47 In-vitro studies have shown increased bond strength for IDS versus delayed dentin sealing (DDS) techniques.48-52 The IDS technique also eliminates any concerns regarding the film thickness of the dentin sealant and protects dentin against bacterial leakage and sensitivity during the provisional phase of treatment.45 Moreover, it was suggested that multiple adhesive coatings can improve the quality of resin-dentin bonds.53
Surface Treatments for Composite Restorations
Several techniques have been suggested for increasing bond strength, involving treating the internal surfaces of indirect restorations (Table 2).54,55 The surface treatments aim not only to achieve a high retentive bond strength of the restoration, but also to avoid any microbiological leakage.56 Composite surface treatments are necessary for adhesion of indirect composite restorations.57 Acid-etching with phosphoric acid, acidulated phosphate fluoride, or hydrofluoric (HF) acid is one of the treatments reported in literature.58-60
The internal surfaces of indirect restorations can be abraded with aluminium oxide, using an intraoral sandblasting device.58,59,61-63 Also, silane coupling agents are used as adhesion promoters.64,65 Another method, the tribochemical coating, forms a silica-modified surface as a result of airborne-particle abrasion with silicon dioxide (SiO2)-coated aluminium particles. The surface becomes chemically reactive to the resin by means of silane coupling agents.63,66,67
Many studies show that Er:YAG laser treatment enhances bond strength between composite and resin cement.68,69 Other studies demonstrate no influence of laser treatment on bond strength.67,70
Roughening the composite area of adhesion, sandblasting, or both sandblasting and silanizing can provide statistically significant additional resistance to tensile load. Acid-etching with silane treatment does not reveal significant changes in tensile bond strength. Sandblasting treatment is the main factor responsible in improving the retentive properties of indirect composite restorations.57
Cementation
Resin cements are divided into three groups according to polymerization process: chemically activated cements, light-cured cements, and dual-cured cements.16,71 Of the three, light-cured resin cements have the clinical advantages of longer working time and better color stability, but curing time, restoration thickness, and overlay material significantly influence the microhardness of the resin composites employed as luting agents.46,72
Dual-cured resin cements have the advantages of controlled working time and adequate polymerization in areas that are inaccessible to light. Conversely, they are relatively difficult to handle.23,73,74 Photoactivation increases the degree of conversion and surface hardness of dual-cured cements.75
Optimal luting of indirect restorations is dependent on the light source power, irradiation time, and dual-cure luting cement or light-curing composite chosen. Curing should be calibrated for each material to address high degrees of conversion. Preheating light-cured filled composites allows the materials to reach optimal fluidity.76-78 The suggested temperature for composite preheating is 39°C.79 The necessary working time for positioning the indirect restorations and removing the excess cement can be extended at the discretion of the clinician, using a light-curing composite as luting agent, thus overcoming the relatively restricted working time allowed by dual-cure cements.2
Total-etching of dentin substrate is recommended as the first step for the two- and three-step adhesive systems.80 To reduce the number of operative steps and to simplify the clinical procedures, self-etching adhesive systems, which do not require a separate acid-etching step, have been introduced.81 Literature reports demonstrate that multi-bottle systems with simultaneous etching and rinsing show superior in-vitro and in-vivo activities compared to the new all-in-one systems.44,82
The self-adhesive resins may be considered an alternative for luting indirect composite restorations onto non-pretreated dentin surfaces,83 even if bond strengths are lower than etch-and-rinse systems.84,85 The etch-and-rinse technique provides more reliable bonding compared to self-etch luting agents and self-adhesive luting agents when used to bond indirect composite restorations to dentin.22,86-88
The constant use of rubber dam isolation is necessary for the cementation protocol with adhesive systems. Removing residual cement using explorers, scalpels, and floss before complete polymerization, and a 15c scalpel after polymerization, is recommended in order to avoid compromising restoration marginal accuracy, compared to the use of burs, discs, or strips (Table 3).2
Discussion and Conclusions
Resin-based composites give predictable results in teeth restoration with respect to both mechanical and esthetic properties when they are used as indirect restoration materials.2 Indirect composites make it possible to overcome some shortcomings of direct techniques. Indirect restorations—ie, those created outside of the mouth—result in better proximal and occlusal contacts, better wear and marginal leakage resistance, and enhancement of mechanical properties compared to direct techniques.6,85
Since the dentin substrate has a high organic content, tubular structure variations, and the presence of outward fluid movement, bonding to dentin is a less reliable technique when compared to enamel bonding.89,90 Bonding composite restorations to tooth structure involves the dentin/adhesive-cement interface and composite restorations/cement interface.22
Each step of the clinical and laboratory procedures can have an impact on the esthetic results and longevity of indirect restorations.91 Cementation is the most critical step and involves the application of both the adhesive system and resin luting agent.92,93 An appropriate treatment of the fitting surface of the resin composite restoration and dentin substrate is necessary to establish a strong and durable bond.57
It is recommended that the freshly cut dentin surfaces be sealed with a dentin bonding agent immediately following tooth preparation, before taking impression.45 Immediate dentin sealing results in a high bond strength for total-etch and self-etch adhesives; however, the microleakage is similar to that with conventional cementation techniques.49
When following a protocol of cementation using an adhesive system, constant rubber dam isolation and careful hand finishing are necessary to provide predictable clinical results (Figure 1 through Figure 4).2
Supragingival margins facilitate impression making, definitive restoration placement, and detection of secondary caries.94 In addition, some studies have demonstrated that subgingival restorations are associated with higher levels of gingival bleeding, attachment loss, and gingival recession than supragingival restorations.95,96 Therefore, in all cases where rubber dam cannot be adequately placed, surgical crown lengthening or orthodontic extrusion should be taken into account. Otherwise, traditionally cemented restorations are preferable to the use of adhesive procedures.
Sandblasting of the composite surfaces has been recommended as a predictable means for enhancing the retention between resin cements and indirect composite restorations.57,97 The application of an appropriately selected adhesive material with proper technique will ensure predictable results and successful long-term clinical outcomes.
Modified United States Public Health Service criteria are the most complete and commonly used assessment techniques in clinical trials on indirect composite restorations.37,98
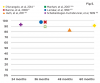
As shown in Figure 5, restorations were evaluated at baseline and after a follow-up period for secondary caries, marginal adaptation, marginal discoloration, color match, anatomic form, surface roughness, endodontic complications, fracture of the restoration, fracture of the tooth, and retention of the restoration.2,6,99-102 In many of the reported follow-up studies, indirect restorative procedures were carried out by dental students,99-102 and the main reasons for failures during the observation period seemed to be secondary caries, endodontic complications, and fractures.1,2
The literature sources support the clinical acceptability of indirect composite resin techniques regarding survival rate and esthetic outcomes at up to 10 years’ follow-up.1,103 Adhesive cementation is a complex procedure that requires knowledge of adhesive principles and adherence to the clinical protocol in order to obtain durable bonding between tooth structure and restorative material.
Disclosure
The authors had no disclosures to report.
References
1. Thordrup M, Isidor F, Hörsted-Bindslev P. A prospective clinical study of indirect and direct composite and ceramic inlays: ten-year results. Quintessence Int. 2006;37(2):139-144.
2. D’Arcangelo C, Zarow M, De Angelis F, et al. Five-year retrospective clinical study of indirect composite restorations luted with a light-cured composite in posterior teeth. Clin Oral Investig. 2014;18(2):615-624.
3. Manhart J, Kunzelmann KH, Chen HY, Hickel R. Mechanical properties and wear behavior of light-cured packable composite resins. Dent Mater. 2000;16(1):33-40.
4. Mendonça JS, Neto RG, Santiago SL, et al. Direct resin composite restorations versus indirect composite inlays: one-year results. J Contemp Dent Pract. 2010;11(3):25-32.
5. Geurtsen W. Biocompatibility of resin-modified filling materials. Crit Rev Oral Biol Med. 2000;11(3):333-355.
6. Barone A, Derchi G, Rossi A, et al. Longitudinal clinical evaluation of bonded composite inlays: a 3-year study. Quintessence Int. 2008;39(1):65-71.
7. Hadis M, Leprince JG, Shortall AC, et al. High irradiance curing and anomalies of exposure reciprocity law in resin-based materials. J Dent. 2011;39(8):549-557.
8. Thonemann B, Federlin M, Schmalz G, Grundler W. Total bonding vs selective bonding: marginal adaptation of Class 2 composite restorations. Oper Dent. 1999;24(5):261-271.
9. Loguercio AD, Alessandra R, Mazzocco KC, et al. Microleakage in class II composite resin restorations: total bonding and open sandwich technique. J Adhes Dent. 2002;4(2):137-144.
10. Nandini S. Indirect resin composites. J Conserv Dent. 2010;13(4):184-194.
11. Gresnigt MM, Kalk W, Ozcan M. Randomized clinical trial of indirect resin composite and ceramic veneers: up to 3-year follow-up. J Adhes Dent. 2013;15(2):181-190.
12. Blank JT. Scientifically based rationale and protocol for use of modern indirect resin inlays and onlays. J Esthet Dent. 2000;12(4):195-208.
13. Small BW. Material choice for restorative dentistry: inlays, onlays, crowns, and bridges. Gen Dent. 2006;54(5):310-312.
14. Aykent F, Yondem I, Ozyesil AG, et al. Effect of different finishing techniques for restorative materials on surface roughness and bacterial adhesion. J Prosthet Dent. 2010;103(4):221-227.
15. Leinfelder KF. Indirect posterior composite resins. Compend Contin Educ Dent. 2005;26(7):495-503.
16. Santos GC Jr, Santos MJ, Rizkalla AS. Adhesive cementation of etchable ceramic esthetic restorations. J Can Dent Assoc. 2009;75(5):379-384.
17. Pashley DH, Ciucchi B, Sano H, et al. Bond strength versus dentine structure: a modelling approach. Arch Oral Biol. 1995;40(12):1109-1118.
18. Van Meerbeek B, Perdigão J, Lambrechts P, Vanherle G. The clinical performance of adhesives. J Dent. 1998;26(1):1-20.
19. Platt JA. Resin cements: into the 21st century. Compend Contin Educ Dent. 1999;20(12):1173-1182.
20. Braga RR, Cesar PF, Gonzaga CC. Mechanical properties of resin cements with different activation modes. J Oral Rehabil. 2002;29(3):257-262.
21. Breschi L, Mazzoni A, Ruggeri A, et al. Dental adhesion review: aging and stability of the bonded interface. Dent Mater. 2008;24(1):90-101.
22. D’Arcangelo C, De Angelis F, D’Amario M, et al. The influence of luting systems on the microtensile bond strength of dentin to indirect resin-based composite and ceramic restorations. Oper Dent. 2009;34(3):328-336.
23. D’Arcangelo C, De Angelis F, Vadini M, et al. Influence of curing time, overlay material and thickness on three light-curing composites used for luting indirect composite restorations. J Adhes Dent. 2012;14(4):377-384.
24. Roulet JF. A world without adhesion? J Adhes Dent. 2001;3(2):119.
25. Ikemura K, Endo T. A review of our development of dental adhesives–effects of radical polymerization initiators and adhesive monomers on adhesion. Dent Mater J. 2010;29(2):109-121.
26. Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34(6):849-853.
27. Bowen RL. Adhesive bonding of various materials to hard tooth tissues. 3. Bonding to dentin improved by pre-treatment and the use of surface-active comonomer. J Dent Res. 1965;44(5):903-905.
28. Roulet JF. Fool-proof adhesives? J Adhes Dent. 2002;4(1):3.
29. Van Meerbeek B, De Munck J, Mattar D, et al. Microtensile bond strengths of an etch & rinse and self-etch adhesive to enamel and dentin as a function of surface treatment. Oper Dent. 2003;28(5):647-660.
30. Busscher HJ, de Jong HP, van Pelt AW, Arends J. The surface free energy of human dental enamel. Biomater Med Devices Artif Organs. 1984;12(1-2):37-49.
31. Van Meerbeek B, De Munck J, Yoshida Y, et al. Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent. 2003;28(3):215-235.
32. Pashley DH, Carvalho RM. Dentine permeability and dentine adhesion. J Dent. 1997;25(5):355-372.
33. Ferrari M, Cagidiaco MC, Mason PN. Micromorphologic relationship between resin and dentin in Class II restorations: an in vivo and in vitro investigation by scanning electron microscopy. Quintessence Int. 1994;25(12):861-866.
34. Breschi L, Perdigão J, Lopes MM, et al. Morphological study of resin-dentin bonding with TEM and in-lens FESEM. Am J Dent. 2003;16(4):267-274.
35. Stona P, Borges GA, Montes MA, et al. Effect of polyacrylic acid on the interface and bond strength of self-adhesive resin cements to dentin. J Adhes Dent. 2013;15(3):221-227.
36. Heintze SD. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent. 2007;9(suppl 1):77-106.
37. Hickel R, Roulet JF, Bayne S, et al. Recommendations for conducting controlled clinical studies of dental restorative materials. Clin Oral Investig. 2007;11(1):5-33.
38. Perugia C, Ferraro E, Docimo R. Immediate dentin sealing in indirect restorations of dental fractures in paediatric dentistry. Eur J Paediatr Dent. 2013;14(2):146-149.
39. Dietschi D, Olsburgh S, Krejci I, Davidson C. In vitro evaluation of marginal and internal adaptation after occlusal stressing of indirect class II composite restorations with different resinous bases. Eur J Oral Sci. 2003;111(1):73-80.
40. de Waal H, Castellucci G. The importance of restorative margin placement to the biologic width and periodontal health. Part II. Int J Periodontics Restorative Dent. 1994;14(1):70-83.
41. Lutz E, Krejci I, Oldenburg TR. Elimination of polymerization stresses at the margins of posterior composite resin restorations: a new restorative technique. Quintessence Int. 1986;17(12):777-784.
42. Azevedo CG, De Goes MF, Ambrosano GM, Chan DC. 1-Year clinical study of indirect resin composite restorations luted with a self-adhesive resin cement: effect of enamel etching. Braz Dent J. 2012;23(2):97-103.
43. Nakabayashi N, Kojima K, Masuhara E. The promotion of adhesion by the infiltration of monomers into tooth substrates. J Biomed Mater Res. 1982;16(3):265-273.
44. Behr M, Hansmann M, Rosentritt M, Handel G. Marginal adaptation of three self-adhesive resin cements vs. a well-tried adhesive luting agent. Clin Oral Investig. 2009;13(4):459-464.
45. Magne P. Immediate dentin sealing: a fundamental procedure for indirect bonded restorations. J Esthet Restor Dent. 2005;17(3):144-155.
46. D’Arcangelo C, De Angelis F, Vadini M, D’Amario M. Clinical evaluation on porcelain laminate veneers bonded with light-cured composite: results up to 7 years. Clin Oral Investig. 2012;16(4):1071-1079.
47. Magne P, Nielsen B. Interactions between impression materials and immediate dentin sealing. J Prosthet Dent. 2009;102(5):298-305.
48. Magne P, Kim TH, Cascione D, Donovan TE. Immediate dentin sealing improves bond strength of indirect restorations. J Prosthet Dent. 2005;94(6):511-519.
49. Duarte S Jr, de Freitas CR, Saad JR, Sadan A. The effect of immediate dentin sealing on the marginal adaptation and bond strengths of total-etch and self-etch adhesives. J Prosthet Dent. 2009;102(1):1-9.
50. de Andrade OS, de Goes MF, Montes MA. Marginal adaptation and microtensile bond strength of composite indirect restorations bonded to dentin treated with adhesive and low-viscosity composite. Dent Mater. 2007;23(3):279-287.
51. Lee JI, Park SH. The effect of three variables on shear bond strength when luting a resin inlay to dentin. Oper Dent. 2009;34(3):288-292.
52. Broyles AC, Pavan S, Bedran-Russo AK. Effect of dentin surface modification on the microtensile bond strength of self-adhesive resin cements. J Prosthodont. 2013;22(1):59-62.
53. D’Arcangelo C, Vanini L, Prosperi GD, et al. The influence of adhesive thickness on the microtensile bond strength of three adhesive systems. J Adhes Dent. 2009;11(2):109-115.
54. Krämer N, Lohbauer U, Frankenberger R. Adhesive luting of indirect restorations. Am J Dent. 2000;13(spec no):60D-76D.
55. Soares CJ, Soares PV, Pereira JC, Fonseca RB. Surface treatment protocols in the cementation process of ceramic and laboratory-processed composite restorations: a literature review. J Esthet Restor Dent. 2005;17(4):224-235.
56. Schmage P, Cakir FY, Nergiz I, Pfeiffer P. Effect of surface conditioning on the retentive bond strengths of fiberreinforced composite posts. J Prosthet Dent. 2009;102(6):368-377.
57. D’Arcangelo C, Vanini L. Effect of three surface treatments on the adhesive properties of indirect composite restorations. J Adhes Dent. 2007;9(3):319-326.
58. Brosh T, Pilo R, Bichacho N, Blutstein R. Effect of combinations of surface treatments and bonding agents on the bond strength of repaired composites. J Prosthet Dent. 1997;77(2):122-126.
59. Hummel SK, Marker V, Pace L, Goldfogle M. Surface treatment of indirect resin composite surfaces before cementation. J Prosthet Dent. 1997;77(6):568-572.
60. Hori S, Minami H, Minesaki Y, et al. Effect of hydrofluoric acid etching on shear bond strength of an indirect resin composite to an adhesive cement. Dent Mater J. 2008;27(4):515-522.
61. Cavalcanti AN, De Lima AF, Peris AR, et al. Effect of surface treatments and bonding agents on the bond strength of repaired composites. J Esthet Restor Dent. 2007;19(2):90-99.
62. Lucena-Martín C, González-López S, Navajas-Rodríguez de Mondelo JM. The effect of various surface treatments and bonding agents on the repaired strength of heat-treated composites. J Prosthet Dent. 2001;86(5):481-488.
63. Bouschlicher MR, Cobb DS, Vargas MA. Effect of two abrasive systems on resin bonding to laboratory-processed indirect resin composite restorations. J Esthet Dent. 1999;11(4):185-196.
64. Honda MI, Flório FM, Basting RT. Effectiveness of indirect composite resin silanization evaluated by microtensile bond strength test. Am J Dent. 2008;21(3):153-158.
65. Lung CY, Matinlinna JP. Aspects of silane coupling agents and surface conditioning in dentistry: an overview. Dent Mater. 2012;28(5):467-477.
66. Valandro LF, Pelogia F, Galhano G, et al. Surface conditioning of a composite used for inlay/onlay restorations: effect on muTBS to resin cement. J Adhes Dent. 2007;9(6):495-498.
67. Cho SD, Rajitrangson P, Matis BA, Platt JA. Effect of Er,Cr:YSGG laser, air abrasion, and silane application on repaired shear bond strength of composites. Oper Dent. 2013;38(3):E1-E9.
68. Burnett LH Jr, Shinkai RS, Eduardo Cde P. Tensile bond strength of a one-bottle adhesive system to indirect composites treated with Er:YAG laser, air abrasion, or fluoridric acid. Photomed Laser Surg. 2004;22(4):351-356.
69. Moezizadeh M, Ansari ZJ, Fard FM. Effect of surface treatment on micro shear bond strength of two indirect composites. J Conserv Dent. 2012;15(3):228-232.
70. Caneppele TM, de Souza AC, Batista GR, et al. Influence of Nd:YAG or Er:YAG laser surface treatment on microtensile bond strength of indirect resin composites to resin cement. Lasers surface treatment of indirect resin composites. Eur J Prosthodont Restor Dent. 2012;20(3):135-140.
71. Bott B, Hannig M. Effect of different luting materials on the marginal adaptation of Class I ceramic inlay restorations in vitro. Dent Mater. 2003;19(4):264-269.
72. Peutzfeldt A. Dual-cure resin cements: in vitro wear and effect of quantity of remaining double bonds, filler volume, and light curing. Acta Odontol Scand. 1995;53(1):29-34.
73. Caughman WF, Chan DC, Rueggeberg FA. Curing potential of dual-polymerizable resin cements in simulated clinical situations. J Prosthet Dent. 2001;86(1):101-106.
74. Hofmann N, Papsthart G, Hugo B, Klaiber B. Comparison of photo-activation versus chemical or dual-curing of resin-based luting cements regarding flexural strength, modulus and surface hardness. J Oral Rehabil. 2001;28(11):1022-1028.
75. Santos MJ, Passos SP, da Encarnação MO, et al. Hardening of a dual-cure resin cement using QTH and LED curing units. J Appl Oral Sci. 2010;18(2):110-115.
76. Acquaviva PA, Cerutti F, Adami G, et al. Degree of conversion of three composite materials employed in the adhesive cementation of indirect restorations: a micro-Raman analysis. J Dent. 2009;37(8):610-615.
77. de Menezes MJ, Arrais CA, Giannini M. Influence of light-activated and auto- and dual-polymerizing adhesive systems on bond strength of indirect composite resin to dentin. J Prosthet Dent. 2006;96(2):115-121.
78. D’Amario M, Pacioni S, Capogreco M, et al. Effect of repeated preheating cycles on flexural strength of resin composites. Oper Dent. 2013;38(1):33-38.
79. D’Amario M, De Angelis F, Vadini M, et al. Influence of a repeated preheating procedure on mechanical properties of three resin composites. Oper Dent. 2015;40(2):181-189.
80. Perdigão J. New developments in dental adhesion. Dent Clin North Am. 2007;51(2):333-357, viii.
81. Han L, Okamoto A, Fukushima M, Okiji T. Evaluation of physical properties and surface degradation of self-adhesive resin cements. Dent Mater. 2007;26(6):906-914.
82. Blunck U, Zaslansky P. Effectiveness of all-in-one adhesive systems tested by thermocycling following short and long-term water storage. J Adhes Dent. 2007;9(2 suppl):231-240.
83. De Munck J, Vargas M, Van Landuyt K, et al. Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater. 2004;20(10):963-971.
84. Radovic I, Monticelli F, Goracci C, et al. Self-adhesive resin cements: a literature review. J Adhes Dent. 2008;10(4):251-258.
85. Türkmen C, Durkan M, Cimilli H, Öksüz M. Tensile bond strength of indirect composites luted with three new self-adhesive resin cements to dentin. J Appl Oral Sci. 2011;19(4):363-369.
86. Fuentes MV, Ceballos L, González-López S. Bond strength of self-adhesive resin cements to different treated indirect composites. Clin Oral Investig. 2013;17(3):717-724.
87. Giráldez I, Ceballos L, Garrido MA, Rodríguez J. Early hardness of self-adhesive resin cements cured under indirect resin composite restorations. J Esthet Restor Dent. 2011;23(2):116-124.
88. Viotti RG, Kasaz A, Pena CE, et al. Microtensile bond strength of new self-adhesive luting agents and conventional multistep systems. J Prosthet Dent. 2009;102(5):306-312.
89. Pashley DH, Sano H, Ciucchi B, et al. Adhesion testing of dentin bonding agents: a review. Dent Mater. 1995;11(2):117-125.
90. Frankenberger R, Krämer N, Petschelt A. Technique sensitivity of dentin bonding: effect of application mistakes on bond strength and marginal adaptation. Oper Dent. 2000;25(4):324-330.
91. Stewart GP, Jain P, Hodges J. Shear bond strength of resin cements to both ceramic and dentin. J Prosthet Dent. 2002;88(3):277-284.
92. Swift EJ Jr, Perdigão J, Combe EC, et al. Effects of restorative and adhesive curing methods on dentin bond strengths. Am J Dent. 2001;14(3):137-140.
93. Mak YF, Lai SC, Cheung GS, et al. Micro-tensile bond testing of resin cements to dentin and an indirect resin composite. Dent Mater. 2002;18(8):609-621.
94. da Cruz MK, Martos J, Silveira LFM, et al. Odontoplasty associated with clinical crown lengthening in management of extensive crown destruction. J Conserv Dent. 2012;15(1):56-60.
95. Bader JD, Rozier RG, McFall WT Jr, Ramsey DL. Effect of crown margins on periodontal conditions in regularly attending patients. J Prosthet Dent. 1991;65(1):75-79.
96. Schätzle M, Land NP, Anerud A, et al. The influence of margins of restorations of the periodontal tissues over 26 years. J Clin Periodontol. 2001;28(1):57-64.
97. Nilsson E, Alaeddin S, Karlsson S, et al. Factors affecting the shear bond strength of bonded composite inlays. Int J Prosthodont. 2000;13(1):52-58.
98. Bayne SC, Schmalz G. Reprinting the classic article on USPHS evaluation methods for measuring the clinical research performance of restorative materials. Clin Oral Investig. 2005;9(4):209-214.
99. Huth KC, Chen HY, Mehl A, et al. Clinical study of indirect composite resin inlays in posterior stress-bearing cavities placed by dental students: results after 4 years. J Dent. 2011;39(7):478-488.
100. Manhart J, Chen HY, Neuerer P, et al. Three-year clinical evaluation of composite and ceramic inlays. Am J Dent. 2001;14(2):95-99.
101. Leirskar J, Henaug T, Thoresen NR, et al. Clinical performance of indirect composite resin inlays/onlays in a dental school: observations up to 34 months. Acta Odontol Scand. 1999;57(4):216-220.
102. Scheibenbogen-Fuchsbrunner A, Manhart J, Kremers L, et al. Two-year clinical evaluation of direct and indirect composite restorations in posterior teeth. J Prosthet Dent. 1999;82(4):391-397.
103. Cetin AR, Unlu N, Cobanoglu N. A five-year clinical evaluation of direct nanofilled and indirect composite resin restorations in posterior teeth. Oper Dent. 2013;38(2):E1-E11.
About the Authors
Camillo D’Arcangelo, DDS
Department of Restorative Dentistry
School of Dentistry
University G. D’Annunzio
Chieti, Italy
Lorenzo Vanini, MD, DDS
Private Practice
Chiasso, Switzerland
Matteo Casinelli, DDS
Unit of Restorative Dentistry
Department of Life
Health and Environmental Sciences
School of Dentistry
University of L’Aquila
L’Aquila, Italy
Massimo Frascaria, DDS, PhD
Unit of Restorative Dentistry
Department of Life
Health and Environmental Sciences
School of Dentistry
University of L’Aquila
L’Aquila, Italy
Francesco De Angelis, DDS, PhD
Department of Restorative Dentistry
School of Dentistry
University G. D’Annunzio
Chieti, Italy
Mirco Vadini, DDS, PhD
Department of Restorative Dentistry
School of Dentistry
University G. D’Annunzio
Chieti, Italy
Maurizio D’Amario, DDS, PhD
Unit of Restorative Dentistry
Department of Life
Health and Environmental Sciences
School of Dentistry
University of L’Aquila
L’Aquila, Italy
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.