You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Today's health care system utilizes a collaborative approach to patient care. This team-based style, in part, results from the increased prevalence of chronic illnesses, deficits in the provision of medical care, growing life expectancy rates, and the complexities of the modern health care system.1 Heightened realization of these issues has prompted health care professionals to work together with patients, families, and communities in an attempt to deliver comprehensive care and achieve favorable health and well-being outcomes through interprofessional collaborative practice.2
Given the paradigm shift from a siloed to multiprofessional approach, health science academia is charged with preparing students to enter a collaborative workforce. Interprofessional education (IPE) has been proposed as a viable solution to meet the current demands, as its intent is to promote effective communication, foster teamwork, improve health outcomes, and increase one's appreciation and understanding of other health care professionals.2
Numerous health science disciplines, including medicine and nursing, have already adopted IPE in their curricula.3 However, research shows that many dental hygiene programs have not started to incorporate shared teaching and learning experiences into their courses of study.4-6 One obstacle may be due to the fact that only a small percentage of dental hygiene programs in the United States (U.S.) are located within dental schools or on health science campuses, thus limiting IPE opportunities.4 Professional education and training experiences have also been shown to greatly influence knowledge, skill sets, and confidence. Dental hygiene students do not always perceive themselves as fundamental members of collaborative health care teams, an issue likely due to a lack of exposure to collective learning experiences.7 Additionally, dental hygiene students may be unfamiliar with the roles and responsibilities of other health care providers.5 These circumstances create the setting for subsequent self-perceptions and abilities. Research by Bell et al. revealed that many of the dental hygienists surveyed felt that their knowledge levels of certain oral-systemic diseases in addition to their confidence levels associated with the management of specific at-risk patients, needed improvement.8 This lack of knowledge and self-confidence may have developed due to the unavailability of IPE, which is problematic considering academic goals of dental hygiene education programs should support the current collaborative practice concepts in order to graduate competent health care providers.
Evidence demonstrates a strong correlation between oral and systemic health, and calls for dental hygienists to be primary members of interprofessional teams based on their expertise in the prevention and treatment of oral diseases. In spite of the demand, dental hygienists are not frequent collaborators on these interprofessional health care teams.6 An additional emphasis has also been placed on uniting the long-standing divide between dental and medical professions.9 In view of the limited IPE opportunities for many dental hygiene students, bridging this divide can be challenging.
The American Dental Hygienists' Association (ADHA) has recognized the critical need for interprofessional collaboration, and contributed to the development of a transformative vision to advance dental hygiene through restructuring the educational system.4,10 IPE was a recurring theme at the September 2013 symposium, "Transforming Dental Hygiene Education: Proud Past, Unlimited Future."10 The resulting white paper, Transforming Dental Hygiene Education and the Profession of the 21st Century further elaborated on the strategies highlighted at the conference.4 Incorporating interprofessional teaching methodologies and creating interdisciplinary experiences within dental hygiene curricula will enable the profession to remain relevant in an constantly evolving health care system. Additionally, IPE experiences are expected to contribute to the amalgamation of oral and medical services, raise the standard of care, and graduate professionals that are primed to enter a collaborative health care system.
As this transformation must begin within the educational system, attention is placed on the academic leaders who bear the responsibility of developing and facilitating interprofessional action strategies. However, educators' perceived lack of value and commitment towards IPE impedes advancement,3,11 and has been identified as a primary obstacle to successful actualization.5 A team-based approach is not always a vision shared among academic leaders. Historically, health science faculty are accustomed to operating in uni-professional environments and the majority of these faculty members were trained prior to the emergence of IPE, making it difficult to recognize the value of this approach.12 Subsequently, this perception has led to some resistance to embracing interprofessional teaching.12 Understanding faculty convictions and aligning attitudes with the objectives of collaborative education and health systems are essential to creating a comprehensive needs assessment and successful IPE program development as the basis for transforming the education process.
The attitudes of dental hygiene administrators and educators towards IPE have not been well documented. Current literature suggests that there is a need to evaluate faculty feelings about shared teaching and learning as well as the attitudinal and institutional factors influencing IPE execution.13,14 Dental hygiene administrators and faculty are responsible for the implementation of interprofessional education, ultimately bridging the gap between education and the requirements and realities of clinical practice. Examining these administrator and faculty perceptions may foster further discussion and create new opportunities for transitioning dental hygiene education to the collaborative, interprofessional model. The purpose of this study was to assess the attitudes of dental hygiene administrators and faculty members about the value of IPE within dental hygiene curricula and to determine whether administrator and faculty perspectives were associated with their professional role, gender, experience, knowledge about IPE, and their use of collaborative teaching strategies.
Methods
The Institutional Review Board of the University of New England, Maine approved this quantitative, cross-sectional study. The study population consisted of the program directors and faculty members of all Commission on Dental Accreditation (CODA) approved, entry-level dental hygiene programs located within the Northeast region of the United States (U.S.).
A combination of snowball and convenience sampling was used to select the study sample using the program website and department contact information available via the ADHA website.15 Program directors were also contacted personally in an attempt to obtain their email addresses in addition to those of their faculty members. In the case of an unresponsive program director, available email addresses were obtained directly from the program website.
The 34-question self-reported survey was comprised of three demographic items, one item assessing knowledge of IPE, one item on current use of IPE, one item about the basis for reported viewpoints, and two Likert scales (totaling 28 items) assessing attitudes towards IPE and interprofessional learning in the academic setting. Both Likert scales used a 5-point rating system, with 1 equaling "strongly disagree" and 5 equaling "strongly agree." The 15-item Likert scale, Attitudes towards Interprofessional Education, was adapted from Parsell and Bligh by Curran, et al.16,17 Curran et al. has also adopted the 13-item Likert scale, Attitudes towards Interprofessional Learning in the Academic Setting, from Gardner, et al.17,18 Permission was granted via email correspondence by Curran to use both scales in this study. Although previously validated, Cronbach's alpha was calculated, demonstrating high internal consistency and reliability across both scales. Cronbach's alpha for Attitudes towards Interprofessional Education was 0.88 and for Attitudes towards Interprofessional Learning in the Academic Setting was 0.78.
The survey was developed and administered via SurveyMethods online software.19 Dental hygiene administrators and faculty in the Northeast region of the U.S. were invited to complete the survey by means of an electronic mail containing a recruitment cover letter and a customized link containing the research consent form and study details, followed by the survey. Survey completion indicated consent to participate in the study. To maintain the anonymity and confidentiality of respondents, no identifying information was collected, including details about their specific institutions. Additionally, software settings were programmed to ensure that Internet Protocol (IP) addresses were not captured and the secure socket layer (SSL) feature was used. After the initial launch of the survey, three follow up emails were sent to non-responders to increase the response rate.
Survey data was downloaded from SurveyMethods as an excel file, and then entered into Statistical Package for the Social Sciences (SPSS) 23. Descriptive statistics were used to measure attitudes by calculating the mean (M) score of all Likert scale items. Additionally, the mode emphasized the most frequently selected underlying factor explaining viewpoints. Inferential statistics were used to ascertain if perspectives were correlated to the following survey variables: professional role, gender, experience, knowledge, and use of IPE. The Spearman's rho (rs) correlation coefficient detected and computed any significant associations present among variables. Ordinal regression analyses were used to draw inferences between these relationships. Data was checked to ensure that all assumptions for running this test were met, validating results. Statistical significance was determined by p-values that were less than or equal to 0.05.
Results
Of the 224 administrators and faculty members invited to participate in the study, 91 completed the survey, resulting in a response rate of 41%.
Demographic Characteristics
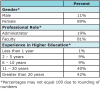
Demographic information about survey respondents was collected and shown in Table I. Most of the respondents reported that they were females in the role of a faculty member. Their experience in higher education was similarly distributed in intervals ranging from two to 10 years and from 11 to more than 20 years, respectively.
Attitudes Towards IPE
Likert scale items and the mean scores of the 15 statements for Attitudes towards Interprofessional Education are exhibited in Table II. Similarly, Table III presents the 13 Likert scale items and associated mean ratings for Attitudes towards Interprofessional Learning in the Academic Setting. Mean calculations were used to determine the perspectives towards each statement. Separate measurements of each item was key to the assessment of the individual attitudes towards the multiple components of IPE thus revealing elements that were favored and identifying areas that were not held in the same regard. Scores closer to 5.00 indicated positivity, whereas those closer to 1.00 indicated negativity. Reversed scored items, shown on Tables II and III, were appropriately calculated.
According to mean scores, survey respondents expressed favorability towards interprofessional pedagogy. They felt most strongly about the importance of health care students acquiring teamworking skills (M = 4.41). High levels of agreement revealed that this will better prepare them to work in groups (M = 4.22) once they enter the collaborative practice workforce, and being impactful when doing so (M = 4.27). Respondents believed that IPE would improve communication skills with patients and other professionals (M = 4.26). Positivity was expressed towards students having a higher quality understanding of clinical issues because of joint learning (M = 4.16). Administrators and faculty deemed a collaborative approach as essential when resolving patient problems (M = 4.40), and felt that if learning within these collaborations is to be effective, individuals need to have a common trust and esteem for each other (M = 4.39). IPE is expected to enhance students' outlooks towards other health care professionals (M = 4.28). Furthermore, respondents anticipated that it would assist learners in recognizing their professional shortcomings (M = 3.98). Overall, they agreed that IPE, taking place before qualification, would improve actual practice (M = 4.22).
Administrators and faculty believed that IPE should be a goal of their campus (M = 3.96). This viewpoint can be clarified through agreement expressed with the following statements: "students like courses that include students from other academic departments" (M = 3.42), "faculty like teaching to students in other academic departments" (M = 3.42), and "faculty like teaching with faculty from other academic departments" (M = 3.49). Respondents felt that in order for interprofessional efforts to be successful, support from administration is requisite (M = 4.39). They agreed that health science campuses should encourage faculty to become involved in teaching multidisciplinary courses (M = 4.07), which could satisfy the notion that institutions should offer their students shared learning experiences (M = 4.09).
Additional mean scores identified in Tables II and III mostly reiterated the stated results. Based on the respondents' levels of agreement with the majority of the statements, more positive than negative attitudes were expressed.
The Basis for Attitudes
The mode served as an indication of the factor that was the most commonly selected explanation for the attitudes of survey respondents towards IPE (Table IV). The basis for perspectives was distributed across the study population. Some respondents specified that their viewpoints could be described by positive factors, such as being in favor of working with other professions (36%); whereas others attributed their feelings to negative factors, such as the barriers perceived to be associated with this educational typology (12%).
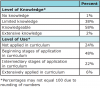
Perspectives Related to Knowledge and Use
Respondents' understanding of IPE and the extent to which they apply it in dental hygiene curricula was explored (Table V). Of the surveyed population, 58% (n=53) were knowledgeable about interprofessional pedagogy, while 38% (n=35) possessed limited knowledge. Furthermore, 48% (n=44) reported that they were in the beginning stages of applying IPE in the dental hygiene curriculum of their affiliated institutions, while 24% (n=22) indicated it is not being applied in the curriculum on any level.
The Spearman's rho correlation coefficient, implementing a two-tailed test of significance, was used to determine any existing relationships between respondents' attitudes and their professional role, gender, experience, knowledge about IPE, and utilization of this teaching methodology. Significant correlations were revealed between perspectives and knowledge (rs =.303) as well as perspectives and use (rs =.269).
Ordinal regression analyses were calculated for each Likert scale item (Tables II and III) and for each level of the variables knowledge and use (Table V), further exploring the relationships identified by the Spearman's rho correlation coefficient. Statistically significant associations (p≤0.05) were noted, detailing the connection between respondents' attitudes towards IPE and their understanding as well as its use. (Table VI and Table VII)
Significant relationships between attitudes and knowledge about IPE were demonstrated. (Tables VI and VII) The 1% of survey respondents with no knowledge (p=0.00) of IPE in addition to the 38% with limited knowledge (p=0.00) of it, felt that multidisciplinary learning would bring about positive feelings towards other health care professionals. Additionally, those with no knowledge (p=0.00) and minimal comprehension (p=0.00) of inter-professional practices, felt that patients would benefit from a collaborative care approach. This same 1% (p=0.00) and 38% (p=0.00) of the population believed that IPE is a necessity for health science programs. Respondents reporting no (p=0.00) or little familiarity (p=0.00) with collaborative education, still strongly agreed that exposure to IPE during training, produces competent members of integrated medical groups. Even with limited understanding (p=0.00) of interprofessional concepts, administrators and faculty strongly believed that team-based learning is only effective in the presence of mutual trust and respect. Little acquaintance (p=0.00) with IPE was still sufficient for recognizing how it enhances communication skills. Respondents with different knowledge levels, varying from limited (p=0.02) to well informed (p=0.02), expressed more agreement with the concept that students would enjoy working with faculty from departments other than their own. Responders citing no awareness (p=0.00) of, or having minimal insight (p=0.00) into interprofessional practices, believed that IPE does not diminish course material. Thirty-eight percent of the population reporting some knowledge (p=0.00) of IPE, felt that institutional support is necessary in order for joint efforts to be successful.
Statistically significant associations were also identified between attitudes and the extent to which IPE is applied within dental hygiene curricula as shown in Tables VI and VII. The 48% of the respondents who are beginning to implement IPE (p=0.04) felt that by doing so, they are fostering students' capacity to better grasp clinical issues. Even the 24% of respondents who have not adopted interprofessional teaching (p=0.03), felt that this approach does not devalue course content. Furthermore, respondents who are not implementing IPE (p=0.04) and those in the very beginning stages of doing so (p=0.04) agreed that the orchestration and execution of such efforts is onerous.
Discussion
This study surveyed dental hygiene administrators and faculty members to determine their attitudes about the value of interprofessional education within dental hygiene curricula. Additionally, it sought to document whether these perspectives are associated with participants' professional role, gender, experience, knowledge about IPE, and use of collaborative teaching strategies.
Although previous research has assessed attitudes towards IPE, minimal studies focus specifically on dental hygiene administrators and educators. This study allows for the discipline of dental hygiene to be included in the literature with the results demonstrating overall positive attitudes toward IPE among the majority of the population surveyed. In comparison to other studies assessing the standpoints from other health care disciplines, the current research was similar in that both program directors and faculty value shared educational pedagogy.17,18,20
Data analysis confirmed that the respondents in this study expressed a strong affirmation in regard to IPE benefitting students as well as patients. Interprofessional learning is believed to enhance student viewpoints about other health care professionals. IPE experiences are also expected to effectively prepare students to be highly competent members of the collaborative practice workforce by focusing on the clarification of patient problems and fostering team-working skills. As a result of increased student abilities, a higher quality of care will be delivered to patients, heightening health outcomes and overall well-being. Approbatory attitudes reveal that collaborative pedagogy is perceived as a frontrunner for maintaining the relevance of dental hygiene while simultaneously confronting the demands of today's health care system.
Respondents' positive perspectives towards IPE were associated with their comprehension of IPE. Since only 1% of the population reported no comprehension of this educational methodology, the primary relationships were between supportive feelings and knowledge levels ranging from limited to adequate. Sentiments correspond with the intention to develop and boost the understanding of IPE. Therefore, positivity is enhancing one's desire to learn more about interprofessional practices, increasing the adoption of them. Curran's et al. study on the attitudes of health sciences faculty members towards interprofessional teamwork and education demonstrated equivalent results indicating that there is a direct correlation between positivity and the interprofessional experience.17 The familiarity and proficiency of collaborative teaching and learning are higher when the importance, worth, and usefulness of it are better perceived by the participants.
Sentiments held by those expected to design and facilitate interprofessional initiatives influence successful implementation. Findings from this study reveal that positive attitudes are related to the extent in which the participants apply IPE within dental hygiene curricula; specifically, at two application levels: not using IPE and beginning to implement it. Although favorable sentiments towards IPE were widespread, the majority population in this study were not affiliated with program curricula structured on an IPE framework. In reality, the use of interprofessional strategies varied greatly among the respondents. An estimated one-quarter of the population do not utilize any shared teaching in their curriculum, approximately one-half are in the infancy stages of IPE execution and approximately one fifth are in the intermediary phases of implementation, and only 6% reported extensive application of interprofessional practices. While these findings reinforce previously reported data indicating that collaborative learning is restricted in dental hygiene education,4,5 they also illustrate the impact of positive viewpoints on the commencement and evolution of IPE which in turn can help overcome inherent limitations. This evidence also reinforces the views held by the Association of Academic Health Centers acknowledging the importance of positive perspectives among faculty in supporting implementation efforts.21
Examining the rationale behind the reported attitudes is key to the development of a descriptive needs assessment, an essential step towards the successful implementation of interprofessional strategies in the curriculum.22 Respondents indicated the basis for their feelings by selecting factors related to leadership support, knowledge, risks, benefits, training, and barriers to IPE. Identification of these attitudes can help serve as the foundation for transformative efforts so that movement towards IPE implementation within dental hygiene education can take place. As a next step, administrators and faculty should reference the information provided to assist with facilitating the development of IPE plans at institutional and individual levels. Specific faculty interests and concerns should be addressed in this process. As many of the respondents in this survey demonstrated limited or adequate understanding of interprofessional pedagogy, efforts should be directed at improving the skills, knowledge, and abilities of those individuals expected to carry out IPE initiatives. Findings from this assessment may be used to inform professional and organizational development, inservice training, informal and formal experiences, as well as other interventions identified to effectively and efficiently prepare faculty to implement IPE into dental hygiene curricula. Faculty involvement in shared teaching and learning requires training; without supportive training experiences, the willingness to be involved in IPE will be minimal.23 The affirmative attitudes identified in this study provide a positive environment for IPE that needs to be fostered.
While these results provide useful information about dental hygiene administrator and faculty perspectives regarding IPE, there are limitations to this study. First, respondents were affiliated with dental hygiene programs located exclusively in the Northeast region of the U.S. and cannot be generalized to dental hygiene programs across the nation. Also, the study findings do not reflect other health science disciplines outside of dental hygiene. Second, although all of the various dental hygiene departments in the Northeast were contacted, there was no way of determining if individuals from each program completed the survey as all identifiers were removed to protect the confidentiality of the participants. Additionally, individuals who support IPE may have been more inclined to participate in the study. Finally, survey questions were self-reported and could have been construed differently among respondents.
Recommendations for future study include the following: a nationwide exploration of dental hygiene administrator and faculty attitudes towards IPE to provide generalizable findings; an investigation of pre- and post-IPE training faculty perspectives to examine the role knowledge plays in influencing viewpoints; an assessment of negative attitudes towards IPE to foster understanding of the basis for resistance; a survey of the attitudes of administrators and faculty members that are affiliated with programs that vary in the extent in which IPE is implemented; an investigation into student learning and clinical practice behavior outcomes following graduation from programs implementing IPE in the curriculum.
Conclusion
Dedicated administrators and faculty members are required to successfully address the paradigm shift in health science academia. Graduates must be well prepared to enter the collaborative practice environment expected of the health care workforce and the attitudes of educators towards IPE plays an important role in this process. The majority of the dental hygiene administrators and faculty members surveyed in this study recognize the value and significance of using IPE to effectively prepare students to enter this new, collaborative workforce. Articulated perspectives by administrators and faculty revealed an interest in moving towards more interdisciplinary teaching methodologies and the findings exposed points of interest and concerns, which can be referenced in advancing future collaborative efforts. Perspectives from this study demonstrate that dental hygiene is on the appropriate path for incorporating interprofessional strategies into program curricula.
Acknowledgements
The author would like to thank Carey Clark, PhD, John Lustig, EdD and Maureen Tsokris, RDH, EdD, for their guidance and support throughout this dissertation research project, and Juan Jaramillo, PhD for his statistical assistance.
About the Author
Cristina M. Casa-Levine, RDH, MS, EdD, is an assistant professor, Department of Dental Hygiene, Farmingdale State College, New York, NY.
Corresponding author: Cristina M. Casa-Levine, RDH, MS, EdD; Casacm1@Farmingdale.edu
References
1. Croker A, Trede F, Higgs, J. Collaboration: what is it like? Phenomenological interpretation of the experience of collaboration within rehabilitation teams. J. Interprof Care. 2012 Jan;26:13-20.
2. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, CH: Health Professions Network Nursing and Midwifery Office within the Department of Human Resources for Health; 2010.
3. Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: report of an expert panel [Internet]. Washington, (D.C.): Interprofessional Education Collaborative; 2011 May. [cited 2016 August 15]. Available from: http://www.aacn.nche.edu/education-resources/ipecreport.pdf
4. American Dental Hygienists' Association. Transforming dental hygiene education and the profession for the 21st century [Internet]. Chicago, (IL); American Dental Hygienists' Association; 2015 [cited 2016 August 15]. Available from: http://www.adha.org/adha-transformationalwhitepaper
5. Brame JL, Mitchell SH, Wilder RS, Sams LD. Dental and allied dental students' attitudes towards and perceptions of intraprofessional education. J Dent Educ. 2015 Jun;79(6): 616-25.
6. Swanson Jaecks K. Current perceptions of the role of dental hygienists in interdisciplinary collaboration. J Dent Hyg. 2009 Spring; 83(2):84-91.
7. Duley SI, Fitzpatrick PG, Zornosa X, Barnes, WG. A center for oral health promotion: establishing an inter-professional paradigm for dental hygiene, health care management and nursing education. J Dent Hyg. 2012 Spring; 86(2):63-70.
8. Bell KP, Phillips CP, Paquette DW, Offenbacher S, Wilder RS. Dental hygienists' knowledge and opinions of oral-systemic connections: implications for education. J Dent Educ. 2012 Jun; 76(6):682-94.
9. Mouradian WE, Lewis CW, Berg JH. Integration of dentistry and medicine and the dentist of the future: the need for the health care team. Calif Dent Assoc J. 2014 Oct; 42:687-96.
10. Battrell A, Lynch A, Steinbach P, et al. Professional growth: advancing education in dental hygiene. J Evid Base Dent Pract. 2014 Jun;14(Sup 1):209-21.e1.
11. VanderWielen LM, Vanderbilt AA, Dumke EK, et al. Improving public health through student-led interprofessional extracurricular education and collaboration: a conceptual framework. J Multidiscip Healthc. 2014 Feb;7:105-10.
12. Becker KL, Hanyok LA, Walton-Moss B. The turf and baggage of nursing and medicine: moving forward to achieve success in interprofessional education. J Nurse Pract. 2014 Apr;10(4):240-44.
13. Lash DB, Barnett MJ, Parekh N, et al. Perceived benefits and challenges of interprofessional education based on a multidisciplinary faculty member survey. Am J Pharm Educ. 2014 Dec;78(10):1-9.
14. Loversidge J, Demb A. Faculty perceptions of key factors in interprofessional education. J. Interprof Care. 2015; 29(4):298-304.
15. American Dental Hygienists' Association. Entrylevel dental hygiene programs. [Internet]. Chicago (IL): American Dental Hygienists' Association; 2016. [cited 2016 August 30]. Available from: http://www.adha.org/resources-docs/71617_Entry_Level_Schools_By_States.pdf
16. Parsell G, Bligh J. The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Med Educ. 1999 Feb;33:95-100.
17. Curran VR, Sharpe D, Forristall, J. Attitudes of health sciences faculty members towards interprofessional teamwork and education. Med Educ. 2007 Sep;41:892-896.
18. Gardner SF, Chamberlin GD, Heestand DE, Stowe CD. Interdisciplinary didactic instruction at academic health centres in the United States: attitudes and barriers. Adv Health Sci Educ. 2002;7:179-190.
19. Survey Methods. Survey software: ask, analyze, improve. [Internet]. SurveyMethods; 2015 [cited 2016 August 30]. Available from: https://www.surveymethods.com/index.aspx
20. Curran VR, Deacon DR, Fleet L. Academic administrators' attitudes towards interprofessional education in Canadian schools of health professional education. J Interprof Care. 2005 May; Supp 1: 76-86.
21. Rafter ME, Pesun IJ, Herren M, et al. A preliminary survey of interprofessional education. J Dent Educ. 2006 Apr;70(4): 417-27.
22. Buring SM, Bhushan A, Brazeau G, et al. Keys to successful implementation of interprofessional education: learning location, faculty development, and curricular themes. Am J Pharm Educ. 2009 Jul; 73(4):1-11.
23. Hall LW, Zierler BK. Interprofessional education and practice guide no.1: developing faculty to effectively facilitate interprofessional education. J Interprof Care. 2015 Jan; 29(1): 3-7.