You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The ADAA has an obligation to disseminate knowledge in the field of dentistry. Sponsorship of a continuing education program by the ADAA does not necessarily imply endorsement of a particular philosophy, product, or technique.
Accumulation of dental data provides the foundation for comprehensive dental care. Alginate impressions and study models have been used in dentistry for years, primarily to aid in diagnosis and treatment planning. Alginates are elastometric by nature and offer the flexibility and duplicating properties to obtain an accurate impression. These impressions are poured up in gypsum to obtain models or casts. Study models are frequently used for presentation purposes and as a visual aid for patient education. These models provide excellent legal documentation and serve as one component of the permanent record of a patient's oral condition. Study models also provide occlusal representation to identify Angle's classification of (mal)occlusion, which defines the relationship of the maxillary and mandibular teeth in the sagittal plane. Additionally, they provide recognition of wear patterns, missing teeth, drifting teeth, actual size reproductions of anatomical structures including tooth size, shape, positions, gingival margins, interdental papillae, and the freni. Alginate impressions and study models are a valuable adjunct in providing optimal patient care.
Alginate
Alginate is an elastic impression material made from marine kelp. It is also composed of sodium alginate, calcium sulfate and retarders. It is used to take primary or preliminary impressions. This colloidal material forms a gel when the powder is mixed with water. It solidifies into an elastic mass capable of producing a negative reproduction of the oral cavity (an impression). It is sometimes referred to as an irreversible hydrocolloid because once it is mixed a chemical reaction occurs preventing it from returning to its original state of powder and water. Alginate impressions are taken to obtain diagnostic study models, which are the positive reproductions of the teeth and surrounding structures. They are also used but not limited to the fabrication of whitening trays, nightguards, and sportsguards. Alginate is the most universally utilized impression material in dentistry. The following are characteristics of an ideal alginate impression material:
• cost effective
• easy to mix
• adequate flow properties
• non-toxic or irritating
• sufficient strength to avoid tearing material upon removal from the mouth
• acceptable working and setting times
• compatible with gypsum products
• patient acceptability
• adequate shelf life
Packaging
Alginate impression powder is packaged in bulk canisters, one-pound poly bags or pre-weighed single use packages. It is recommended that the powder in the poly bag be transferred into an airtight canister after its initial opening. It is cost effective to purchase alginate in bulk. However, the individual unit dose package offers convenience, accuracy and extended shelf life. It is important to store alginate in a cool, dry area in an airtight container to prevent moisture contamination and prolong the shelf life. Keep in mind that exposures to atmospheric humidity will adversely affect the setting time and markedly decrease the shelf life of alginate. Therefore, alginate canisters should never be left opened or without the lid tightly secured.
Setting Times
Alginate may be purchased in regular, fast and extra fast set varieties. These set times control the working time and the setting time of the material. The working time is the actual time permitted to spatulate the alginate, load the tray and seat the tray in the mouth. The setting time is the amount of time necessary for the alginate to become an elastic mass prior to the tray removal from the mouth. The ADA specification Type 1/Fast Set has a working time of one minute and a setting time of 1-2 minutes. The ADA specification for Type II/Normal Set has a working time of 1-2 minutes and a setting time of 2-4 minutes. The temperature of the water can alter the working and setting times. Ideally, the water temperature should be 73 degrees F or as close to room temperature as possible. An increase in the water or powder temperature decreases the working and setting times, while a decrease in the water or powder temperature increases the working and setting times. It is recommended that a dispensing bottle be filled with water and held at room temperature to provide product consistency. Improper water/powder ratios can also affect the setting time.
Flavoring the Impression Material
Flavoring the impression material makes the procedure more palatable for the patient. Bubble gum, grape and mint are examples of flavors that may be already incorporated into the powder. For unflavored alginates, flavored liquid drops can be added to the water before mixing the alginate. Offering the patient a choice of flavors often gives the individual a feeling of control. This can enhance the patient's cooperation level, thus producing a pleasant experience.
Properties of Powder
Alginate powder may be supplied in regular or dustless forms. Dustless powder is manufactured in an effort to reduce harmful effects to the operator. However, this does not eliminate the need to wear Personal Protective Equipment (PPE) during this procedure. The operators must protect themselves from adverse reactions by wearing personal protective equipment, such as masks, protective eyewear, gowns and gloves, when handling alginate. Without the use of PPE, minute dust particles may be inhaled into the lungs. Prolonged exposure may lead to respiratory problems and/or allergic reactions. The dust can also migrate behind contact lenses and irritate the eyes. The manufacturers of alginate must supply Safety Data Sheets (SDSs). In accordance with OSHA's regulations, the employer is required to maintain SDS sheets in a reference file for employees to access at will. The operator should read the SDS sheets prior to handling alginates, paying special attention to the Health Hazard Data section (Figure 1 and Figure 2).
Disinfecting Protocol/Technique
Antimicrobial agents are incorporated into some brands of alginate but do not substitute for disinfection. Rinse the impression under gently running, room temperature tap water. Spray the impression and tray with an immediate-level hospital grade (capable of killing tuberculocidal activity) disinfectant of choice. (The most accurate casts are associated with disinfection of alginate impressions by spray rather than by immersion.) Place the sprayed impression in a plastic bag, seal the bag tightly, and allow the impression to remain for the amount of contact time recommended by the manufacturer. A label can be affixed to the bag for proper identification. After the required amount of time, remove the impression from the bag and, under room temperature tap water gently rinse again. Pour according to the manufacturer’s directions. IMPORTANT: If disinfection of the impression is not completed properly, the gypsum cast will be contaminated and capable of transmitting disease.
Following the manufacturer’s instructions for disinfectant contact time lessens the opportunity for distortion of the impression, whether using the spray or immersion technique. Dehydration causes distortion which can be easily controlled by pouring up the alginate impression according to the manufacturer’s directions. Once the impression is disinfected and rinsed, it should be poured at once. All alginates are subject to shrinkage from dehydration. If the impression cannot be poured at once, the impression must by wrapped in a wet paper towel with moist cotton rolls over the occlusal and incisal edges and be held in a moist environment (sealed plastic bag) until it can be poured. Ideally alginates should be poured within 30 minutes for best results. If this is not possible, it can be stored in a holding solution, Extend-A-Pour®, for up to thirty days.
Chromatic Alginates
Alginate may be manufactured with chromatic agents that have color indicators in the powder. The color of the mix changes throughout the manipulation of the product. For example, the white powder may change to a deep purple during the mixing phase, turn pink for insertion into the tray and then turn white when the tray is seated. These color changes alert the operator when to end spatulation, when to fill the tray and when the alginate has set. This built-in indicator is an excellent guide for the operator to gauge the various stages of the procedure. The tray does not have to be seated until the last color change, thus reducing the amount of time the tray remains in the patient's mouth. This feature is particularly important for the patient with gagging tendencies. These color changes vary with each manufacturer and may vary based upon the pH of the water used.
Manufacturer's Specifications
It is imperative to follow the manufacturer's specifications for manipulation and use of alginate. Avoid interchanging the powder and water measuring devices from various manufacturers as these devices vary and will affect the accuracy of the mix.
Armamentarium/Supplies and Equipment
The following supplies and equipment are necessary for taking alginate impressions:
• Basic set-up
• Room temperature water and powder
• Water measuring device
• Flavor drops (optional)
• Alginate powder
• Powder measuring device
• Mixing bowls
• Wide blade spatulas
• Maxillary and mandibular impression trays
• Adhesive (optional)
• Beading/utility/rope wax
• Bite registration material
• Disinfectant
• Paper towels/emesis basin
• Plastic bag
• Waterproof pen for patient identification purposes
• PPE for operator
Patient Preparation
Seat patients in an upright position and don a patient napkin to prevent compromising the patient's clothing. A brief oral examination is necessary prior to taking an alginate impression. The purpose of this exam is to inspect the oral cavity for debris, which should be removed prior to taking the impression. At this time, the operator should examine the palatal region for size, height and possible maxillary or mandibular tori. This will alert the operator to adjust the amount of alginate required for full anatomical coverage, i.e. if the palate is shallow, the operator should remove excess alginate material to avoid gagging the patient. Conversely, patients presenting with a high palate will require additional alginate material in this area to prevent voids. Also at this point, it is imperative that the patient takes out any removable dental appliances, oral piercings or grills. The operator should observe the lip area for dryness and chapping to see if it is necessary to lubricate the lips with petroleum jelly for the patient's comfort. Ask the patient to rinse with mouthwash to reduce the number of microorganisms in the oral cavity, as well as minimize air bubbles that can be produced by saliva.
Paper towels or tissues and an emesis basin are placed within the operator's reach in the event of a gagging episode and subsequent vomiting accident. Explain the procedure to the patient. The operator may ask, "Have you ever had impressions taken before?" Observe the patient's verbal and nonverbal response. Negative responses may indicate a bad prior experience or exposure to preconditioning. Reassuring the patient at this time is crucial. The clinician should display a confident attitude. Convey positive information to assure a successful outcome. Basic instructions can be given at this time, such as telling the patients that the pudding-like material will feel cool, that it will set soon and that deep breathing through the nose will make the procedure comfortable. Not overloading the posterior areas of the tray and removing the impression from the oral cavity as soon as it is set also helps relieve the gag reflex.
Tray Selection
Alginate trays are available in a variety of sizes: extra small, small, medium, large and extra large. Some manufacturers label the trays by number to identify size. The smaller the number the larger the tray. Full maxillary and mandibular trays are supplied in metal, plastic or Styrofoam. Perforated disposable trays are made of plastic and are indicated for “single use.” Perforated trays are recommended because the alginate material flows through the holes, or perforations, which provide a mechanical lock of the alginate to the tray. This mechanical lock ensures that the alginate and the tray are removed from the patient’s mouth as one unit. Solid or perforated metal impression trays must be cleaned, packaged and sterilized prior to reuse. The operator should try each mandibular and maxillary tray in the patient’s mouth to ensure a proper fit before the alginate impression is taken. The impression tray “try in” also provides the patient with a preview of how the tray will fit and feel once it is placed in the oral cavity. NOTE: All trays that are tried in the patient's mouth but do not fit correctly must be sterilized prior to restorage.
Criteria for tray selection includes:
• Trays should extend distally to cover the maxillary tuberosity and cover the mandibular retromolar pad for maximum anatomical reproduction.
• Tray height should fully cover the length of anterior and posterior teeth.
• Tray should extend beyond the facial aspect of the teeth with a few millimeters of space between the tray and soft tissue.
• The tray size should be comfortable for the patient and allow for any tori that are present.
If tori are present when using a metal tray, bend the lingual aspect of the tray up so the tray does not come into contact with the tori. If using a plastic tray, trim away the area of the tray that would come in contact with the tori.
Adhesives
When using plastic trays, it is recommended that an alginate adhesive be used. Alginate adhesives are supplied in brush-on or spray-on form. It is recommended that the adhesive be placed inside the tray 5-10 minutes prior to the insertion of the mixed alginate material. The purpose of the adhesive is twofold: 1) the adhesive holds the impression material to the tray so that the tray and alginate come out of the patient's mouth as one unit and 2) to prevent distortion of the impression by securing the alginate tightly against the side of the tray.
Utility/Beading Wax
Utility/beading wax (sometimes referred to as periphery/rope wax) may be used to customize the tray for patient needs. Wax may be added to the borders of the tray to extend its length or height. The anterior region of the tray may be lined with two utility/beading ropes of wax and three utility/beading ropes of wax to maximize anatomical coverage in the vestibular and freni areas. Patients presenting with high palates can have wax placed in the palatal area on the inside of the tray. This will compensate for the high palate and will eliminate voids in the palatal area of the impression. Wax may be placed around the tray periphery to protect and cushion the soft tissues in the oral cavity. The placement of utility wax on the posterior region of the maxillary tray prevents excessive alginate from flowing down the throat; this will help prevent the activation of the gag reflex.
Patients With a Gag Reflex
There are several options to help with the gagging patient. These include:
• Remain positive and in control of the situation
• Make sure the impression tray is the smallest you can use without compromising the required anatomical coverage
• Seat patient upright
• Remind patient to breathe through their nose
• Always take the mandibular impression first
• Psychology - give directions to distract the patient. Example: "lift your left arm" or "lift your right leg"
• Use slightly warmer water for a quicker set time
Alternatives to Hand Mixing
Alternatives exist for mixing alginates other than manual manipulation of the impression material. The Alginator and the Vac-U-Mix automatically mix the alginate through the use of motorized electrical equipment.
The Alginator is a small countertop piece of equipment (Figure 3) that produces consistent uniform and homogeneous alginate mixes. Instead of manual hand spatulation, the Alginator rotates the bowl automatically at 300 times per minute. Read the manufacturer's operating instructions before using this equipment.
Steps to use Alginator - the following are general guidelines to follow:
1. The flexible mixing bowl is guided into the Alginator and turned clockwise to lock it in position.
2. Water and powder are added to the bowl and blended together by hand.
3. The Alginator is turned on.
4. The spatula is held by the operator and pressed along the side of the bowl while it automatically rotates. Keep the material in the bottom half of the bowl. Otherwise, the alginate material will expel everywhere!
5. Stop and wipe off the spatula.
6. Resume mixing by flexing the flat portion of the spatula blade against the center and side of the bowl until mixed.
7. Collect the mixed alginate on the spatula and prepare to load the impression tray.
The Whip-Mix Vac-U-Mixer may also be used to mix alginate impression material (Figure 4). The use of this power-driven equipment insures a bubble-free mix because air is sucked from the mix by means of vacuum tubing. The self-contained mixing bowl and lid, which is attached to the machinery, will automatically mix the alginate. Refer to the manufacturer's operating instructions before using the Vac-U-Mixer.
Steps to use Vac-U-Mixer - the following steps are general guidelines:
1. Rinse the bowl and lid assembly. A separate bowl should be used for alginates only. Shake off excess water.
2. Fill the bowl with water and alginate powder according to the manufacturer's instructions.
3. Hand spatulate to incorporate all powder particles into the water.
4. Place the lid with paddle on the bowl and twist the lid so the tabs lock together.
5. Attach the vacuum by placing the metal nozzle at the end of the vacuum hose into the opening located on top of the lid.
6. Grasp the bowl and lid as one unit and insert the drive nut into the drive chuck for automatic start.
7. Turn the manual switch to "ON" so the pump continues to run after the bowl is disengaged.
8. The suggested mixing time is 12-15 seconds at low speed.
9. Break the vacuum immediately and use mixed alginate in the conventional manner.
10. Let the vacuum pump run for an additional minute to purge water vapor and allow the unit to automatically re-oil.
Alginate Alternatives
Other alginate alternatives are manufactured in cartridge delivery systems or automix machines and are becoming increasingly popular. AlgiNot® is an example and may be used for:
• Preliminary impressions
• Provisional crown and bridge impressions
• Study model impressions
• Opposing dentition impressions
• Orthodontic model impressions
• Impressions for sports guards, snore guards, bleaching trays or other traditional alginate
Advantages to these systems are appealing as there is no manual mixing, ease of use, dustless, dimensionally stable, easy clean up, and the ability to disinfect and re-pour. The mixed alginate is placed directly in the tray via the tip thus eliminating the need for a bowl and spatula, canisters of alginate, and powder and water measuring devices (Figure 5).
Mixing Techniques
Mandibular Tray
Inspect all materials for cleanliness. All disinfected bowls and spatulas should be rinsed and dried before use. This removes the disinfectant residue, which may become incorporated in the mix and cause an allergic reaction for the patient.
Always take the mandibular impression first. The patient is less likely to gag on the lower, thus instilling a positive experience.
Steps for mixing mandibular tray - the following steps should be used to obtain a full mandibular arch impression:
1. Place two measures of room temperature water into the bowl.
2. Fluff the powder canister. A gentle tumble is all that is necessary. Back and forth motions are not recommended because this will condense the alginate within the container, thus disrupting the water/powder ratio.
3. Place two level scoops of powder into the bowl of premeasured water.
4. Stir the water and powder until all the powder particles have been moistened.
5. Mix the alginate by pressing it along the sides of the bowl. Be sure to condense the mixture between the bowl and spatula to remove air bubbles and create a creamy, homogeneous mix. (As an alternative to hand mixing, use an Alginator or a Whip-mix as previously discussed.)
6. Collect the mixed mass of alginate into one area along the edge of the mixing bowl. NOTE: The inexperienced operator may find it necessary to take a small amount of the mixed alginate and place it in the oral vestibule and/or occlusal surfaces to insure total anatomical coverage and accuracy without air bubble entrapment.
7. Take half of the mixed alginate and quickly load it into the mandibular tray from the lingual aspect while firmly pressing down towards the bottom of the tray.
8. Collect the second half of the mixed alginate and fill the opposite side of the tray in the same manner.
9. Wet a gloved finger with cool water and pass the fingers over the tray with a light force to create a smooth finish (Figure 6).
Seating the Mandibular Tray. After the impression tray has been satisfactorily fit to the patient's mouth, utility wax may be placed around the periphery of the tray for reasons already cited. After the alginate has been mixed and the tray has been loaded, the tray is now ready to be inserted into the patient's mouth.
Steps for seating mandibular tray - the following guidelines should be followed for seating a mandibular tray in the oral cavity.
1. Have the patient seated in an upright position.
2. The operator should be positioned in front of the patient for proper seating of the impression.
3. Instruct the patient to open his or her mouth.
4. Opening too widely eliminates the elasticity of the cheek, which is necessary for properly seating the impression.
5. Retract the cheek with an index finger to provide visibility for placement of the tray.
6. Insert the tray from the side and then center it over the arch (Figure 7). The midpoint of the impression tray handle should be perfectly aligned with the patient's midline while the tray handle maintains a parallel position to the floor.
7. Press down on the posterior portion of the tray first and continue to the anterior in one smooth motion.
8. Roll the lower lip up over the anterior portion of the mandibular tray for finer anatomical detail.
9. Instruct the patient to elevate his tongue and then relax it. This technique enhances a more detailed duplication of the lingual aspect.
10. Firmly hold the tray with equal bilateral pressure in the patient's mouth while waiting for the final set of the impression material. The firm, equal pressure on both sides of the mouth will prevent distortion (Figure 8).
11. Prior to the removal of the tray, the operator must check to see if the material has set. The operator can easily test for the final set by simply pressing the alginate in the mixing bowl or in the patient's mouth with the operator's finger to observe that no deformation or dent occurs in the material.
Removal of Mandibular Impression. All alginates should be removed in one quick snap-out motion to prevent distortion of the impression. The operator should insert the index finger into the mucobuccal fold of the patient's vestibule while tucking the index finger under the periphery of the tray and push in an upward motion. This will enable the operator to break the alginate seal that conforms to the teeth while exerting a firm lifting motion with the opposite hand. The tray should be held with the operator's thumb under the tray handle and the fingers resting over the handle to prevent possible trauma to the maxillary anterior teeth. Exert a firm lifting uniform motion; snap the impression tray up off of the mandibular arch while protecting the maxillary teeth with the opposite hand. Never rock or wiggle the tray to remove it from the dental arch, as this is certain to create an overall distortion of the impression.
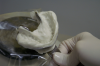
Inspection of Impression. The alginate impression should be inspected immediately upon its removal from the oral cavity (Figure 9). The purpose of inspection is to observe:
• a smooth homogeneous set (a grainy appearance will show if spatulation was inadequate).
• that the impression did not separate from the impression tray.
• coverage of the total dentition and its accompanying freni, vestibular, retromolar, and tuberosity areas.
• presence of voids and air bubbles.
• no evidence of tray visibility in the incisal and occlusal surfaces; sharp anatomical detail
• presence of blood, saliva and debris.
Disinfection and Storage. All impressions must be disinfected before being removed from the treatment area.
Steps in disinfection of impression - the following steps should be taken:
1. Immediately after inspection is completed, rinse the impression for thirty seconds under slow running, room temperature tap water to minimize aerosolization and splatter. Check to see that all blood, saliva, and debris have been removed.
2. Spray disinfectant completely covering all areas of the impression and tray; or use the immersion method according to the manufacturer's recommendations.
3. After disinfection, rinse the impression under room temperature tap water for thirty seconds.
4. Place disinfected impression, wrapped in a moistened paper towel in a plastic bag for storage until poured. (Bags can be purchased commercially or headrest covers may be used.)
5. Ideally, the impression should be poured in gypsum within 30 minutes to prevent dimensional distortion. Impressions may be poured in-house or picked up by a commercial dental laboratory. It is inadvisable to mail study model impressions to a laboratory. The time elapsed between the actual impression taking and subsequent pouring of the impression will result in dimensional distortion.
6. Patient identification should be made by labeling the bag with the patient's name with a waterproof marker.
7. A laboratory prescription should be completed with a waterproof pen and stapled to the storage bag. This may also be accomplished with an online order wizard script.
Maxillary Tray
Once the impression tray has been satisfactorily fit to the patient's mouth, the operator should dry the trays and affix the beading wax to customize the tray prior to mixing the alginate. The maxillary impression is always taken after the mandibular impression has been obtained.
Steps for mixing maxillary tray - the following steps should be followed for mixing a full maxillary impression:
1. Place three measures of room temperature water into the mixing bowl.
2. Fluff the powder canister. A gentle tumble is all that is necessary. Back and forth motions are not recommended because this will condense the alginate within the container, thus disrupting the water/powder ratio.
3. Place three level scoops of powder into the bowl of premeasured water.
4. Stir the water and powder until all the powder particles have been moistened.
5. Mix the alginate by pressing it along the sides of the bowl. Be sure to condense the mixture between the bowl and spatula to remove air bubbles and create a creamy, homogeneous mix. (As an alternative to hand mixing, use an Alginator or a Whip-mix as previously discussed.)
6. Collect the mixed mass of alginate into one area along the edge of the mixing bowl. The inexperienced operator may find it necessary to take a small amount of the mixed alginate and place it in the oral vestibule and/or occlusal surfaces to insure total anatomical coverage and accuracy without air bubble entrapment.
7. Take all of the mixed alginate and quickly load it into the maxillary tray from the palatal aspect while firmly pressing down towards the bottom of the tray. This technique will prevent voids and air bubbles in the impression.
8. Wet fingers with cool water and pass the fingers over the tray with a light force to create a smooth finish.
Seating the Maxillary Tray. After the alginate has been mixed and the tray has been loaded, the tray is now ready to be inserted into the patient's mouth.
1. Have the patient seated in an upright position. The patient's occlusal plane should be parallel to the floor.
2. The operator should be positioned at the patient's side for proper seating of the impression tray.
3. Instruct the patient to open his or her mouth. Opening too widely eliminates the elasticity of the cheek, which is necessary for properly seating the impression tray.
4. Retract the cheek with the index finger to provide visibility for placement of the tray.
5. Insert the tray from the side of the patient's mouth and then center it over the maxillary arch. The midpoint of the impression tray handle should be perfectly aligned with the patient's midline while the tray handle maintains a parallel position to the floor.
6. Press down on the posterior portion of the tray first and continue to press anteriorly in one smooth motion. This will force the excess alginate material forward to obtain maximum vestibular anatomy and simultaneously eliminate the flow of alginate down the patient's throat.
7. Roll the upper lip up over the anterior portion of the maxillary tray for finer anatomical detail.
8. Firmly hold the tray with equal bilateral pressure in the patient's mouth while waiting for the final set of the impression material. This firm bilateral pressure will prevent distortion of the impression. The operator should be positioned at the patient's side while maintaining a "headlock" for stability. Instruct the patient to tuck his chin downward as he tips his head forward and holds still.
9. The operator can easily test for the final set by simply pressing the alginate in the mixing bowl or in the patient's mouth with a finger to observe that no deformation or dent occurs in the alginate impression material.
Removal of Maxillary Tray. Maxillary impressions should be removed in one quick snap-out motion to prevent distortion of the impression material. The operator should insert the index finger into the mucobuccal fold of the patient's vestibule while tucking the index finger over the periphery of the tray and pull in a downward motion. This will enable the operator to break the alginate seal that conforms to the teeth while exerting a firm downward uniform motion with the opposite hand. The tray should be held with the operator's thumb over the tray handle and the fingers resting under the handle to prevent possible trauma to the mandibular anterior teeth. Exert a firm downward motion; snap the impression tray off of the maxillary arch. Never rock or wiggle the tray to remove it from the dental arch, as this is certain to create overall distortion of the impression.
As with the mandibular impression, the maxillary impression must then be inspected for the purposes previously cited. At the same time, guidelines for disinfection and storage should be implemented. Note: Regular alginate impressions should be poured within 30 minutes to avoid distortion. Chromaticity alginates traditionally allow more time prior to pouring model...refer to the manufacturer’s directions. It should be noted that both impressions and the wax bite registration should be packaged together in one bag to avoid error.
Bite Registration
A bite registration is an occlusal representation of how the maxillary and mandibular teeth intercuspate. Bite registration is essential for the subsequent articulation of the maxillary and mandibular study models. The bite registration is routinely obtained immediately following the maxillary impression. If the bite registration is taken prior to tray selection, the registration can aid in choosing the appropriate size of the impression tray. This time-saving technique eliminates the need for the sterilization of improperly sized trays.
Options for Obtaining the Bite Registration
The operator instructs the patient to practice opening and closing in centric relation in preparation for obtaining an accurate bite registration. There are currently a variety of ways to obtain the bite registration.
It may be accomplished via: Baseplate wax method — Baseplate wax is manufactured in 3"x 5" sheets and sold by the box. The 3"x 5" sheet may easily be cut with a lab knife to accommodate the width of the dental aches. The custom-sized baseplate wax may be cut in arch form or folded in half and used in rectangular form to increase the stiffness. It is placed in the patient's mouth after it has been softened in lukewarm water. It is placed over the occlusal surfaces of either dental arch, depending on the operator's preference. The patient is instructed to bite normally into the wax in centric occlusion. The patient's teeth should remain embedded in the wax while the wax cools and hardens. The operator may choose to accelerate the cooling and hardening process by applying air from the air/water syringe. Once this is accomplished, the operator carefully removes the wax bite registration from the oral cavity while making every attempt to avoid distorting it. It is then inspected for accuracy and immediately disinfected by spraying or immersion.
Bite waxes are manufactured in the shape of the dental arch with foil sandwiched between the pieces of wax. It must be softened under hot water. It is placed over the occlusal surfaces of either dental arch (Figure 10). The patient is instructed to bite normally into the wax in centric relation. It remains in place until it has cooled and hardened (Figure 11). Once this is accomplished, the operator carefully removes the wax bite registration from the mouth. It is inspected for accuracy and appropriately disinfected.
Elastic bite registration material is manufactured for use with cartridge delivery systems. The bite registration material is injected onto the mandibular occlusal surfaces. The patient is directed to occlude in centric relation. The material remains in place until it has achieved a rubberized state. It is then carefully removed from the oral cavity, inspected for accuracy and appropriately disinfected.
Clean Up
Before adding material to the mixing bowl, to help with easier and faster clean up slightly coat the mixing bowls or metal impression trays with non-stick cooking sprays. There are also lubricating spray or wipes available from your dental supply company. Check with your local representative.
Gypsum
Gypsum is a naturally occurring mineral mined in various parts of the world. In its purest form it is known as calcium sulfate dihydrate and water. Manufacturers process the mined gypsum by heating it in kilns to temperatures between 230-250 degrees F. This procedure eliminates the water content from the gypsum, thus producing calcium sulfate hemihydrate. It is subsequently distributed for commercial use. Calcium sulfate hemihydrate is the actual mineral gypsum product used in dentistry to fabricate diagnostic study models or positive reproductions of the oral cavity. The gypsum powder, which may be plaster, stone, improved stone or investment materials is mixed with water until a smooth, creamy mix is achieved and allowed to solidify or harden into a rigid mass. The setting of the gypsum is achieved through the "Loss of Gloss" phenomenon. This occurs during the initial setting of the gypsum cast between the first 7-13 minutes. An exothermic chemical reaction occurs when the shiny plaster finish takes on a dull appearance. If the operator's skin comes in contact with the plaster, he or she will feel heat, which is the result of a rise in temperature during hardening through the exothermic process. The final set of plaster takes place within 45-60 minutes. Plaster is the recommended choice of gypsum products for use in dentistry for study model construction for presentation purposes. When additional strength is a concern, stone may be used for increased durability, i.e. stone is advisable for procedures such as the fabrication of whitening trays, nightguards or sportsguards.
The following are desired characteristics of gypsum products:
• Compatibility with impression materials
• Acceptable working and setting times
• Adequate flow properties
• Ease of manipulation
• Reasonable cost
• Adequate shelf life
• Acceptable strength and durability
• Excellent dimensional stability
• Capable of duplicating fine detail of hard and soft tissues
Packaging
Gypsum plaster is packaged in 25-50 pound boxes, 100-pound drums and in pre-packaged envelopes. It is imperative that gypsum powder be stored in an airtight container to prevent moisture contamination, which interferes with the set of the material. It is recommended that all gypsum products be stored in a cool, dry area in an airtight container to prolong the shelf life of the material. It should be noted that gypsum left in open containers will readily absorb moisture and humidity, which will markedly decrease the shelf-life and will adversely affect the setting properties of the material.
Setting Times
Setting time may be defined as the amount of time required from the initial incorporation of gypsum powder with water until the material hardens or sets. An exothermic chemical reaction gives off heat during the hardening of gypsum. Placing a hand on the plaster and feeling warmth will evidence this exothermic reaction. It is recommended that once poured into the impression, gypsum should remain undisturbed for 45-60 minutes to completely set before separating the model from the impression. Although mixing bowls should be disinfected, check once again to see if any hardened gypsum is still present in the mixing bowl. Unclean bowls will adversely effect the setting times, the consistency and the overall strength of the gypsum material.
Gypsum setting times may be influenced by the use of accelerators and retarders.
The following are examples of accelerators that hasten the set of gypsum:
• Increase in water temperature above 68 degrees F when mixing the plaster
• Increase in room temperature or humidity
• Faster rate of spatulation time will hasten the setting time
• Pinch of table salt (sodium chloride)
• Decrease the amount of water specified by the manufacturer
The following are examples of retarders that allow for more working time and increase the setting time:
• Cooler than room temperature water
• Decrease in room temperature and humidity
• Slower rate of spatulation will slow down the setting time
• Borax (calcium salts) in small concentrations
• Increase in the amount of water specified by the manufacturer making a thinner mix, although this weakens the cast
Properties of Dental Plaster Powder
Dental plaster or Plaster of Paris powder particles are jagged and irregular in shape, porous, and vary in particle size. Plaster is usually white, which is desirable for presentation purposes. It should be stated that dental model plaster is the weakest of all dental gypsum. Therefore, care must be taken when handling study casts during consultations. The operator must protect himself when handling gypsum products by wearing Personal Protective Equipment (PPE). Prolonged exposure may lead to respiratory problems and eye irritation. SDS should be reviewed prior to handling the product while paying close attention to the Health Hazard Data section.
Armamentarium/Supplies and Equipment
The following supplies and equipment are necessary for pouring impressions for study model construction:
• Impressions
• Room temperature water
• Water measuring device
• Model plaster powder
• Powder measuring device
• Mixing bowl - Debubblizer
• Stiff bladed spatula
• Laboratory vibrator to be covered with clear plastic bag for clean up purposes
• Bracket tray cover for workbench cleanliness
• Model base accessory items, i.e. boxing wax, prefabricated base formers
• Tiles for inversion technique
• Laboratory knife
• PPE for operator
Laboratory Preparation of the Impression
To prepare the alginate impression for pouring, the following must be done immediately before pouring to reduce shrinking of alginate material:
1. Remove moist paper towels from alginate impression.
2. Remove moist cotton rolls from occlusal and incisal areas.
3. Inspect impression to ascertain required coverage for indicated use. (check for unwanted bubbles, tears, voids, etc.)
4. Gently shake the impression over the lab sink in order to remove excess moisture.
5. Spray the impression with a commercially manufactured debubblizer. This serves to reduce the surface tension, thereby enhancing the flow of the plaster and reducing the number of air bubbles on the cast's surface.
6. Gently air-dry the impression.
7. Inspect impression to confirm that all obvious moisture has been removed.
Gypsum (Plaster) Hand Mixing Technique
It is important to follow the manufacturer's instructions for water/powder ratios. The use of a Whip Mix Vac-U-Mixer eliminates the need for hand mixing. (The Alginator may also be used for mixing gypsum provided great care is taken to avoid splashing.) The generally recommended W/P ratio for hand mixing plaster is usually 50:100 or simply phrased one-part water to two-parts powder. An example of this W/P ratio would be 1/2 cup of water to 1 cup of powder. If you are using stone the ratio is usually 30:100. Dental gypsum is mixed with water to obtain a creamy, homogeneous consistency.
The following list outlines the steps to be followed for successfully mixing plaster by hand.
1. Assemble all armamentarium, supplies and equipment.
2. Place premeasured, room temperature water into the clean mixing bowl.
3. Measure twice as much plaster powder as used for water.
4. Gradually sift/add powder into water to prevent air entrapment.
5. Allow the wetting of powder particles.
6. Stir the powder and the water together.
7. Hand spatulate the mix at 120 RPM for one minute in one continuous direction to avoid air entrapment. As always, the manufacturer's instructions should be strictly followed.
8. Place the bowl of mixed plaster on the platform of the vibrator that has been covered with plastic.
9. Secure the bowl and mix with one hand while turning the vibrator on "low" speed.
10. Press the sides of the flexible bowl on the vibrator while observing for the release of air bubbles. If bubbles fail to break from vibration, it may be necessary to mechanically break the bubbles with the spatula.
11. Once this has been accomplished, remove the bowl from the vibrator for subsequent pouring.
Pouring the Anatomical Portion of the Study Models
The anatomical portion of the study model is always poured prior to the base/art portion of the cast.
Leaving the vibrator on low speed, the operator will proceed with the following steps:
1. Hold the impression by the handle while resting the base of the impression tray at an angle on the vibrator's platform (Figure 12).
2. Load the tip of the spatula with a small amount (approximately 1/2 teaspoon) of mixed plaster.
3. Start to fill the impression by resting the spatula against one posterior corner (Figure 13).
4. Allow the mix to flow into the occlusal surfaces of the adjacent teeth.
5. Continue to add small increments of mixed gypsum to the same corner as the first increment. Observe the gypsum as it flows down into the occlusal and incisal surfaces.
6. Rotate the tray sideways to force the flow of material into each tooth impression.
7. Once all teeth have been sufficiently filled with plaster, add larger increments of mix until the entire impression is filled. Vibrate a few more seconds.
8. Remove impression from the vibrator.
9. Turn off the vibrator.
10. The study model will begin to set slightly while the operator prepares the base/art portion material for the study model.
Creating the Study Model Base/Art Portion
The base of the study model may be referred to as the art portion of the cast. This area should not exceed 1/3 of the overall height of the cast. The purpose of the study model base is for:
• Aesthetics — adds to the professional appearance of the models.
• Articulation — to properly represent the patient's occlusion and relative anatomical structures.
• Preservation — for ease in handling and storage.
Inverted Technique: A separate mix of gypsum is made with a W/P of 2:5 using the conventional mixing technique already outlined for pouring the anatomical portion impression. This increased W/P provides a thicker mix and stronger model base. A mass of material is placed onto a ceramic tile approximately 1 inch in height. The diameter of the mass should exceed the circumference of the impression to allow for subsequent trimming of the base with appropriate angles. Invert the impression tray or anatomical portion of the cast and place over the (gypsum mass) base material. Using a stiff, wet spatula, mold the plaster to the initial pour, making certain not to imbed the tray in gypsum (Figure 14). Be sure to add gypsum to the heels of the base. The handle should maintain a parallel position to the countertop. Leave undisturbed for 45-60 minutes to allow complete setting of the gypsum. The gypsum will feel warm to the touch during the setting process.
Rubber Model Base Former: A separate mix of gypsum is made with a W/P of 2:5. With the vibrator on low and the rubber base former resting on the vibrator platform, fill the commercial base former with plaster. Invert the initial pour onto the gypsum in the mold making certain that no voids exist between the initial pour and the base material. The advantage of using a model base former is that it eliminates time-consuming model trimming.
Boxing Method: Boxing wax is used to create a wall around the circumference of the unpoured impression to create one unit to be poured. First, the anatomical portion of the impression is poured. Subsequently, the operator continues to fill the gypsum material to the top of the boxing wax. The boxing wax acts like a retaining wall to support the art portion of the cast created in this manner. This wax wall eliminates the need for inverting the poured impression to create a base.
Maxillary & Mandibular Base Former with Handle Slot: The base is obtained by guiding the handle of the impression tray into the base former. A slot in the base former allows the handle to insert through the former. The impression tray fits snuggly inside the former. It is then filled with gypsum in the conventional manner (Figure 15).
Separating the Cast from Impression
The operator should carefully remove the impression tray from the plaster cast without deformation to the model. This is accomplished by placing a laboratory knife between the abutting gypsum and the tray periphery. Next, the knife is gently twisted to loosen or separate the cast from the alginate (Figure 16). The tray is then lifted off in one upward motion. Never rock the tray off the cast as this motion may easily lead to breakage of the teeth.
In the event that the cast does not separate easily from the alginate, recheck the peripheral margins and resume using the knife to gently pry the stubborn area. This situation occurs if the impression was overpoured or overseated during inversion. If concern for breakage is evident, soak the cast in cool water for 10 minutes. This will ease the model separation process.
Trimming the Cast
The purpose of trimming study models is to articulate the maxillary and mandibular arches in occlusion. The models are then ready to sit in proper occlusion for presentation, preservation and storage purposes.
Ideally, study models should be trimmed with a model trimmer (Figure 17) immediately after their separation from the alginate impression tray. The study model should be wet to enhance the ease of cutting the angles of the base on the model trimmer. If several hours have passed from the time of model separation from the alginate impression, it may be necessary to submerge the study models under cool water for 10-15 minutes. A dry model will bind in the model trimmer and leave stone on the cutting wheel. To enhance the professional appearance of the cast, fleck off any imperfections from the moist models by using a small lab knife. Generally speaking, for a Class I or a Class II malocclusion, the maxillary cast is trimmed first. Subsequently, the mandibular cast is set into occlusion by means of the wax bite registration and trimmed to conform to the maxillary cast. It is recommended to trim the mandibular cast first in the presence of a Class III malocclusion. Note: As always, safety first, i.e. all PPE should be worn by the operator during this procedure. Special attention should be given to protect the eyes and the hands during the operation of the model trimmer as well as disinfection of the treatment area and sterilization of any instruments used during the operation of the model trimmer.
The following procedures should be followed for trimming casts:
1. Place the base of the maxillary model on the table of the model trimmer, which is preset at 90 degrees.
2. Turn on the water to the model trimmer. Moderate water flow will enable the rotating.
3. Gently press the base of the cast on the rotating wheel. The base is trimmed parallel to the occlusal plane. Continue applying light force until the base comprises 1/3 of the overall height of the cast. The anatomical portion will comprise the remaining 2/3 of the entire cast. This can be determined by the use of a flexible millimeter ruler by measuring the maxillary model from the base of muco-labial fold to the cusp tip of the canine. The total height of the maxillary cast should be 35 mm. The total height of the mandibular cast will also be 35 mm. The combined overall height of the diagnostic casts will be 70 mm or 2.75 inches in height according to the old Tweed method. The new Tweed, which stands at an overall height of 2.5 inches, may be the practitioner's preference. Repeat the same procedure for the mandibular base (Figure 18).
4. Place the base portion of the maxillary cast on the platform of the model trimmer. Apply light force to cut the heel of the model perpendicular to the midline (Figure 19).
5. Remove the cast from the model trimmer and examine it to see if it sits flat (180 degrees) when placed on the workbench.
6. Hold the side of the maxillary cast on the wheel and trim each side at 65 degrees from the heels. Allow 3-5 mm of space beyond the facial surfaces of the teeth on the cast.
7. Trim the anterior portion of the maxillary cast to form a point at the midline. This should configure to an 85 degree angle. This point will be approximately 5 mm from the labial surface of the maxillary central incisors. The end point should run from canine to canine.
8. While trimming the anterior angles, it is imperative to leave the entire natural anatomical structures intact, i.e. frenum, vestibular area, etc. The anterior cuts should follow the general contour of the anterior teeth, be of equal length, and at the same angle to the sides of the model, be cut to the greatest depth of the vestibule without cutting into the anterior teeth, and end anteriorly at the midline of the maxillary arch.
9. Articulate the maxillary and mandibular cast by means of the wax bite registration.
10. Cut the heel of the mandibular cast to match up with the maxillary cast. Rest the articulated models on the workbench to determine that they sit flat (180 degree angle).
11. Place the articulated models on the model trimmer platform. Trim the sides of the posterior region of the mandibular cast so they are in concert with the slides of the maxillary cast. Allow 3-5 mm of space beyond the facial surfaces of the teeth on the cast.
12. Trim the anterior portion of the mandibular cast to form an arc or a rounded area from the first premolar to the first premolar. Caution should be taken to prevent damaging the incisors.
13. Place the articulated models on the model trimmer platform so that a 60-degree angle can be simultaneously cut at the posterior heel corners (Figure 20).
14. Rest the articulated casts without the bite registration in place, to assess that the trimming process has been completed to satisfaction. Also, confirm that the study models properly represent the patient's current occlusion (Figure 21).
Finishing the Cast
Fill in any visible voids or bubbles on the model surface with a thick mix of plaster and smooth with the gloved fingertip. Let the models dry for 48 hours. Sand the base and sides of the study models with a fine grit sandpaper under slow running water. NEVER sand the teeth or anatomical structures of the casts. The models may now be polished to a high gloss finish to enhance their professional appearance. This may be accomplished through the use of a commercial model luster spray or submersion in a model luster solution for one hour. An alternative to using a commercial model luster product is to entirely submerge the casts in a soapy solution of Ivory flakes and hot water (165 degree F) for one half hour. Finally, buff each cast with a soft, dry, clean cloth to achieve a high glossy appearance.
Labeling and Storage
Each cast must be identified with the patient's full name, the date the impressions were taken and the patient's date of birth. This may be accomplished with an adhesive label that is typed and placed on the heels of the maxillary and mandibular casts 24 to 48 hours after the final finish. Another labeling device is an engraving marker. The patient's engraving information should be completed on the heels of the unfinished maxillary and mandibular casts, i.e. prior to the soaping or luster process.
Diagnostic study models are stored on their bases in labeled boxes. Foam, sponge or bubble pack should be placed between the maxillary and mandibular cast to prevent breakage of the models.
Summary
Be sure to tightly reclose the storage containers that hold the alginate and gypsum products. REMEMBER, humidity, high temperature, moisture contamination and leaving the containers open will markedly decrease the materials shelf life thus, resulting in additional expenditures and increase overhead costs to the facility. Improper storage also adversely affects the setting qualities of these materials. All used equipment should be cleaned and appropriately disinfected prior to being stored. Always follow OSHA recommendations for decontamination. Laboratory sinks should be equipped with a gypsum trap to prevent clogging or back up of the drainpipes. All unused set materials must be discarded in the trash barrel and should never be allowed to enter the sink area. All countertops should be cleaned and disinfected. The area should reestablish its neat orderly appearance.
Glossary
accelerator- any material that hastens or speeds up the chemical reaction of a material; a catalyst
alginate- an irreversible hydrocolloid predominantly used to construct diagnostic study models
anatomical portion- the area of the cast that represents the teeth and surrounding dental anatomy including the oral vestibule and freni
articulation- the contactual relation of the maxillary and mandibular teeth as they intercuspate
art portion- the base that supports the anatomical portion of the diagnostic cast
chromatic agents- ingredients that produce color change
disinfection- the process of reducing the number of disease-producing microbes to a safe level
emesis basin- a kidney shaped receptacle made of plastic or metal
exothermic- a chemical reaction that releases energy in the form of heat
gypsum- a natural mineral found in mines; known as calcium sulfate dihydrate and water
homogeneous- containing properties that are totally uniform and consistent throughout
imbibition- the absorption of water that creates distortion through swelling
loss of gloss- when the shiny appearance of gypsum acquires a dull finish
occlusion- intercuspation of the maxillary and mandibular teeth
retarders- any material that slows down the chemical reaction of a material
spatulation time- the time required for thoroughly mixing alginate or gypsum
study models- the positive reproduction of the oral cavity, which includes the anatomical and art portions
syneresis- the loss of water that creates distortion through shrinkage
working time- the time that elapses between the incorporation of ingredients up to the point just prior to setting
References
Bird, Doni & Robinson, Debbie, Torres and Ehrlich Modern Dental Assisting, 10th edition, St. Louis, MO: Mosby, 2012.
Collin, WJN, A Handbook for Dental Hygienists, 3rd edition, Wright, 1992.
Cottone, Terezhalmy, & Molinari, Practical Infection Control in Dentistry, 4th edition, Media, PA: Williams & Wilkins, 2008.
Dofka, Charline, Competency Skills for the Dental Assistant, 1st edition, Albany, NY: Delmar Publishers, 1996.
Robinson and Bird, Essentials of Dental Assisting, 6th edition, Saunders, 2017
Molinari & Harte, Practical Infection Control in Dentistry, 3rd edition, Lippincott Williams & Wilkins, 2010.
OSAP, From Policy to Practice: OSAP’s Guide to the Guidelines, 2016.
Phinney & Halstead, Dental Assisting… A Comprehensive Approach. Delmar Cengage Learning, 2013.
Tyler, L., Pearson's Comprehensive Dental Assisting, Pearson Education, Inc, 2009.
Wilkins, Esther, Clinical Practice of the Dental Hygienist, 12th Wolters Kluwer, 2016.
About the Authors
Ellen Gambardella, CDA, RDA, M Ed, FADAA
In a nationwide search, Ellen was selected as the “Most Effective Dental Assistant Educator in the United States”. The Massachusetts Dental Society presented her with the “Special Award for Teacher of the Year” and the “Volunteer Auxiliary of the Year” award. She is the recipient of the Goldin Foundation Award for Excellence in Education and the Dr. LeClaire Dental Health Professional Award for innovative and impassioned teaching. The United States Air Force recognized Ellen for her educational support of the 66th Dental Flight and Medical Group. She has been appointed by the Massachusetts Department of Education to develop Dental Assisting teacher licensing examinations. A former faculty member of Tufts and Northeastern Universities, Ellen has lectured nationally and internationally, is an author, and has vast experience in the area of accelerated learning. She has been featured in The Dental Assistant Journal on “Maximizing Efficiency in the Dental Office” and was awarded the title of “Fellow” from the American Dental Assistants Association.
Rita Johnson, COA, RDH, MA Bus
Rita Johnson is a former treatment coordinator in a private orthodontic practice and a former professor at Middlesex Community College, where she received the Outstanding Faculty Recognition Award. Rita is also the recipient of the “Volunteer Contributions for Auxiliaries” award, given by the Massachusetts Dental Society. Rita worked at Brontes Technologies, where she was involved in the research and development of digital orthodontics. She is currently employed by 3M Oral Care Solutions Division where she serves as a Digital Practice Specialist. Rita has written RDH curriculum, authored articles, patented orthodontic products, and has vast experience in the area of practice management.
The editor wishes to thank Michael Durda of Dux Dental for his countless hours editing portions of this manuscript and supplying photographs.