You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The traditional method of treating dental decay in the United States (U.S.) has been restorative dental treatment, which can be expensive, time consuming, and difficult to access for many patient populations.1-4 Silver diamine fluoride (SDF) is an inexpensive, non-invasive, antimicrobial liquid used in several countries to treat carious lesions and decrease sensitivity.1 As of April 2014, a 38% SDF was cleared for marketing as a Class II medical device by the U.S. Food and Drug Administration (FDA) for the treatment of dentinal hypersensitivity.1,5 Marketed as Advantage Arrest™ (Elevate Oral Care LLC, West Palm Beach, FL), SDF has been used in the U.S. (off-label), for the arrest of carious lesions.1,4,5 In October of 2016, the FDA granted the designation of breakthrough therapy to Advantage Arrest 38% SDF as a treatment for arresting dental caries in children and adults.6 This designation is designed to expedite the development and review of drugs that address a serious medical need and is based on preliminary clinical evidence indicating that the drug may demonstrate significant improvement over current therapies.
Previous studies on SDF have focused primarily on its clinical efficacy.2,7-10 Using SDF at 38% concentration has been highly effective in the arrest and prevention of carious lesions.1-12 SDF contains silver ions that act as antimicrobial and bactericidal agents within lesions by destroying bacterial membranes, denaturing proteins, and inhibiting DNA replication.1,13 The fluoride ions in SDF help create fluorapatite, a more acid-resistant enamel which can prevent further demineralization of tooth structure.14 Applying SDF to occlusal, facial, and lingual surfaces has been shown to be successful in arresting caries in multiple clinical trials,1,2,7-10 and its application to interproximal surfaces is currently being studied.1,8 While a single application of SDF appears insufficient for sustained effects, annual and semi-annual re-applications have been shown to be highly successful.1 Furthermore, SDF application is cost effective; one 8mL bottle of Advantage Arrest™, costing approximately $129, is sufficient to treat 1,600 carious lesions. The widespread use of SDF is limited by the fact that it stains the carious lesion black, and sometimes causes a temporary metallic taste.1,2,7-12,15-17 Acceptability of the black staining has been studied in two recent studies.2,18 Chu et al. demonstrated that parents of Chinese preschool children expressed no significant changes in their satisfaction with their child’s appearance following treatment with SDF.2 In an initial report of parental response to a scenario of a large cavity on their child’s baby molar, parents’ decisions regarding SDF treatment were influenced by their child’s behavior and gender, the location of the tooth to be treated, and the use of local anesthesia.18 SDF treatment can be a promising strategy to manage dental caries in young children and those who have special needs.2 Geriatric patients with high anxiety or special needs and other patient populations could also benefit significantly from its application.4,19-22
The incidence of oral disease is disproportionately greater for lower-income and rural populations, racial and ethnic minorities, medically compromised or disabled populations and young children.23 In California, the licensure category of registered dental hygienists in alternative practice (RDHAPs) was created to help care for the substantial percentage of the population lacking access to dental care.23,24 RDHAPs receive specialized training and a specific license to treat patients with limited access by delivering dental hygiene care in the residences of patients that are homebound, at schools, residential facilities, community institutions, and other dental health professional shortage areas.22 RDHAPs are most likely to use SDF as they are authorized to provide preventive oral health services without direct supervision in these community-based settings.23,25
Although the clinical efficacy of SDF has been extensively studied,17 SDF is relatively new to the field of dentistry in the U.S. Consequently, the level of knowledge possessed by RDHAPs in California regarding SDF treatments is not known. The purpose of this study was to assess the perceptions of RDHAPs regarding the use of SDF to treat dental caries.
Methods and Materials
This cross-sectional study was approved by the Institutional Review Board of the University of California, San Francisco (UCSF). The target population consisted of dental hygienists licensed as RDHAPs in the state of California. RDHAP email addresses were acquired from various Internet sources, i.e., publicly available lists available from the Dental Hygiene Committee of California (DHCC), California Dental Hygienists’ Association (CDHA), and LinkedIn. All RDHAPs with known email addresses were included in the invitation to participate in the electronic survey.
A 16-item survey instrument was created to assess the perceptions of RDHAPs regarding treatment of caries with SDF. To assess the respondent’s familiarity with SDF, 8 response options were offered ranging from “never heard of product” to “use product frequently.” A brief description of SDF’s characteristics followed this item, for the benefit of respondents not familiar with SDF: SDF is an inexpensive, non-invasive clear antimicrobial varnish that can be applied with a micro-brush; SDF contains a fluoride concentration of 5%, which is twice the amount of fluoride present in 5% sodium fluoride varnish (2.26%); and the area treated with SDF hardens and turns black. The 12 subsequent questions, regarding the respondents’ perceptions, used the 5-point Likert scale, ranging from strongly agree to strongly disagree. The survey was created and distributed using Qualtrics™ (Provo, UT), a survey research program.
The survey was pre-tested on a convenience sample consisting of 8 dental hygienists in the Master of Science in Dental Hygiene program at UCSF, 2 dentists currently studying SDF at UCSF, and 2 practicing RDHAPs, in order to assess survey acceptability and feasibility. Survey modifications were made based on feedback.
A request to participate in the survey was distributed electronically to the respondents describing the purpose of the study, in addition to providing instructions for giving informed consent and a link to the survey instrument. Accessing the survey indicated the participant’s consent. Follow-up email messages were sent to non-respondents at 3, 6 and 8 weeks following the initial distribution to encourage participation.
Qualtrics™ tabulated the responses and calculated the response frequency for each survey item. Cross tabulation analysis determined the significant relationships between respondents’ employment/practice settings and their responses regarding perceptions of SDF, as well as between respondents’ responses regarding their perceptions.
Results
Respondents’ demographic information and level of familiarity with SDF
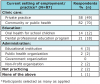
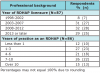
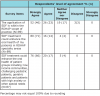
Of the 222 potential respondents, 103 completed the online survey (n=103), resulting in a response rate of 46%. One hundred and nineteen respondents stated that they worked in private practice and/or a community or public health clinical care setting (Table I). Ninety-two percent of the respondents had received their RDHAP licensure between 2003 and 2013 “or later.” The time frames that the RDHAPs received their licenses were similarly distributed over the ranges of years that were delineated in the survey, 2003-2007 (31%), 2008-2012 (32%), and 2013 “or later” (29%), as shown in Table II. Fifty-four percent of the respondents were unfamiliar with SDF as a caries therapeutic agent, with 32% reporting that they had never heard of SDF and 22% stating that they were not sure what the SDF product was used for (Table III).
Respondents’ perceptions regarding SDF as a caries therapeutic agent
Seventy-eight percent of the respondents agreed that the application of SDF was within the RDHAP scope of practice (Table IV). Respondents’ agreement that the use of SDF was within the RDHAP scope of practice was statistically related to their type of employment/practice setting (p<0.01). Almost all respondents agreed that SDF treatment could enhance the oral health of patients in RDHAP specialty areas and patient groups in low-income communities, challenging pediatric patients, geriatric patients, and those with high anxiety or other special needs.
The majority of respondents agreed that many patients or their parents would be interested in SDF for the reasons expressed in the survey displayed in Table V. Ninety-one percent of the respondents agreed with the statement, “Patients (or the parents of patients) would be interested in SDF because it does not require the use of local anesthesia.” A small number of respondents disagreed with statements describing the advantages of SDF. Fifty-six percent of the respondents agreed that many patients or their parents would not accept treatment of dental caries with SDF due to the permanent black staining of the carious lesion. This perception was significantly related (p=0.03) to their employment/practice settings (Table V).
Overall, 88% of respondents perceived that the advantages of SDF outweighed the disadvantages for the patients that they were accustomed to treating in their RDHAP practice settings. The statistical relationship of this statement to other responses is summarized in Table VI. Most respondents agreed that they “would like to use SDF to arrest active carious lesions” in their patients (91%) and that they “want to offer the option of SDF so that [their] patients receive the best dental care” (93%).
Discussion
This study assessed the perceptions of RDHAPs regarding the use of SDF to treat dental caries. Treating carious lesions with SDF is especially useful in situations where dental resources are limited and treatment can be carried out by dental auxiliaries,26 situations in which RDHAPs typically practice. The majority of respondents agreed that the application of SDF to treat dental caries is within the RDHAP’s scope of practice. These respondents are in agreement with the California law allowing RDHAPs to apply topical therapeutic agents for the control of dental caries without direct supervision.25,27 The phrase “without direct supervision” allows for RDHAPS to practice in specified settings, including the residences of the homebound, nursing homes, hospitals, residential care facilities, dental health professional shortage areas, and other public health settings.23,25
Most of the respondents who agreed that “the application of SDF is within the RDHAP scope of practice” also reported that they were currently practicing in community or public health settings. These respondents most likely viewed their scope of practice in terms of the activities and needs required by the patients in the settings in which they practice. Practicing in community/public health settings may have provided these respondents experiences that enhanced their comfort working in an environment with limited resources and supervision while serving patients with extensive dental needs. Because the RDHAP may be the only oral health care provider these patients see,23,26 the RDHAP may be more accustomed to the greater demands and expectations of extended dental services.
Approximately one quarter of the respondents did not believe that the application of SDF to treat dental caries was within the RDHAP scope of practice. These respondents may have disagreed based on the survey’s use of the phrase “to treat dental caries.” They may have viewed the treatment of dental caries as the sole responsibility of the designated supervising dentist. Also, many dental hygienists, including RDHAPs, may see their role as preventive rather than treatment-based. In addition, the description of SDF’s application technique, “can be applied with a micro-brush,” may have required additional clarification, for example, that the excavation of soft dentin is not needed because SDF will react with the tooth surface and create a layer of silver protein that resists bacterial acids and promotes the formation of hydroxyapatite and fluorapatite.15,17 Some respondents raised concerns about the legal ambiguity regarding the use of SDF “off-label” to treat dental caries. They may not have been aware that off-label use of approved pharmaceuticals is common, and these drugs frequently have medical evidence supporting their “off label” use.28 As a Class II medical device, regulatory controls are required to provide assurance of the device’s safety and effectiveness.28 Similar to SDF, sodium fluoride varnish has been cleared by the FDA for treatment of dentinal hypersensitivity,29 although it is widely used to prevent dental caries.16 Since the time this survey was conducted in 2015, SDF has been granted the designation of Breakthrough Therapy as a treatment for arresting dental caries in children and adults by the FDA.6
The majority of respondents agreed that patients or their parents would be interested in SDF for a number of reasons. First, it is an alternative to removing tooth structure by drilling to place restorative material. Avoiding dental procedures involving use of a drill could substantially alleviate the angst associated with a dental visit for many patients. Secondly, SDF is applied like a varnish on top of the carious lesion; thus, it does not require the use of local anesthesia. Fear and stress frequently prevent people from visiting the dentist and are attributed to a variety of factors, including the sound of the dentist’s drill and the thought of the needle to administer local anesthesia.30,31 The greatest percentage of respondents strongly agreed that fear of the injection for local anesthesia is a major contributor to dental anxiety. Furthermore, the application procedure of SDF, like that of other topical agents and varnishes, considerably reduces the amount of time required for a dental visit to treat caries.19,20 Lastly, the potential cost of a dental visit can create a barrier for the patient to avoid dental appointments and treatment31; however, in contrast, SDF is very cost effective. Currently sold for approximately $129.00 per bottle (8mL), one drop of SDF (25μL) is sufficient to treat five teeth.1 Therefore SDF may be a viable option for patients faced with the problem of limited financial resources.10,21
Over half of the respondents agreed that many patients would not accept the treatment of dental caries with SDF due to the permanent black staining of the carious lesion. This may be an assumption by respondents who feel that patients are biased by the media marketing the importance of esthetic appearance. However, based on the studies of Chu, et al. and Tesoriero, et al., this may not be true, especially in all cultures. In Chu’s study parents of Chinese preschool children expressed no change in satisfaction with their children’s teeth and appearance following SDF treatment.2 While these results from a Chinese culture may not be directly related to Western norms, Tesoriero’s study was conducted in New York, where most of the parents were comfortable with SDF treatment on a posterior tooth but not on an anterior tooth.18
The greatest number of “disagree” responses to the statement “Many patients (or parents of patients) would not accept treatment of dental caries with SDF due to the permanent black staining of the carious lesion” were from respondents who were currently practicing in community or public health settings. This may be because the RDHAPs working in these settings may be regularly treating patients whose primary concern is having teeth free of painful carious lesions. Teeth with black stains due to SDF may not be a contraindication for them.
The majority of respondents agreed that the advantages of SDF, including its low cost, efficiency of treatment, and the fact that it does not require the use of local anesthesia, outweighed the disadvantage of the black staining for their patient populations. Moreover, the nature of the application procedure facilitates its use by dental auxiliaries, such as RDHAPs.26 Consequently, the respondents in this study would like to use SDF to arrest active carious lesions in their patients and to offer the option of SDF so that their patients can receive optimal dental care.
The finding that approximately half of the respondents were unfamiliar with SDF as a caries therapeutic agent was not surprising since SDF was not available in the United States until 2015.1 However, due to SDF’s substantial benefits, the issue of lack of knowledge should be addressed. Opportunities need to be promoted to educate all oral health care providers of the advantages/disadvantages of the application of this medicament. It is recommended that dental hygiene educational programs at all levels—entry-level to advanced degree--provide both didactic information and clinical experiences. More continuing education programs with similar didactic and clinical components are also recommended. Education should not be limited to oral health care providers, but include other health care providers, especially pediatricians and nurses.
One limitation in generalizing these results to a broader population is that the subjects of this study were RDHAPs. This category of dental hygienist is somewhat unique to California, although many other states allow dental hygienists to practice in specific settings with less supervision.32 Furthermore the 46% response rate may suggest a response bias. RDHAPs who were not familiar with SDF may not have been interested in completing the survey. Ten of the 11 respondents who did not continue the survey after the item probing familiarity indicated that they were not familiar with SDF. Another limitation may be the use of the term “private practice,” which may have been ambiguous in terms of their current setting of employment/practice. Respondents owning RDHAP practices may consider “RDHAP private practice” as referring to something other than what is commonly known as a “private practice” in the field of dentistry. It might have been prudent to define private practice as being associated with a supervising dentist, a requirement for RDHAPs in California. The option to type in an answer allowed for clarification of respondents’ interpretations.
Conclusion
The clinical application of SDF has been shown to be effective in arresting carious lesions; however, its use depends upon the oral health care providers’ familiarity with the product and their perceptions of its benefits to their patient population. This study surveyed RDHAPs, dental hygienists who are licensed to treat underserved patients in a variety of settings in California. Approximately half of the respondents were unfamiliar with SDF, which emphasizes the need for the properties of SDF to be addressed in dental hygiene educational programs and continuing education courses. After being informed of the application process and SDF’s clinical efficacy, most respondents agreed that the use of SDF was within their scope of practice. These respondents felt that their patients or the parents of their patients would be interested in this treatment due to its advantages, including not requiring local anesthesia and the removal of tooth structure, its low cost and reduced treatment time. According to the respondents, these advantages outweighed the disadvantage of permanent black staining of the carious lesion, and they were interested in offering the option of SDF as a means of delivering optimal dental care.
Acknowledgment
The authors are grateful to Jeremy A. Horst, DDS, PhD, and Hellene Ellenikiotis, DDS, for their stimulating conversations regarding SDF and their contributions to the development of the survey.
Salina Chhokar, RDH, MS is a graduate of the Master of Science program in dental hygiene; Lory Laughter, RDH, MS is formerly an assistant clinical professor; Dorothy J. Rowe, RDH, PhD is an associate professor emeritus; all in the Department of Preventive and Restorative Dental Sciences, University of California, San Francisco, CA.
Corresponding author: Dorothy Rowe, RDH, PhD; Dorothy.rowe@ucsf.edu
References
1. Horst JA, Ellenikiotis H, Milgrom PM, UCSF Silver Caries Arrest Committee. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications and consent. J Calif Dent Assoc. 2016 Jan;44 (1):17-28.
2. Chu CH, Lo ECM, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 2002 Nov;81(11):767-770.
3. Sharma G, Puranik MP, Sowmya KR. Approaches to arresting dental caries: An update. J Clin Diagn Res. 2015 May;9(5):8-11.
4. Alcorn M, Johnson T. New addition to the caries armamentarium. Dimensions Dent Hyg. 2015 Jul;13(7):24-27.
5. U.S. Food and Drug Administration. Diamine Silver Fluoride Dental [Internet]. Silver Spring(MD): U.S. Food and Drug Administration; 2017[cited 2017 Jan 16] Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPCD/classification.cfm?ID=1332
6. Wilson TG. Silver diamine fluoride receives new FDA designation. Decisions in Dentistry. 2016 Nov;2(12):10.
7. Yee R, Holmgren C, Mulder J, et al. Efficacy of silver diamine fluoride for arresting caries treatment. J Dent Res. 2009 Jul;88(7):644-7.
8. Mattos-Silveira J, Floriano I, Ferreira F, et al. Children’s discomfort may vary among different treatments for initial approximal caries lesions: preliminary randomized controlled clinical trial. Int J Clin Pediatr Dent. 2015 Jul;(25):300-4.
9. Zhi QH, Lo ECM, Lin HC. Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in preschool children. J Dent. 2012 Nov;40(11):962-7.
10. Tan HP, Lo ECM, Dyson JE, et al. A randomized trial on root caries prevention in elders. J Dent Res. 2010;89(10):1086-1090.
11. Dos Santos VE Jr, de Vasconcelos FM, Ribeiro AG, et al. Paradigm shift in the effective treatment of caries in schoolchildren at risk. Int J Dent. 2012 Feb;62(1): 47-51.
12. Targino AG, Flores MA, dos Santos VE Jr, et al. An innovative approach to treating dental decay in children. A new anti-caries agent. J Mater Sci Mater Med. 2014 Aug;25(8):2041-7.
13. Mei ML, Li QL, Chu CH, et al. The inhibitory effects of silver diamine fluoride at different concentrations on matrix metalloproteinases. Dent Mater. 2012 Aug;28(8):903-8.
14. Featherstone JD. The continuum of dental caries – evidence for a dynamic disease process. J Dent Res. 2004;83 Spec Iss C:C39-42.
15. Yamaga R, Nishino M, Yoshida S, et al. Diamine silver fluoride and its clinical application. J Osaka Univ Dent Sch. 1972 Sep;12:1-20.
16. Newburn E. Topical fluorides in caries prevention management: A North American perspective. J Dent Educ. 2001Oct; 65(10):1078-83.
17. Gao SS, Zhao IS, Duangthip D, et al. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clin Trans Res. 2016 May;1(3):1-10.
18. Tesoriero J, Lee A. Parental acceptance of silver diamine fluoride. Paper presented at: American Academy of Pediatric Dentistry Annual Session; 2016 May 26-29; San Antonio, TX.
19. Quock RL, Patel SA, Falcao FA, et al. Is a drill-less dental filling possible? Med Hypotheses. 2011Sep;77(3):315-17.
20. Clarkson BH, Exterkate RA. Non-invasive dentistry: A dream or reality? Caries Res. 2015; Suppl 1:11-17.
21. Zhang W, McGrath C, Lo EC, et al. Silver diamine fluoride and education to prevent and arrest root caries among community-dwelling elders. Caries Res. 2013;47(4):284-90.
22. Monse B, Heinrich-Weltzien R, Mulder J, et al. Caries preventive efficacy of silver diamine fluoride (SDF) and ART sealants in a school-based daily fluoride toothbrushing program in the Philippines. BMC Oral Health. 2012; Nov 21;12:52.
23. Mertz E, Glassman P. Alternative practice dental hygiene in California: past, present, and future. J Calif Dent Assoc. 2011 Jan;39(1):37-46.
24. Dyer TA, Robinson PG. The acceptability of care provided by dental auxiliaries; A systematic review. J Am Dent Assoc. 2016 Apr;147(4):244-54.
25. California Dental Hygienists’ Association. RDHAP [Internet]. Sacramento (CA): California Dental Hygienists’ Association; 2015 [cited 2015 Dec 6] Available from: from http://cdha.org/rdhap
26. Craig GG, Powel KR, Price CA. Clinical evaluation of a modified silver fluoride application technique designed to facilitate lesion assessment in outreach programs. BMC Oral Health. 2013 Dec 28;13:73.
27. Dental Hygiene Committee California. Licenses, laws and regulations [Internet]. Sacramento (CA): California Department of Consumer Affairs; 2016 [Cited 2016 April 24] Available from: http://leginfo.legislature.ca.gov/faces/codes_displayText.xhtml?lawCode=BPC&division=2.&title=&part=&chapter=4.&article=9
28. U.S. Food and Drug Administration. Understanding investigational drugs and off label use of approved drugs [Internet]. Silver Spring (MD): U.S. Food and Drug Administration; 2016 [cited 2016 Apr 28] Available from: http://www.fda.gov/ForPatients/Other/OffLabel/default.htm
29. U.S. Food and Drug Administration. Fluoride Varnish [Internet]. Silver Spring (MD): U.S. Food and Drug Administration; 2017 [cited 2017 Jan 3] Available from: http://www.accessdata.fda.gov/cdrh_docs/pdf3/k031932.pdf
30. Yamada T, Ebisu S, Kuwano S. A questionnaire survey on the effect of the sound of dental drills on the feeling of patients in dental clinics. Acoust Sci Tech. 2006;27(5):305-8.
31. Armfield JM, Ketting M. Predictors of dental avoidance among Australian adults with different levels of dental anxiety. Health Psychol. 2015 Sep;34(9):929-40.
32. American Dental Hygienists Association. Direct Access States [Internet]. Chicago(IL): American Dental Hygienists’ Association; 2016 [cited 2017 Jan13] Available from: https://www.adha.org/resources-docs/7513_Direct_Access_to_Care_from_DH.pdf