You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
A clinician's endodontic success rate can be difficult to determine, either in the long or short term. Complications of root canal anatomy can make success difficult to gauge. The main opportunity that clinicians can take advantage of regarding root canal system anatomy relates to microanatomy. This article will provide an overview of root canal system anatomy and historical root canal therapy. It will then introduce multisonic technology, which can dramatically improve endodontic outcomes for patients. This technology enables clinicians to be more conservative in their treatment and achieve greater case success.1,2
Endodontic Success and the Root Canal System
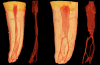
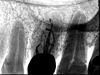
Some dentists are familiar with the 1917 study of the root canal system that was brought to the United States in 1925 by Walter Hess.3 The study set the benchmark for the modern understanding of dental anatomy, but it also created limitations, because of the concept of a single "root canal." A better concept for this anatomy is root canal "systems," a term introduced by Dr. Herbert Schilder in 1974.4Today, a cursory Google search will provide incredibly detailed displays of digitized micro computed tomography (CT) of root canal system anatomy. These images demonstrate the complexity of root canal systems, which can be compared to a fingerprint because of their person-specific nature. Figure 1 provides a representation of a lower premolar micro CT that makes it clear how difficult the endodontic clinician's task of cleaning and shaping such an intricate system can be. This complexity also illustrates why clinicians may be falling short of fully debriding and disinfecting these anatomical systems regardless of what instruments and irrigation protocols are utilized.
Irrigation methods have changed over time, transitioning from passive irrigation to active irrigation. Gutta-percha cone activation gave way to the EndoActivator® (Dentsply Sirona, dentsplysirona.com) by Dr. Clifford Ruddle, which opened the door for moving irrigants more effectively throughout the root canal system. Next came ultrasonic activation technologies, including PiezoFlow® (Dentsply Sirona), EndoVac® (Kerr Dental, kerrdental.com), and, more recently, EndoVac Pure™ (Kerr Dental), which have collectively helped clinicians to realize the value of active over passive irrigation. In the 1970s and early 1980s, dental school education for root canals did not consider the system view. This limited perspective later shifted, as exemplified by Schilder's article, "Cleaning and Shaping the Root Canal."4 In a key quote from this article, Schilder states, "Initially, root canals were manipulated primarily to allow placement of intracanal medicaments, with little attempt to remove completely the organic contents of the root canal system. In spite of elaborate modifications over the years, many methods of preparing root canals mechanically still fail to cleanse root canal systems effectively."
Schilder, whose thinking was forward-looking, provided five mechanical objectives. These five objectives were reduced to four by Ruddle: continuous tapering preparation, original anatomy maintained, position of foramen maintained, and foramen kept as small as practical.5 With new, disruptive root canal treatment technology currently on the market, the objective of a continuous tapering preparation is, in the opinion of these authors, perhaps no longer necessary. Throughout the history of endodontics, there have been many times when a new technology challenged the status quo, was dismissed or disliked, but then became the norm. Microscope technology that emerged in the early 1990s and cone-beam computed tomography (CBCT)/three-dimensional (3D) imaging are examples of disruptive technologies that were met with skepticism but have now become commonplace.
Advanced Root Canal Technology
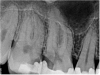
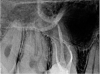
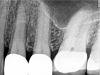
The new technology introduced in this article is based on advanced multisonic technology. Several current systems take advantage of ultrasonics and/or piezoelectric ultrasonic technology to deliver endodontic therapy. Some of these include MiniEndo™ (Kerr Dental), Varios® (NSK, nskdental.us), and Newtron® (Satelec, A-dec Inc, a-dec.com). The cases documented in this article feature the GentleWave® System (Sonendo®, sonendo.com), which employs a proprietary multisonic cleansing technology to deliver therapeutic irrigants into the root canal system, including lateral canals and tubules of complex root canal systems, while leaving the dentin largely intact.1,6-11 In the case shown in Figure 2 (preoperative radiograph) and Figure 3 (postoperative), the clinician was initially under the misconception that simple "cleaning and shaping" could be used for the root canal system in the conventional manner. The clinician evaluated the root canal system digitally in 2D and 3D before starting the case. The case was accessed, prepared, and cleaned and disinfected. Special attention to the digital imagery of the mesiobuccal root complex allowed the clinician to appreciate that the MB1 and MB2 merged before exiting from a common foramen. The 2D postoperative radiograph (Figure 3) illustrates that all of the mechanical objectives were realized.
Figure 4 shows another preoperative radiographic image. The clinician was especially interested in observing what would happen in the apical one-third of the distal canal. Figure 5 shows the cone-fit radiograph, and Figure 6 shows the postoperative 2D image. The introduction of multisonic technology allowed the clinician to preserve more dentin while keeping the access more conservative.
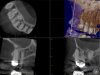
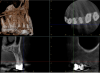
Figure 7 shows another tooth that was diagnosed with a necrotic pulp; Figure 8 shows a preoperative CBCT slice from the volumetric scan of the tooth. The clinician observed that there was more than one canal in the mesiobuccal system and that a periapical lesion was present. Lesions were visible radiographically on every root, adjacent to numerous portals of exit in the apical one-third. In this case, the clinician aimed to be more conservative and was able to better maintain the original anatomy. In the mesiobuccal root, the canals crisscrossed, and considering the delicate anatomy in the apical one-third, it was imperative to keep the foramen as small as practical. A much larger palatal canal was also observed. The clinician provided a coronal seal buildup before the rubber dam was removed from the tooth. Figure 9 shows the postoperative 2D radiograph.
Figure 10 is from a case on the upper arch, tooth No. 3. On the distal buccal area, superimposed over the palatal and distobuccal root, there was a large periapical lesion. Figure 11 shows the preoperative CBCT slice. The tooth had preoperative draining via a sinus tract through the buccal plate that the clinician was able to appreciate before initiating the procedure. These images clarify the amount of bone destruction periapically, in the axial view. Recognition of the preoperative indicators enabled the clinician to consider how to best proceed with treatment. Figure 12 shows the postoperative 2D radiograph, which reveals a delicate buccal system and significant anatomy in the palatal canal. There was some extrusion of sealer palatally and at other portals of exit. Figure 13 shows a 3-week postoperative recall 2D radiograph of the case. The draining sinus tract had healed by that point in time.
Figure 14 and Figure 15 show the preoperative digital images for another case with a necrotic pulp. In the preoperative 3D CBCT volume, the clinician observed that the mesiobuccal system, distobuccal system, and palatal system all communicated. On evaluating the mesiobuccal system, the clinician observed anastomoses between the canals. The clinician sought to employ a conservative approach to treating the case. Figure 16 and Figure 17 show the postoperative scans wherein it can be seen that the clinician practiced "directed dentin conservation" (a term attributed to Dr. David Clark and Dr. John Khademi and perpetuated by Dr. Eric Herbranson).12 The only mechanical objective not illustrated by this case is the continuous tapering preparation. Overall, the original root canal system anatomy was maintained and the foramen was kept as small as practical. Figure 18 shows an inverted postoperative radiograph that better illustrates both of these principles.
Figure 19 and Figure 20 illustrate a premolar in which the condition of the pulp was initially misdiagnosed and the patient was referred for restorative work. She returned within a few months, explaining that her tooth hurt. The clinician found that the pulp of tooth No. 12 was necrotic and the tooth had multiple portals of exit and multiple lesions of endodontic origin adjacent to these portals of exit. Figure 21 shows the postoperative 2D radiograph of the tooth after multisonic technology was used to clean and debride the microanatomy.
Advantages of the Technology
In the authors' experience, the multisonic procedure does not take appreciable additional time and, in most cases, can be completed in a single-visit appointment. Clinician, staff, and patient fatigue are noticeably decreased because the process requires less time in shaping/preparation of the root canal system. In lieu of shaping of the root canal system, the clinician's objective is solely to create a pathway to allow the multisonic technology to deliver degassed irrigants to the entire root canal system. The potential for instrument fatigue is reduced because the clinician does not attempt to enlarge the systems significantly beyond the natural anatomy. Instrument stress is lessened, resulting in fewer separated instruments and reduced anxiety for both clinician and staff. There is decreased schedule disruption and reduced loss of valuable tooth structure.
Employment of this technique alleviates the need for multiple instrument passage and repeated recapitulations. As a result, this procedure dramatically lessens the production of the smear layer,11 leading to cleaner systems and more thorough debridement.
The technology involves a less-invasive technique with smaller, more conservative shapes.1 Less patient time is required because it is predominantly a single-visit procedure. The authors have found that only rarely will a case require placement of calcium hydroxide or an intra-appointment medicament. Postoperatively, the procedure results in less pain, less sensitivity, no swelling, and little to no discomfort; over-the-counter non-narcotic anti-inflammatory medications are all that are necessary postoperatively for most patients.
Conclusion
Success rates for endodontic procedures can be quantifiably and qualitatively improved with the use of new technology. Multisonic treatment advances root canal therapy and supports improvements to endodontic outcomes for patients. It accomplishes this through a far more conservative and thorough method than traditional root canal procedures. Using this modality, the clinician can achieve the five mechanical objectives determined initially by Schilder. This allows the clinician to transition from a sense of "cleaning and shaping" to "preparing" the root canal system. Overall, success can be measured by the reduction of clinical fatigue, a decrease in discomfort for the patient and improved healing rates, enabling the clinician to provide a higher level of care that better addresses the complexity of the root canal system.
References
1. Sigurdsson A, Garland RW, Le KT, Woo SM. 12-month healing rates after endodontic therapy using the novel GentleWave System: a prospective multicenter clinical study. J Endod. 2016;42(7):1040-1048.
2. Sigurdsson A, Le KT, Woo SM, et al. Six-month healing success rates after endodontic treatment using the novel GentleWave System: the PURE prospective multi-center clinical study. J Clin Exp Dent. 2016;8(3):e290-e298.
3. Hess W. The Anatomy of the Root-Canals of the Teeth of the Permanent Dentition, Part 1. New York: William Wood and Co.; 1925.
4. Schilder H. Cleaning and shaping the root canal. Dent Clin North Am. 1974;18(2):269-296.
5. Ruddle CJ. WaveOne: helpful hints. The Ruddle Report. http://www.endoruddle.com/blogs/show/20/waveone-helpful-hints. Published May 9, 2012. Accessed November 27, 2017.
6. Van der Sluis LWM, Shemesh H, Wu MK, Wesselink PR. An evaluation of the influence of passive ultrasonic irrigation on the seal of root canal fillings. Int Endod J. 2007;40(5):356-361.
7. Haapasalo M, Wang Z, Shen Y, et al. Tissue dissolution by a novel multisonic ultracleaning system and sodium hypochlorite. J Endod. 2014;40(8):1178-1181.
8. Ma J, Shen Y, Yang Y, et al. In vitro study of calcium hydroxide removal from mandibular molar root canals. J Endod. 2015;41(4):553-558.
9. Charara K, Friedman S, Sherman A, et al. Assessment of apical extrusion during root canal procedure with the novel GentleWave system in a simulated apical environment. J Endod. 2016;42(1):135-139.
10. Macedo RG, Robinson JP, Verhaagen B, et al. A novel methodology providing insights into removal of biofilm-mimicking hydrogel from lateral morphological features of the root canal during irrigation procedures. Int Endod J. 2014;47(11):1040-1051.
11. Vandrangi P, Basrani B. Multisonic ultracleaning in molars with the GentleWave system. Oral Health. May 2015;72-86.
12. Clark D, Khademi J. Modern molar endodontic access and directed dentin conservation. Dent Clin North Am. 2010;54(2):249-273.