You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
In 2015, dentistry topped Business Insider’s list of “The 27 jobs that are the most damaging to your health.”1 At No. 1, dentists’ jobs were ranked more harmful than those of continuous mining-machine operators and nuclear equipment operation technicians. One of the most significant factors in dentistry’s rise to the top was the prevalence of musculoskeletal disorders reported by dental professionals. Research indicates that up to 76% of practicing dentists report symptoms related to musculoskeletal disorders.2 This statistic has not changed much over the last 7 decades. Despite substantial innovations in practice strategies and ergonomic equipment design, dental professionals continue to develop musculoskeletal disorders and practice in pain.
The Centers for Disease Control and Prevention’s definition of musculoskeletal disorders is “injuries or disorders of the muscles, nerves, tendons, joints, cartilage, and spinal discs.”3 By this definition, an offense to any component of either the muscular or skeletal system could be diagnosed as a musculoskeletal disorder; the definition is too broad for dentists trying to understand the effects of dental practice on their pain. A more accurate description of musculoskeletal disorders relating to dentists can be narrowed down to “work-related” musculoskeletal disorders (WMSDs). With WMSDs, the work environment and the performance of the work contribute to the development of the musculoskeletal disorder, not just general circumstances that may result in injuries.4 WMSDs in dentistry have been thoroughly investigated and shown to have profound influence on thesymptoms experienced by dental professionals.5 Recognizing that musculoskeletal disorders are triggered specifically by work environments and performance provides more insight into the source of pain in dentistry.
WMSDs can be prevented by understanding risks, appreciating the role of pain, and applying basic physical and ergonomic principles to everyday work tasks. For dentists who have already developed WMSDs and passed the prevention stage, similar strategies as those used for prevention can help resolve many of the impairments associated with WMSDs.
PREVALENCE OF WMSDS IN DENTISTRY
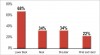
Dentistry has a long history of WMSDs. Biller was the first to link dentistry to WMSDs in 1949, when he reported that 65% of dentists had back pain.6 Nearly 70 years later, the statistics are unfortunately similar. Al-Shehri et al, in a recent study of 515 dental students and dentists, discovered that 64% reported lower back pain.7 Many researchers have expanded on Biller’s initialwork. Studies have confirmed that low back pain is only one of many pain-related complaints of dentists. Although exact numbers vary, clear patterns of musculoskeletal dysfunction have emerged. Figure 1 shows the most common areas of pain reported in dentists, as measured in a recent study by Al-Mohrej et al.8
When specific attributes are considered, distinctive patterns are evident. Age and gender are predictive of pain experienced by dentists. Older dentists report increased incidents of back and neck pain, while younger dentists report pain in other areas, including shoulders, knees, feet, and hands.9 The pain experience itself differs for male and female dentists. These differences include intensity of pain, frequency of symptoms, and anatomical regions. Some studies have shown that female dental professionals report more severe and frequent symptoms than their male counterparts.10,11 Male dental professionals have the most pain complaints in the lower back, neck, and shoulder regions, while female dental professionals report pain in those regions in addition to hands and knees.12
Dentists have a very high likelihood of experiencing pain, a prominent symptom in the development of WMSDs. Research from across the world indicates the phenomenon is global and can significantly impact a dentist’s quality of life and career.
IMPACT OF WMSDS
The most immediately noticeable consequence of WMSDs is the physical limitations dentists experience. The body protects itself from pain by reducing the range of motion of joints and strength of muscular contractions and by modifying synergistic movements. These changes in the musculoskeletal system restrict the ability of the dentist to perform work tasks in a normal fashion. Activities such as accessing the oral cavity correctly, maintaining a good visual field, and using equipment and instruments may become arduous. By attempting to protect against injury and reduce pain, the body requires the dentist to adjust his/her practice to accommodate.13 Muscle imbalances may develop secondary to the initiation of the protection mechanism.These imbalances alter the biomechanics of joint motion, contractility of muscles, and positioning of tendons.14,15 Alterations in movement patterns of any joint can lead to increased risk of dysfunction and injury.16,17
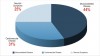
Impairments involving the musculoskeletal system affect other systems of the body, including the cardiovascular and psychological systems.18,19 Each of these systems plays an important role in overall health. In a study of premature retirement of dentists, Burke et al found patterns of illness that precipitated retirement. Detailed in Figure 2, the illnesses most often cited for early exit from dentistry were found to be musculoskeletal disorders, cardiac disorders, and neurotic symptoms.20 These categories are not discrete; they are interrelated. Research has shown an intricate relationship between dysfunctional musculoskeletal systems, cardiac disease, and mental health. One such study found a strong association between cardiovascular disease and rotator cuff tendinopathy.21 The association is likely the result of reduced physical activity because ofpain. Reduced physical activity, a common result of WMSDs, increases the risk of cardiovascular disease. Other studies have highlighted the link between mental and physical health. Depression and severe pain are commonly associated.22 Chronic pain sufferers experience depression at twice the rate of others.23 The American Psychological Association has detailed the relationship between stress and other health areas, including neurotic symptoms as well as the cardiac, respiratory, musculoskeletal, nervous, and reproductive systems.24 Consequently, it is practically impossible to isolate the effects of musculoskeletal dysfunction from the rest of the body. The physical impact of WMSDs is extensive. Pain in the musculoskeletal system is indicative of a person’s overall health and should be treated accordingly. If left untreated, WMSDs can become life-threatening.
WMSDs have far-reaching effects not only on overall health, but on personal lifestyles. Pain developed while practicing dentistry can significantly influence activity outside of work. Almost one-third of dentists attribute reduction in normal activities to neck and upper back pain from practicing dentistry.25 The occurrence of lifestyle changes because of chronic pain is well-documented.26,27 The most common lifestyle change is reduced physical activity. This change alone is a significant contributing factor to increased risk of developing cardiovascular diseases.28 Other modifications to lifestyle include sleep disturbances, reduced social activity, and increased anxiety.28,29
Lifestyle choices and limitations resulting from WMSDs amplify the physical impairments, but their impact does not end there. The financial health of dentists and their practices can be affected by WMSDs. Sick leave, absenteeism, reduced hours, and even early retirement may considerably diminish the income potential of a dentist with a WMSD. Dentists owning private practices often fear the loss of personalincome as well as the appearance of stability of their practice if they are unable to work,30 yet research indicates up to 39% of dentists will miss work secondary to musculoskeletal pain.9,31 The reasons most frequently cited for absenteeism by dentists are pain in the neck, shoulders, and lower back.32,33 Absenteeism may result in short-term financial losses, but early retirement has been estimated to reduce the lifetime revenue of an individual dentist between $1 million and $3 million.34
WMSDs have the potential to devastate the lives of dentists if left untreated. Physical health, lifestyle changes, and financial status may all be compromised. To avoid WMSDs in their practices, dentists should become aware of the consequences, beginning with recognizing pain as the earliest indicator of a WMSD.
UNDERSTANDING PAIN IN DENTAL PRACTICE
The recent rise of pain science has yielded a body of knowledge for recognizing and treating pain. Pain is essential to living a healthy life because it prevents and protects against possible assaults on the body. The pain mechanism is designed as a complicated and responsive warning system; it is vulnerable to physiologic changes and malfunction. Resolving pain in its earliest stages allows the pain mechanism to remain in a healthy state. It is important to understand how the pain mechanism is activated, as well as how it can malfunction and be remediated. Whether the feeling of pain is a consequence of a dentistry practice, an old sports injury, traumatic accident, or anatomical abnormality, tissue damage and nervous system dysfunction are the two distinct and overlapping factors that are responsible for all pain.
Tissue Damage
Most tissue damage occurs in dentists because of repeated or prolonged contractions by underperforming muscles to maintain static positioning. Repetitive actions, awkward positioning, and excessive force are three of the main risk factorsinvolved in creating tissue damage.35 Modification of any of these elements may significantly reduce the risk for acquiring microtrauma and decrease the risk of developing WMSDs.
Repeated contractions are performed when using the same muscle group to perform the same or similar activities over and over. Repeated forceful contractions with minimal rest time strain and wear the muscle and tendon tissues, resulting in microtrauma and inflammation.36 Accumulation of microtrauma over time eventually leads to injury. This phenomenon has many names, including cumulative trauma disorder and repetitive stress injury. As dentists continually adopt the same postures throughout the day, the musculature does not have ample recovery time for repair of sustained microtrauma.
Poor muscle performance is another factor in tissue damage. When muscles are not operatingat their optimal capacity, they may become weak, uncoordinated, and inflexible. Muscle imbalances may develop that will alter the synergy of muscle groups.13 A rounded shoulder position caused by poor posture (Figure 3 and Figure 4) over time can result in imbalances in the shoulder muscles. This common position found in dentistry shortens and restricts the ability of the pectoral muscles to lengthen to full capacity. The change in the length of the pectoral group effectively changes the position of the humerus and scapula; the humerus will become slightly internally rotated, with a forward bias of the scapula. The opposite effect may be experienced by the rhomboid muscles of the upper thoracic, charged with accurately positioning the scapula: the rhomboid group may be lengthened and unable to contract to oppose the pectoral group (Figure 4). This particular muscle imbalance has been shown to influence joint mechanics and contribute to shoulder dysfunction.37,38 Asnoted previously, shoulder pain is one of the top complaints of dentists. It is a result of poor posture.39,40 Ensuring optimal skeletal alignment is crucial for improving muscle balance and performance, thus reducing risk of tissue damage.
The final contributor to tissue damage in dentistry is perhaps the most infamous. Prolonged static contractions have been cast as the villain of dentistry for decades. A static contraction occurs when a muscle group is required to contract in the same capacity, typically as a stabilizing strategy. Often the contractions are maintained at a sub-maximum level for lengthy periods of time. These lengthy contractions compromise the normal metabolic activity and lead to muscle fatigue. When fatigued, muscles can no longer maintain the sub-maximal contractions and are at severe risk for injury. To protect the muscle tissue, signals indicating muscle failure are relayed to sensory nerves that initiate the pain cycle (Figure 5).
Dentistry is the confluence of three major risk factors for tissue damage: (1) the practitioner is required to perform repeated contractions that may cause microtrauma; (2) awkward posture not suitable for proper skeletal alignment encourages muscle imbalances; and (3) the prolonged contractions necessary to stabilize the body’s position can lead to fatigue. Tissue damage can be repaired with noninvasive or more aggressive interventions. However, there are instances where tissue damage is not the reason dentists experience pain.
Dysfunctional Neurologic System
The nervous system has specialized pathways for which to gather information to assess the statusof the body. The descending facilitation pathway is responsible for not only gathering information, but also generating the sensation of pain to encourage conscious attention.41 In a healthy system, the signals released by damaged tissues warn the sensory nervous system that something is amiss. The brain uses that information to activate the pain pathway to gather information and to remove the tissue from harm, if possible. An example is when a dentist begins to feel the first twinges of pain or discomfort. If the dentist moves out of the offending position, the immediate threat of tissue damage is removed and the pain signals will eventually cease because the central nervous system received a signal from the damaged tissue, made a decision, relayed information to remediate the harmful situation, did not receive any more indicators of damage, and therefore stopped sending pain signals.
Chronic pain changes this dynamic. The nervous system can become more than a relay system for injury and pain: it can become the actual source. Peripheral sensory nerves, the nerves responsible for receiving signals, can send faulty information to the brain, signaling tissue damage when no damage is occurring. When the brain receives these signals, it activates the descending facilitation pathway to gain more details to make an informed decision for remediation.41 Because there is no information to be gained, pain signals are sent as a precautionary measure. Unfortunately, the nervous system does not recognize that there is no signal indicating damage. It remains activated despite the absence of the activation signals, leading to a vicious cycle of chronic pain that is exacerbated with even the slightest change.42
Pain is experienced entirely in the brain. If there is a disruption of the nerve signal from an injured body part to the brain, there will be absolutely no pain, even if the injury is very severe. The reverse is also true. If the brain expects to experience pain, even when there is no physical harm, pain will be felt. Several remarkable studies have shown how the brain interprets pain with and without physical harm. Geuter and Büchel found that the anticipation of pain was enough to activate the descending facilitation pathway and invoke the pain experience even before a placebo agent was applied to the skin.43
Generation of the pain cycle through a dysfunctional nervous system is the bane of pain science. Oversensitive and excessively excitable sensory nerves are not as easily treated as tissue damage; even after tissue has recovered, the sensory nerves may not return to normal functioning.42 Chronic low back pain is a good example of this phenomenon. Despite surgical interventions to restore tissues to normal or reduce offending causes, pain may persist. Failure to reduce pain by surgical interventions can leave dentists feeling hopeless.44-46 Dentists are no less susceptible to a dysfunctional nervous system than anyone else. Knowing that the nervous system may be responsible for pain allows dentists to consider noninvasive pain management techniques. Lack of pain management can result in further tissue damage or exaggeration of the nervous system’s response.
TREATING WMSDS IN DENTISTRY WITH A MULTIFACTORIAL APPROACH
Pain in dentistry is complex; eliminating it from daily practice and life is not easy. To address the factors that can lead to painful practice, a multifactorial approach is recommended. The evidence-based strategies below have been provided as a sample of the breadth of treatment options for dentists.
General Exercise Programs
General exercise is widely understood to facilitate good health. Aerobic exercise programsimprove coordination, strength, and endurance—all of which may be affected while practicing dentistry.
Specific Exercise Programs
For dentists hoping to prevent specific impairments related to WMSDs, a specific exercise program may be indicated. Specific programs designed and prescribed by licensed professionals such as physical and occupational therapists can anticipate likely muscle imbalances and joint dysfunctions that result in pain. Programs frequently prescribed by these professionals include postural training, strengthening, coordination, and flexibility exercises. The following is a series of common exercises prescribed for dental professionals for prevention or relief of WMSDs. Not all exercises are appropriate for individual cases. If pain is experienced or exacerbated, exercise should be terminated immediately and a physical or occupational therapist should be enlisted to ensure appropriateness and proper performance of exercise.
Abdominal activation. The fundamental exercise that is critical to a successful posture in dentists, whether sitting or standing, is the activation of the rectus abdominis, or the six-pack muscle, along with the abdominal obliques. The rectus abdominis originates at the bottom of the rib cage and inserts into the anterior pubic bone. It is one of the primary stabilizers of the trunk and is responsible for upright posture. Without proper activation of the rectus abdominis, support for the vertebral column falls to the small muscle groups surrounding the spine. These muscles were designed to exert fine control, not provide gross movements as with the larger muscle groups.47 Often, dentists try to correct posture by retracting their shoulders and arching the back. The muscles used for those movements are only accessory postural muscles and will fatigue, quickly leaving the dentist once again in a compromised posture. The stabilizing muscles were designed for endurance; once trained properly,they do not fatigue quickly. To strengthen this group of muscles and create a healthy posture, the abdominis rectus should be activated often and the contracted position should be maintained for as long as possible. The abdominal obliques will co-activate automatically to create a stable trunk. Eccentric activation of the rectus abdominis can be performed sitting, standing, or lying down. When activated while bending forward during practice, a key element is to protect the lumbar spine. To activate the rectus abdominis, simply draw in the abdomen as though trying to join the navel with the spine. Figure 6 shows the position before activation, and Figure 7 after activation. Respiration or talking should not be affected.
Hamstring stretch. The hamstring is a group of muscles located in the posterior thigh and is pivotal to treating low back pain. Although the individual muscles attach in various places, all attach to the posterior pelvis and can exert a downward rotational force when tight. This downward force can tilt the pelvis backwards while standing or sitting, which reduces the lumbar lordosis, or curvature, and changes the stress points in the vertebral column, ultimately leading to back pain.48 Most dentists continue to practice dentistry in a seated position. From being seated most of the day, the hamstring group has the potential to become shortened, thus exerting the downward rotational force on the pelvis. Stretching this muscle groupproperly and regularly can help prevent shortening and allow the pelvis to maintain optimal alignment. Figure 8 and Figure 9 illustrate the proper form for stretching the hamstrings. The knee is extended and supported by the floor while the back is straight. One should gently lean forward until a slight discomfort is felt, then stop. To thoroughly stretch the entire muscle, including the musculotendinous junction, a prolonged low-intensity stretch is much more effective than a short higher-intensity stretch.49 The ideal stretch should be slightly uncomfortable and maintained for 60 seconds. For best results, it is also recommended the stretch be performed 3 times at night.
Scapular retraction. Performing a scapular retraction exercise accomplishes two goals: first, it provides a passive stretch for the often-shortened pectoral muscles50; second, it helps reactivate the rhomboid muscle group along with other scapular stabilization muscles to improve strength and endurance. If performed frequently and correctly, the exercise helps restore the balance of the anterior/posterior shoulder muscles. There are a few important considerations before performing this exercise. These muscles are not postural muscles; they are not designed for maintaining an upright posture, although they may assist—they fatigue quickly. This exercise does not negate the abdominal activation exercise, but it should be used in conjunction with it to createa more ideal alignment. It is tempting to extend the shoulder by driving the elbows backwards, but unfortunately, if the elbows are used to extend the shoulders, the rhomboid muscles are not activated and therefore will not be strengthened. The last consideration is that this exercise is best performed either in front of a mirror or with someone watching from behind initially. It can be challenging to get the right “feel” at first; visual or verbal cues can help facilitate proper form. Figure 10 and Figure 11 illustrate the proper form. The position of the dentist’s elbows and the wrinkling of his shirt are both indications that he is performing the exercise correctly. This exercise should be performed with up to 15 repetitions and 5- to 10-second holds twice per day. The exercise can also be performed during short breaks to re-establish scapular positioning.51
Cervical retraction. Muscle imbalances are also commonly found in the cervical region. The typical imbalance found in the cervical region occurs because the dentist’s neck is flexed during most tasks, especially when not using proper-fitting loupes. The flexed position of the cervical spine encourages a weakness in the anterior muscles of the neck. The deep neck flexors can become weak because the more superficial neck flexors are doing most of the work.34 To strengthen the deep neck, good form is crucial.52 In Figure 12 and Figure 13, the direction of the movement can be seen. The chin maintains a neutral position, not tipping up or down, and is moved backwards. The head is sliding posteriorly while remaining parallel with the vertebrae. If done properly, a “double chin” is formed. The deep neck flexors are postural muscles, so endurance training is preferred to the strength training described above for the scapular retraction. The initial regimen is dependent on the severity of the weakness. If the deep neck flexors are very weak, simply attaining the correct position may be enough at first. However, holding the position for up to 60 seconds for 3 repetitions should be a goal. Strengthening the deep neck flexors improves proprioceptive awareness, which can eventually help correct many cervical positioning/posture deficits found with dentists.
Proprioceptive Awareness Activities
Proprioception is the reflexive ability of the body to know where it is in space and how to move within it. Specialized receptors are distributed in all the synovial joints of the body to provide information about the position of each one.53 Proprioceptive awareness as it pertains to dentistry is the ability of the dentist to know and understand the position of his or her body in space while performing work tasks. Generally, this awareness does not require a conscious effort; for dentists who are consistent withexercise routines, it is relatively automatic. The brain processes the position of each joint and is well acquainted with which muscle actions are required to maintain healthy positioning.
However, for dentists who do not consistently exercise, learning how to position the body properly may take considerable effort in the beginning. Without outside assistance, it is difficult to assess whether proper alignment is attained or maintained. Asking assistants to provide reminders whenever an improper posture is assumed is a good place to start. Using visual aids such as video or photographs can provide additional feedback on positioning. Technology can assist as well. Sensors can be worn on the body that provide immediate feedback when posture is less than ideal, and software programs can help guide awareness. Yoga can be an excellent activity to improve proprioceptive awareness. The deliberate attention to the positioning of the body achieved through yoga can significantly improve the spatial cognition in the brain as well as increase strength and flexibility.54 With proprioceptive training, posture and ergonomic interventions may be more effective because the body is able to make minor corrections in positioning and muscle activation.
Environment
The environment in the dental office is one of themost important extrinsic elements that can determine the health of a dentist. The office design and equipment selected can either aid in supporting the dentist’s health or become a detriment to it. Ergonomic considerations go beyond the selection of chairs and loupes. Lighting, operating positions, and patient positioning should be considered when assessing health risks.
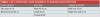
Chair. Regardless of what type of chair is selected, objective parameters should be obtained to achieve and maintain healthy operator posture during tasks. Most chairs today are more than adequate to provide proper support. Proper chair selection and adjustment should be based on the body position of the operator. Compare the posture of the dentist in Figure 14 and Figure 15. The chair that is adjusted properly allows a natural lumbar lordosis (or curve) to exist (Figure 14). The poorly adjusted chair in Figure 15 forces a posterior pelvic rotation and flattens out the back because it is too low for the dentist, which will lead to muscle fatigue and pain. Figure 14 shows the correct positioning, with the hips slightly more elevated than the knees. Key elements of any operator chair that will ensure good posture are outlined in Table 1.55 An exception to the key elements listed is a saddle stool, regarding seat pan tilt. Saddle stools are designed in a way that any tilting adjustment will compromise theintegrity of the design and create more stress than relief. The other elements, height and lumbar support, remain the same.
Loupes. Properly measured and fitted loupes are the first line of defense against neck and shoulder pain. Without loupes, or with poor fitting ones, a neutral posture is impossible to achieve while performing dental tasks (Figure 16 and Figure 17). A vast selection of loupes is available for dentists. They vary by style, weight, magnification, and declination angles. Loupes can be paired with lighting attachments to improve field visualization even further. When selecting loupes, it is imperative that the working distance is measured correctly. This measurement can be problematic because dentists will often want to be measured with proper posture even if they have not taken the necessary steps to guarantee proper posture will be maintained for a lengthy period. Most of the time, it cannot, which renders the loupes measured while in correct posture useless. Before investing in a pair of loupes, consider the following:
Measure postural endurance. Record how long a correct posture can be maintained before muscle fatigue. Poor postural endurance is indicated when correct posture is unable to be maintained for 15 minutes without fatigue.56,57 Consider other interventions to improve postural endurance before investing in loupes.
Position of neck. The angle of neck flexion should be no greater than 20 degrees,34 which is difficult without loupes. When considering loupes, do not just consider the magnification and weight; have someone measure the angle of neck flexion, or take a photograph and measure it.
Varying positions. Dentists tend to perform work tasks while either sitting or standing. Variety in positions and postures improves general conditioning as well as muscle performance. There are six types of posture58:
• Lying down
• Sitting with forward lean
• Sitting in neutral position
• Reclined sitting
• Standing
• Walking
Obviously, practicing while lying down or walking is not optimal, but the other four positions should be considered.
Sitting with forward lean: This posture is most appropriate for delivering care. Ergonomic strategies to protect the body should be employed, including the chair and loupe guidelines discussed earlier.
Sitting in neutral position: Neutral position is appropriate for computer or office work requiring a seated position. In this posture:
• Elbows are flexed no more than 90 degrees.
• Hips, knees and ankles are all at 90-degree angles.
• Lumbar lordosis (curve) is present.
Different ergonomic considerations may apply to the neutral position. Lumbar supports, chair adjustments, armrests, and even small stools or blocks may be used to rest feet and to ensure proper angulation of legs.
Reclined sitting: Best used in resting situations, reclined sitting is important to vary the stressthrough the spinal column. If operator chairs have lumbar supports, dentists can lean back to rest during small breaks in procedures. Reclined sitting opens the hip angles and mobilizes the pelvis, allowing small movements of muscles that are often statically contracted. Reclined sitting at home or while driving is acceptable as well, but as with any other posture, prolonged reclined sitting can lead to tissue damage and pain. A good strategy to keep track of time spent in this position is to set a timer for 30 minutes; after the alarm sounds, change positions or take a short walk.
Standing: Seen as the alternative to sitting, there has been an industry movement for increased standing time during treatment. Historically, standing was the preferred method of delivering dental care until the 1960s. One reason sitting for treatment became popular was that it was thought it would reduce the load on the back and legs that was felt while standing; instead, it just moved it.59 Standing is best used for specific procedures that require a lot of leverage, such as tooth extractions. It can be used as an alternative to sitting at any time throughout the day to provide relief from sitting pressure.
Research has shown that no one posture position is the answer. When used correctly, working through each of the four positions throughout the day will create significant variation in movements, rest times, and stresses placed on the body, helping to prevent the development of WMSDs.60,61
Factors outside the office. Although practicing dentistry may be the primary source of developing WMSDs, activities outside the office also have an influence. Some high-risk activities include the following:
Cell phone/electronic use: The neck is typically flexed in a position similar to a poor workingposture.
Sitting in a recliner/driving: Although reclining may be comfortable for a short period, it also may mimic the unsafe rounded back posture commonly found in dentists, leading to further tissue damage.
Any activity requiring similar posture to what the body endures for long periods at work should be avoided, especially if it produces pain.
CONCLUSION
WMSDs in dentistry are a global problem. Although much is known about the impact of WMSDs on health, lifestyle, and financial status, little progress has been made to effectively reduce the prevalence. Research in pain science has begun to provide important information on why pain occurs even without tissue damage. Application of this information can greatly improve the likelihood that dentists can understand the source of their pain and select appropriate interventions for remediation. General and specific exercise programs can help prevent and protect dentists from the development of WMSDs. Striving for good general health and using specific exercises to strengthen, stretch, and coordinate muscles groups will greatly improve chances for practicing dentistry without pain. WMSDs are complex; no single intervention will fix everything. A multifactorial approach to WMSD prevention includes identification of sources of pain, exercise programs, proprioceptive awareness training, and ergonomic solutions. Pain in dentistry is not inevitable. Dentists have tools available for pain-free practice. Seeking treatment and advice from licensed professionals at the first signs of WMSDs and continuing to do so throughout the entirety of a dental practice will ensure a long and healthy career.
REFERENCES
1. Kiersz A. The 27 jobs that are the most damaging to your health. Business Insider. http://www.businessinsider.com/ the-most-unhealthy-jobs-in-america-2015-11/#9-stationary-engineers-and-boiler-operators-19. Published November 2, 2015. Accessed August 22, 2017.
2. Radanović B, Vučinić P, Janković T, et al. Musculoskeletal symptoms of the neck and shoulders among dental practitioners. J Back Musculoskelet Rehabil. 2017;30(4):675-679.
3. The National Institute for Occupational Safety and Health. Ergonomics and musculoskeletal disorders. Centers for Disease Control and Prevention. https://www.cdc.gov/ niosh/topics/ergonomics/default.html. Updated May 10, 2016. Accessed August 22, 2017.
4. Centers for Disease Control and Prevention. Work-related musculoskeletal disorders and ergonomics. https://www.cdc. gov/workplacehealthpromotion/health-strategies/musculoskeletal-disorders/. Updated March 1, 2016. Accessed August 22, 2017.
5. Mangharam J, McGlothan JD. Ergonomics and dentistry: a literature review. In: Murphy DC, ed. Ergonomics and the Dental Care Worker. Washington, DC: American Public Health Association; 1998:25-81.
6. Biller FE. The occupational hazards in dental practice. Oral Hyg. 1946;36:1194-1201.
7. Al-Shehri Z, Al Zoughool M. Prevalence and risk factors of musculoskeletal symptoms among dental students and dental practitioners in Riyadh City, Saudia Arabia. Arch Environ Occup Health. 2017;14:1-8.
8. Al-Mohrej OA, AlShaalan NS, Al-Bani WM, et al. Prevalence of musculoskeletal pain of the neck, upper extremities and lower back among dental practitioners working in Riyadh, Saudi Arabia: a cross-sectional study. BMJ Open. 2016;20(6):e011100. doi: 10.1136/ bmjopen-2016-011100.
9. Alghadir A, Zafar H, Iqbal ZA. Work-related musculoskeletal disorders among dental professionals in Saudi Arabia. J Phys Ther Sci. 2015;27(4):1107-1112.
10. Rundcrantz BL. Pain and discomfort in the musculoskeletal system among dentists. Swed Dent J Suppl. 1991;76:1-102.
11. Bozkurt S, Demirsoy N, Günendi Z. Risk factors associated with work-related musculoskeletal disorders in dentistry. Clin Invest Med. 2016;39(6):27527.
12. Tirgar A, Javanshir K, Talebian A, et al. Musculoskeletal disorders among a group of Iranian general practitioners. J Back Musculoskelet Rehabil. 2015;28(4):755-759.
13. Lund JP, Donga R, Widmer CG, Stohler CS. The pain-adaptation model: a discussion of the relationship betweenchronic musculoskeletal pain and motor activity. Can J Physiol Pharmacol. 1991;69(5):683-694.
14. Baratta R, Solomonow M, Zhou BH, et al. Muscular coactivation. The role of the antagonist musculature in maintaining knee stability. Am J Sports Med. 1988;16(2):113-122.
15. David G, Magarey ME, Jones MA, et al. EMG and strength correlates of selected shoulder muscles during rotations of the glenohumeral joint. Clin Biomechan. 2000;15(2):95-102.
16. Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39(2):90-104.
17. Delahunt E, Monaghan K, Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am J Sports Med. 2006;34(12):1970-1976.
18. Slater M, Perruccio AV, Badley EM. Musculoskeletal comorbidities in cardiovascular disease, diabetes and respiratory disease: the impact on activity limitations; a representative population-based study. BCM Public Health. 2011;11:77. doi: 10.1186/1471-2458-11-77.
19. Ryan CG, McDonough S, Kirwan JP. An investigation of association between chronic musculoskeletal pain and cardiovascualr disease in the Health Survey for England (2008). Eur J Pain. 2014;18(5):740-750.
20. Burke FJ, Main JR, Freeman R. The practice of dentistry: an assessment of reasons for premature retirement. Br Dent J. 1997;182(7):250-254.
21. Applegate KA, Thiese MS, Merryweather AS, et al. Association between cardiovascular disease risk factors and rotator cuff tendinopathy: a cross-sectional study. J Occup Environ Med. 2017;59(2):154-160.
22. Stubbs B, Vancampfort D, Veronese N, et al. Depression and pain: primary data and meta-analysis among 237 952 people across 47 low- and middle-income countries. Psychol Med. 2017;22:1-12.
23. Canadian Mental Health Association. The relationship between mental health, mental illness and chronic physical conditions. https://ontario.cmha.ca/documents/ the-relationship-between-mental-health-mental-illness-and-chronic-physical-conditions/. Published December 2008. Accessed August 22, 2017.
24. American Psychological Association. Stress effects on the body. http://www.apa.org/helpcenter/stress-body.aspx. Accessed August 22, 2017.
25. Taib MFM, Bahn S, Yun MH, Taib MSM. The effects of physical and psychosocial factors and ergonomic conditions on the prevalence of musculoskeletal disorders among dentists in Malaysia. Work. 2017;57(2):297-308.
26. Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287-333.
27. Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317-332.
28. Andersson HI. Increased mortality among individuals with chronic widespread pain relates to lifestyle factors: a prospective population-based study. Disabil Rehabil. 2009;31(24):1980-1987.
29. Tüzün EH. Quality of life in chronic musculoskeltal pain. Best Pract Res Clin Rheumatol. 2007;21(3):567-579.
30. Finsen L, Christensen H, Bakke M. Musculoskeletal disorders among dentists and variation in dental work. Appl Ergon. 1998;29(2):119-125.
31. Alexopoulos EC, Stathi IC, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet Disord. 2004;9(5):16. doi: 10.1186/1471-2474-5-16.
32. Rundcrantz BL, Johnsson B, Moritz U. Cervical pain and discomfort among dentists. Epidemiological, clinical and therapeutic aspects. Part 1. A survey of pain and discomfort. Swed Dent J. 1990;14(2):71-80.
33. Memarpour M, Badakhsh S, Khosroshahi SS, Vossoughi M. Work-related musculoskeletal disorders among Iranian dentists. Work. 2013;45(4):465-474.
34. Valachi B. Practice Dentistry Pain-Free: Evidence-Based Strategies to Prevent Pain and Extend Your Career. Portland, OR: Posturedontics Press;2008.
35. Hamilton A. Cumulative trauma disorder. National Safety Council. http://www.safetyandhealthmagazine.com/ articles/cumulative-trauma-disorder. Published June 1, 2013. Accessed August 22, 2017.
36. Solomonow M. Neuromuscular manifestations of viscoelastic tissue degradation following high and low risk repetitive lumbar flexion. J Electromyogr Kinesiol. 2012;22(2):155-175.
37. Reuther KE, Thomas SJ, Tucker JJ, et al. Scapular dyskinesis is detrimental to shoulder tendon properties and joint mechanics in a rat model. J Orthop Res. 2014;32(11):1436-1443.
38. Kanlayanaphotporn R. Changes in sitting posture affect shoulder range of motion. J Bodyw Mov Ther. 2014;18(2):239-243.
39. Oliveira Dantas FF, de Lima KC. The relationship between physical load and musculoskeletal complaints among Brazilian dentists. Appl Ergon. 2015;47:93-98.
40. Rafie F, Zamani Jam A, Shahravan A, et al. Prevalence of upper extremity musculoskeletal disorders in dentists: symptoms and risk factors. J Environ Public Health. 2015;2015:517346. doi: 10.1155/2015/517346.
41. Retrain Pain Foundation. Retrain pain. www.retrainpain. org. Accessed August 22, 2017.
42. Hall J, Guyton A. Textbook of Medical Physiology. 11th ed. Elsevier; 2005.
43. Geuter S, Büchel C. Facilitation of pain in the human spinal cord by nocebo treatment. J Neurosci. 2013;33(34);13784-13790.
44. Ghoneim MM, O’Hara MW. Depression and postoperative complications: an overview. BMC Surg. 2016;16:5. doi: 10.1186/s12893-016-0120-y.
45. Barbosa DC, Ângelos JSD, Macena GMJ, et al. Effects of ozone on the pain and disability in patients with failed back surgery syndrome. Rev Assoc Med Bras. 1992;63(4):355-369.
46. Sahin N, Karahan AY, Devrimsel G, Gezer IA. Comparison among pain, depression, and quality of life in cases with failed back surgery syndrome and non-specific chronic back pain. J Phys Ther Sci. 2017;29(5):891-895.
47. Neumann, DA. Kinesiology of the Musculoskeletal System. Mosby; 2002.
48. Kendall FP, McCreary EK, Provance PG, et al. Muscles: Testing and Function With Posture and Pain. Baltimore, MD: Lippincott Williams & Wilkins.
49. Apostolopoulos N, Metsios GS, Flouris AD, et al. The relevance of stretch intensity and position—a systematic review. Front Psychol. 2015;18(6):1128. doi: 10.3389/fpsyg.2015.01128.
50. Viriyatharakij N, Chinkulprasert C, Rakthim N, et al. Change of pectoralis minor length, andacromial distance, during scapular retraction at 60° shoulder elevation. J Bodyw Mov Ther. 2017;21(1):53-57.
51. Schüldt K, Harms-Ringdahl K. Activity levels during isometric test contractions of neck and shoulder muscles. Scand J Rehabil Med. 1988;20(3):117-127.
52. Falla D, O’Leary S, Fagan A, Jull G. Recruitment of the deep cervical flexor muscles during postural-correction exercise performed in sitting. Man Ther. 2007;12(2):139-143.
53. Dutton M. Orthopaedic Examination, Evaluation, and Intervention. New York, NY: McGraw-Hill Medical.
54. Sung PS. New perspective: outcome measurement indices for yoga therapy. J Yoga Phys Ther. 2014;4:157. doi: 10.4172/2157-7595.1000157.
55. Hokwerda O, Wouters JAJ, de Ruijter RAG, Zijlstra-Shaw S. Ergonomic Requirements for Dental Equipment. European Society of Dental Ergonomics. 2007.
56. Abdelraouf OR, Abdel-Aziem AA. The relationship between core endurance and back dysfunction in collegiate male athletes with and without nonspecific low back pain. Int J Sports Phys Ther. 2016;11(3)337-344.
57. Waongenngarm P, Rajaratnam BS, Janwantanakul P. Internal oblique and transversus abdominis muscle fatigue induced by slumped sitting posture after 1 hour of sitting in office workers. Saf Health Work. 2016;7(1):49-54.
58. Heller-Ono A. The ergonomics of posture with Alison Heller-Ono [podcast]. United States: J. Benedict. 2017.
59. Valachi B. Dental ergonomics with Bethany Valachi: Dentistry uncensored with Howard Farran [podcast]. Dentaltown. com. http://www.dentaltown.com/blog/post/3933/304-dental-ergonomics-with-bethany-valachi-dentistry-uncensored-with-howard-farran. Accessed September 6, 2017.
60. Lin MY, Barbir A, Dennerlein JT. Evaluating biomechanics of user-selected sitting and standing computer workstation. Appl Ergon. 2017;65:382-388.
61. Balogh I, Ohlsson K, Nordander C, et al. The importance of work organization on workload and musculoskeletal health- -Grocery store work as a model. Appl Ergon. 2016;53:143-151.
Disclosure
The author has no disclosures to report.
About the Author
Juanita Benedict, DPT, CEAS II
Dental Ergonomic Consultant, Orlando, Florida