You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Oral pathology is a visual specialty, and clinical images can facilitate your learning the clinical features of oral mucosal lesions. Several atlases are recommended in the Additional Resources section of this course. The textual material in this course is designed to be used with The Oral Pathology Image Database (Atlas): http://guides.lib.uiowa.edu/c.php?g=131885&p=864394.
Please note that lesions or diseases discussed in the textual material that have clinical images available on The Oral Pathology Image Database are designated with *.
Part I: Introduction to Clinical Differential Diagnosis
Diagnosing lesions of the oral mucosa is necessary for the proper management of patients. Clinical differential diagnosis is the cognitive process of applying logic and knowledge, in a series of step-by-step decisions, to create a list of possible diagnoses. Differential diagnosis should be approached on the basis of exclusion. All lesions that cannot be excluded represent the initial differential diagnosis and are the basis for ordering tests and procedures to narrow the diagnosis. Guessing what the one best diagnosis is for an oral lesion can be dangerous for the patient because serious conditions can be overlooked.
It is helpful for clinicians to organize their knowledge of oral pathology using a system that simulates the clinical appearance of oral lesions. A decision tree is a flowchart that organizes information so that the user can make a series of step-by-step decisions and arrive at a logical conclusion (Figure 1).
How to Use the Decision Tree
To use the decision tree, the clinician begins at the left side of the tree, makes the first decision, and proceeds to the right. The names of individual lesions are listed on the far right of the tree. Any lesion or group of lesions that cannot be excluded becomes part of the clinical differential diagnosis.
The first decision to make when using the decision tree is whether the lesion is a surface lesion or soft tissue enlargement.
Surface lesions consist of lesions that involve the epithelium and superficial connective tissue of mucosa and skin. They do not exceed 2-3 mm in thickness. Surface lesions are divided into three categories based on their clinical appearance: white, pigmented, and vesicular-ulcerated-erythematous. Each of these categories is further subclassified as shown in Table 1 through Table 3.
Soft tissue enlargements are swellings or masses that are divided into two categories: reactive and tumors in Table 4. The term tumor is used in the clinical sense of an enlargement and is not based on microscopic criteria or basic pathologic process. For example, irritation fibroma is classified as a tumor because this lesion is persistent and progressively increases in size, although most people agree that the true pathogenesis is that of a reactive process secondary to chronic irritation.
Reactive soft tissue enlargements may increase and decrease (fluctuate) in size and usually eventually regress. Reactive enlargements are often, but not always, tender or painful and usually have a more rapid growth rate (measured in hours to weeks) than tumors. Some reactive enlargements begin as a diffuse lesion and become more localized with time. Sometimes reactive lesions are associated with tender lymph nodes and systemic manifestations, such as fever and malaise. Once it is decided that a soft tissue enlargement is reactive, the next step is to determine what the lesion is reacting to, such as bacterial, viral, or fungal infections or chemical or physical injury.
Soft tissue tumors are characterized by being persistent and progressive; they do not resolve without treatment. They are usually not painful early in their development, and the growth rate varies from weeks to years.
Benign and Malignant Tumors
If a soft tissue enlargement appears to be a tumor, the clinician must next determine if the enlargement is benign or malignant. Benign tumors are typically better defined or circumscribed and have a slower growth rate, measured in months and years, than malignant neoplasms. Malignant neoplasms are more likely to be painful and cause ulceration of the overlying epithelium than benign lesions. Since malignant neoplasms invade or infiltrate surrounding muscle, nerve, blood vessels, and connective tissue, they are fixed or adherent to surrounding structures during palpation. Some benign tumors are also fixed to surrounding structures, but other benign tumors are surrounded by a fibrous connective tissue capsule, which may allow the lesion to be moved within the tissue independent of surrounding structures.
Benign tumors can be subdivided into four categories: epithelial, mesenchymal, and salivary gland tumors, and cysts of soft tissue. Although soft tissue cysts are not tumors, their historical and clinical features resemble those of benign tumors. Each of these categories is further subclassified as shown in Table 5 through Table 8.
It should be emphasized that the clinical descriptions above are general guidelines, and exceptions occur. Removal of the lesion and microscopic examination of the tissue is the only way to arrive at a definitive diagnosis.
Part II: Surface Lesions of Oral Mucosa
Remember that surface lesions of oral mucosa consist of lesions that involve the epithelium and/ or superficial connective tissue. They do not exceed 2-3 mm in thickness. Clinically, surface lesions are flat or slightly thickened rather than being swellings or enlargements.
We initially divide surface lesions into three categories based on their clinical appearance: white, pigmented, and vesicular-ulcerated-erythematous.
White Surface Lesions of Oral Mucosa
Surface lesions of oral mucosa that appear white, tan, or light yellow are divided into three groups based on their clinical features:
1. White lesions due to epithelial thickening
2. White lesions due to accumulation of necrotic debris on the mucosal surface
3. White lesions due to subepithelial changes in the connective tissue.
Epithelial thickening white lesions appear white because the pink to red color of the blood vessels in the underlying connective tissue is masked by the increased thickness of the epithelium. These lesions are asymptomatic, rough to palpation, and cannot be rubbed off with a gauze. They appear flat white when dried.
Three of the epithelial thickening white lesions occur on the tongue: hairy tongue, hairy leukoplakia, and geographic tongue (erythema migrans).
Hairy tongue* (Figure 2) is the result of the accumulation of keratin on the dorsal surface of the tongue. Numerous causes have been proposed, but lack of mechanical stimulation to the dorsal tongue due to poor oral hygiene and/or a soft diet are probably the most important causes. The lesion presents as elongated filiform papillae having a hair-like appearance. The papillae are typically stained brown, black or other colors depending on the patient’s diet and habits. Hairy tongue is typically not painful. Hairy tongue is not a serious condition, but warrants treatment for cosmetic and hygienic reasons. Treatment involves using a toothbrush, tongue blade, or tongue scraper to brush or scrape the dorsal surface of the tongue. The prognosis is good.
Hairy leukoplakia is caused by Epstein-Barr virus and presents as unilateral or bilateral, asymptomatic, white, rough patches, usually on the lateral surfaces of the tongue. It most commonly occurs in HIV positive patients but can also be found in any immunocompromised patient. Hairy leukoplakia does not require treatment, but it should alert the clinician that the patient is immunocompromised.
White Surface Lesions
Erythema migrans (geographic tongue, benign migratory glossitis) (Figure 3) is a common, harmless lesion that can typically be diagnosed by its clinical features. It presents as multiple red patches surrounded by a thickened, irregular, white border. A lesion will resolve in one area and appear in other areas (migrate). This condition is usually not painful and requires no treatment. If the patient complains of pain or burning with the lesions, a diagnosis of candidosis should be considered. Rarely, lesions of erythema migrans can be found on oral mucosal surfaces other than the tongue.
Nicotine stomatitis* (Figure 4) is an epithelial thickening lesion of the hard palate caused by heat from smoking a pipe, cigar, or occasionally cigarettes. The lesion is white, rough, asymptomatic, and leathery appearing and contains numerous red dots or macules. The red macules represent inflamed salivary gland duct orifices. Nicotine stomatitis is not considered a premalignant lesion and does not need to be biopsied. However, the patient should be encouraged to stop smoking, and the oral mucosa should be evaluated periodically. The prognosis for nicotine stomatitis is good, but the patient is at increased risk to develop cancer in other locations in the upper aerodigestive tract.
White sponge nevus* (Figure 5) is a genetic disorder, usually congenital or developing in childhood. The oral mucosa is diffusely white, rough, thickened and folded. The most common location is the buccal mucosa bilaterally, but other oral mucosal areas may be involved. Nasal, pharyngeal, and anogenital mucosa may be affected. The condition is not painful. Other family members often have the condition. The clinical features and history are diagnostic. This condition is benign and requires no treatment. The prognosis is excellent.
Leukoedema is a generalized white change of oral mucosa which is probably a variation of normal rather than a disease. The cause is unknown. It occurs much more commonly in blacks than whites. Leukoedema is diffuse and symmetrically distributed on the buccal mucosa and may extend onto the labial mucosa. The appearance is gray-white, opaque, or milky. It can be smooth to palpation or wrinkled, and it does not rub off. A characteristic clinical feature is that the white appearance decreases when the buccal mucosa is stretched. Leukoedema is asymptomatic, and the patient is unaware of its presence. Leukoedema is diagnosed clinically, and a biopsy is not required. No treatment is necessary. It is a benign lesion and is not premalignant.
Lichen planus* (Figure 6) is a chronic inflammatory disease involving skin and oral mucosa. It represents an immune abnormality involving T lymphocytes sensitized to antigens in the overlying stratified squamous epithelium. Often it is associated with medications the patient is taking, and it is then called a lichenoid mucositis secondary to medications. Classic lichen planus and drug-related lichenoid mucositis appear identical clinically and microscopically.
Skin lesions of lichen planus (Figure 7) consist of pruritic (itching), erythematous to light purple patches, sometimes with an overlying network pattern of white lines or striations. Oral lesions most commonly appear as white epithelial thickening arranged in a network pattern (Wickham’s striae) with erythema of the surrounding mucosa. White patches, erythematous erosions, and ulcers may also occur. The white lesions are not painful, but the erosions and ulcers are usually painful. Lichen planus almost always has multiple lesions bilaterally, with the buccal mucosa commonly involved. Oral lesions may occur with or without skin lesions.
An incisional biopsy is required for definitive diagnosis. Asymptomatic lesions require no treatment other than inspection during annual dental visits. Topical and/or systemic corticosteroids will almost always control, but not cure, painful erosions and ulcers of lichen planus. Candidal overgrowth (candidosis) is common in patients with lichen planus and should be treated with antifungal medications.
The term “leukoplakia” refers to a clinically white mucosal thickening lesion that cannot be further defined. Most “leukoplakia” will be shown microscopically to be hyperkeratosis, with or without epithelial dysplasia, carcinoma in situ, or superficially invasive squamous cell carcinoma. Leukoplakia is a clinical description and not a diagnosis, and the term will not be used further in this discussion.
Hyperkeratosis (focal keratosis)* (Figure 8) is a microscopic term meaning increased thickness of the keratin layer of stratified squamous epithelium with no microscopic evidence of atypical epithelial cells. Clinically, hyperkeratotic lesions appear as white, rough, non-painful patches that do not rub off. They are often secondary to chronic irritation, such as biting or tobacco use.
Hyperkeratotic lesions on oral mucosal surfaces that are normally keratinized, such as dorsum of the tongue, hard palate, and attached gingiva, sometimes represent a physiologic response (callus) to chronic irritation. These lesions will usually resolve if the irritant is removed. Hyperkeratotic lesions on surfaces that are normally nonkeratinized are potentially more serious and should be biopsied if they do not resolve if irritants are removed. Remember, however, that dysplasia, carcinoma in situ, and squamous cell carcinoma can occur on any oral mucosal surface.
Epithelial dysplasia is atypical or abnormal growth of the stratified squamous epithelium lining a mucosal surface. It is a diagnosis that must be made microscopically. These lesions appear clinically as white, rough, non-painful areas, or non-painful red patches (“erythroplakia” or “erythroplasia”), or patches that demonstrate both red and white areas. Because these lesions are asymptomatic, the patient is usually not aware of them. Some lesions diagnosed as epithelial dysplasia will progress to squamous cell carcinoma, while others will resolve. Since it is impossible to determine by microscopic examination which lesions will progress or resolve, treatment is complete surgical excision, if possible, and follow-up.
Carcinoma in situ* (Figure 9) is cancer of the oral epithelium which is confined to the epithelial layer. It presents most commonly as a persistent red plaque (erythroplakia) or a mixed white and red plaque. It may also appear as a white plaque. Complete removal is the treatment. When completely removed, the prognosis is excellent, although the patient is at increased risk of developing new lesions at other locations on the oral mucosa.
Squamous cell carcinoma* (Figure 10 and Figure 11) is the most common malignant neoplasm of the oral cavity. Tobacco and alcohol use and human papilloma virus infection have been identified as risk factors, but squamous cell carcinoma can occur in patients with no known risk factors. Squamous cell carcinoma can occur anywhere on the oral mucosa, but is most common on the ventral and lateral surfaces of the tongue, floor of the mouth, soft palate, tonsillar pillar area, and retromolar trigone areas.
Superficially invasive, or early, squamous cell carcinoma lesions appear as surface lesions rather than soft tissue enlargements. They are almost invariably non-painful, and thus patients do not know they have a lesion. Early lesions may be white rough epithelial thickening lesions, red persistent non-painful lesions, or a combination of the two.
It is important to recognize squamous cell carcinoma in its early stages when cure is possible without disfiguring surgery. The main treatment for oral squamous cell carcinoma is complete surgical excision. Lymph node dissection is performed when lymph nodes are involved. Radiation therapy is often used as an adjunct to surgery. Chemotherapy is reserved for palliative therapy.
Surface Debris White Lesions
Surface debris white lesions are associated with necrosis of the overlying epithelium. The necrotic epithelium can be removed with a gauze leaving an erythematous or ulcerated base. Surface debris lesions are usually painful.
A burn of oral mucosa can be caused by heat or chemicals. It presents as a painful ulcer covered by a white to yellow surface. Often the patient can provide a history of burn to confirm the diagnosis. A burn will resolve spontaneously.
Fibrin clot* (Figure 12) refers to coagulated protein present on the surface of an ulcer. A fibrin clot appears clinically as a tan or yellow surface lesion usually surrounded by an erythematous halo associated with the ulcer. It can be rubbed off. There may be a history of injury or a mucosal disease associated with ulcers. Management should be aimed at treating the cause of the ulcer, as the fibrin clot resolves with the ulcer.
Candidosis (candidiasis)* (Figure 13) is a common cause of oral discomfort. Predisposing factors include immunosuppression, antibiotic therapy, xerostomia and use of dentures. Oral lesions may appear as white plaques, which rub off leaving an erythematous base. Diffuse painful erythematous mucosa is another common presentation. Nail and/or vaginal lesions may also be present. A wide variety of topical and systemic antifungal agents are used for management.
White Lesions Due to Subepithelial Change
White lesions due to subepithelial change have normal overlying epithelium, but changes in the connective tissue partially mask blood vessels and cause the area to appear white, yellow or tan. These lesions have a smooth translucent surface, do not rub off, and are not painful.
Gingivial cyst of the newborn* (Figure 14) is also known as dental lamina cyst of the newborn. This is an epithelial inclusion cyst found on the attached alveolar mucosa of infants. It presents as an asymptomatic white thickened surface lesion. Similar cysts occur on the hard palate. No treatment is necessary as the lesions resolve spontaneously within several weeks after birth.
Fordyce granules* (Figure 15) appear as flat or slightly elevated, yellow clusters, most commonly located on the buccal mucosa and lip. They represent sebaceous glands. Fordyce granules are harmless and require no treatment.
Scarring (subepithelial fibrosis) of the oral mucosa can appear as white surface lesions with a smooth surface. They are non-painful and do not rub off. Diagnosis is made by history of trauma or surgery to the area. No treatment is necessary.
Pigmented Surface Lesions of Oral Mucosa
Pigmented surface lesions of oral mucosa appear blue, brown, or black. They are classified as generalized lesions, which are diffuse and multifocal, and localized lesions, which are unilateral and involve only one or several locations. Note that some soft tissue enlargements are pigmented, but they are discussed under Soft Tissue Enlargements.
Generalized Pigmented Surface Lesions of Oral Mucosa are bilateral, multiple and diffuse. There are numerous causes for generalized pigmentations, varying from common to rare, and the most important are discussed below.
Hereditary (racial, ethnic, physiologic)* pigmentation is the most common type of generalized pigmentation. The pigmentation is diffuse, symmetrical, and most apparent on the gingiva and labial mucosa. In general, the extent of oral mucosal pigmentation is directly related to the extent of skin pigmentation.
Pregnancy can lead to multiple melanotic macules on oral mucosa and facial skin (melasma or chloasma). No treatment is necessary for the melanin pigmentation, and it typically fades after the pregnancy.
Numerous medications*, such as quinine drugs used in the treatment of systemic lupus erythematosus, can cause diffuse pigmented lesions.
Smoker’s melanosis is caused by stimulation of melanin production by melanocytes due to chemical substances in cigarette smoke. The anterior facial gingiva is most commonly involved, although any oral mucosal site can demonstrate this. Often smoker’s melanosis can be clinically diagnosed by correlating a history of smoking with the location and distribution of the pigmentation. If the diagnosis is not evident, then biopsy is indicated. No therapy other than smoking cessation is necessary once the diagnosis has been made.
Ingestion of, or exposure to, heavy metals*, such as lead, mercury, gold, arsenic and bismuth, can lead to diffuse pigmentation of oral mucosa. The pigmentation may be dark blue, gray or black and commonly involves the marginal gingiva. Diffuse mucosal ulceration and a metallic taste may also be noted. Extraoral manifestations may be a clue to the diagnosis, and include dermatitis, tremors, mental changes, headache, fatigue, and gastrointestinal upset. Management of suspected heavy metal intoxication involves referral for diagnostic workup.
Peutz-Jeghers syndrome is a genetic condition characterized by numerous freckle-like lesions on the skin of the hands and around the mouth, nose and anogenital region. Intra-oral freckles may involve the lips, tongue and buccal mucosa. Patients also have multiple polyps, mainly in the small intestine. The polyps sometimes result in intestinal obstruction. Patients have an increased risk of gastrointestinal carcinoma but the polyps are not premalignant. Newly diagnosed patients with this syndrome should be referred for evaluation of the gastrointestinal tract.
Neurofibromatosis (von Recklinghausen’s disease of skin) (Figure 16) is a genetic disease with multiple subtypes. Type I is the most common type and is characterized by multiple neurofibromas. The neurofibromas vary in size, number, and may be well circumscribed or diffuse. Melanotic macules called café-au-lait spots, at least 1.5 cm in diameter and numbering 6 or more, are diagnostic of neurofibromatosis. Axillary freckles are also common. Numerous other systemic manifestations may be present in neurofibromatosis. Central nervous system abnormalities are especially prominent. There is no definitive treatment for neurofibromatosis. See also the discussion of neurofibromatosis with neurofibroma.
Polyostotic fibrous dysplasia is a systemic syndrome in which diffuse bony lesions of fibrous dysplasia involve multiple areas of the skeleton. The McCune-Albright syndrome includes polyostotic fibrous dysplasia, café-au-lait melanotic macules, and endocrine abnormalities, such as precocious puberty in females. The Jaffe- Lichtenstein syndrome includes polyostotic fibrous dysplasia plus café-au-lait pigmentation without endocrine abnormalities.
Note that the vast majority of cases of fibrous dysplasia of the jaws occur as a solitary (monostotic) lesion rather than as part of the polyostotic syndrome. Monostotic fibrous dysplasia does not have generalized café-au-lait pigmentations.
In Addison’s disease* (Figure 17) the adrenal cortex is destroyed, resulting in decreased production of cortisol, aldosterone and adrenal androgens. Signs and symptoms include weakness, anorexia, nausea, vomiting, diarrhea, abdominal pain, decreased serum sodium, and hypotension. Diffuse pigmentation of skin and oral mucosa typically occur in Addison’s disease. Treatment consists of replacement therapy with glucocorticoids and mineral corticoids. The prognosis is good with appropriate therapy.
Localized Pigmented Surface Lesions of Oral Mucosa
Localized pigmented surface lesions are divided into 4 categories based on their cause and clinical features.
Intravascular Blood Lesions appear red, blue or purple due to an increased amount of blood within blood vessels as a result of increased number or size of blood vessels. Firm palpation of the lesions causes them to blanch because the blood is displaced.
Hemangioma* (Figure 18) is a proliferation of blood vessels which usually is noted at birth or early childhood. It may be well circumscribed or diffuse. The arteriovenous malformation is a different lesion. It represents a direct communication between an artery and a vein, and it will demonstrate a thrill and bruit. A hemangioma requires no treatment unless it is a functional or cosmetic problem. Many hemangiomas will regress spontaneously during childhood. Incision of an arteriovenous malformation may lead to fatal hemorrhage.
A varix* (Figure 19) is a dilated vein or venule. It presents as a relatively small, localized, elevated, blue or purple lesion. It is compressible and blanches upon pressure unless a thrombus has formed within it. A thrombosed varix is firm and does not blanch. Varices are most common on the ventral surface of the tongue, floor of the mouth, lips, and buccal mucosa. Varices increase in number with age and may also be the result of trauma. Once a varix has been diagnosed it needs no further treatment. A thrombosed varix often cannot be clinically distinguished from a nevus, and biopsy and microscopic examination are necessary to establish a definitive diagnosis.
Kaposi’s sarcoma* (Figure 20) is a malignant vascular neoplasm most commonly seen in patients with HIV infection, organ transplants or other causes of immune suppression. It appears as a flat or slightly elevated, blue to purple plaque on skin and oral mucosa. The lesion may develop into a compressible soft tissue enlargement that sometimes blanches on pressure. Oral lesions occur most commonly on the hard palate and gingiva. Treatment for oral Kaposi’s sarcoma includes systemic or intralesional chemotherapy and surgical excision. Prognosis depends on the systemic health status of the patient.
Extravascular Blood Lesions
Extravascular Blood Lesions are due to the presence of blood outside of blood vessels. They do not blanch and typically resolve within a month. The patient often has a history of trauma or bleeding problem.
Ecchymosis* (Figure 21) is a bruise. It occurs due to hemorrhage and accumulation of blood in the connective tissue. It is usually the result of trauma, but may also be secondary to deficiency of platelets and/or clotting factors and viral infections. An ecchymosis is typically flat and red, purple, or blue in color. If the ecchymosis is due to trauma, then it will resolve spontaneously and no treatment is necessary. If it is secondary to a systemic disease, then further workup is indicated.
A hematoma* (Figure 22) is the result of hemorrhage, with pooling of blood in the connective tissue. A hematoma causes thickening or enlargement of the mucosa. It is purple to black in color. No treatment is necessary once a diagnosis is made. A hematoma will resolve spontaneously in several weeks to over a month.
Petechiae* (Figure 23) are round, red, pinpoint areas of hemorrhage. Petechiae are usually caused by trauma, viral infection, or a bleeding problem. They resolve over a few weeks. Petechiae do not require treatment. Investigation of the cause of petechiae may be indicated.
Melanocytic Lesions
Melanocytic Lesions appear brown or black due to the deposition of melanin.
Ephelis* is a freckle. It is flat, brown or black in color, and occurs on sun-exposed surfaces. It is due to increased production of melanin by melanocytes. An ephelis requires no treatment.
Oral melanotic macule* (Figure 24) is a localized pigmented lesion associated with increased melanin pigmentation of the stratified squamous epithelium. It is asymptomatic, flat and not thickened, and appears similar to an ephelis (freckle) of skin. It is a harmless lesion, but its significance lies in distinguishing it from nevus or early melanoma. A biopsy should be performed if any doubt exists about the diagnosis.
If an oral pigmented lesion is not thickened, but is larger in diameter, has any variation in color, cannot be diagnosed as tattoo based on radiographic findings, or has irregular borders it should be excised.
Melanocytic Nevus* (Figure 25) is a benign proliferation of nevus cells (melanocytes). Nevi of skin first appear in childhood and progress through a series of clinical and microscopic stages. Most people have between 10 and 40 nevi on their skin. Nevi of skin that have uniform color and borders and are not changing in size or surface texture are not considered premalignant lesions and do not need to be removed unless they are chronically irritated or are a cosmetic problem. Nevi of oral mucosa are relatively rare. They occur most commonly on the gingiva and hard palate. Nevi of oral mucosa should be completely excised because they cannot be differentiated from melanoma based on their clinical features.
Melanoma* (Figure 26) is a malignant neoplasm of melanocytes. Melanoma of skin has increased significantly in incidence, while melanoma of oral mucosa is relatively rare. The most important clinical features of cutaneous melanoma are asymmetry of the lesion, variation in color (brown, black, red, white, blue), and diameter greater than 6 mm. Oral melanoma begins as an irregular, brown to black macule. Later the lesion will develop thickening and sometimes ulceration. The most common locations are the hard palate, gingiva, and alveolar ridge. It is not possible to distinguish an oral melanocytic nevus from early melanoma. If oral nevus and/or melanoma are included in the clinical differential diagnosis, then a biopsy is indicated. Biopsy is also indicated for flat, non-thickened pigmentations that are changing or have atypical color, borders, or size. Treatment for melanoma is complete surgical excision. The thickness of the lesion and depth of invasion are the most important prognostic factors.
Tattoo
Tattoo* (Figure 27) is a localized pigmented area caused by implantation of foreign material into skin or oral mucosa. Oral tattoos are usually caused by amalgam particles or graphite in lead pencils. A tattoo is localized, dark gray to black, non-tender, and either macular or slightly thickened. A tattoo sometimes increases in size due to ingestion of the foreign material by phagocytes and then migration of these cells. Some tattoos can be visualized on a radiograph, but absence of radiographic evidence of amalgam particles does not exclude the diagnosis of tattoo. Obviously, some tattoos are intentional artistic endeavors and do not cause a diagnostic challenge. The typical small, localized, non-thickened tattoo does not require treatment, once a diagnosis is made. A tattoo that is thickened and does not have amalgam particles evident on a radiograph should be biopsied so that nevus and melanoma can be excluded.
Vesicular-Ulcerated-Erythematous Surface Lesions of Oral Mucosa
Numerous diseases cause ulcers of the oral mucosa. Once an ulcer forms, regardless of the disease, it results in discomfort. For that reason, differential diagnosis of oral mucosal ulcers is important to both patients and health care providers. Sometimes ulcers are preceded by blisters, but it is often impossible to determine if a blister was present because blisters in the oral cavity rapidly rupture. Small blisters (2-5 mm) are called vesicles, whereas larger blisters (greater than 5 mm) are called bullae (singular bulla).
In some diseases applying lateral pressure to an area of normal appearing skin or mucosa may cause formation of a blister. This phenomenon is known as a Nikolsky sign (Figure 28). A Nikolsky sign may be present in epidermolysis bullosa, pemphigus, mucous membrane pemphigoid, lichen planus and lupus erythematosus. Not all patients with these diseases demonstrate a Nikolsky sign.
A thorough history should be obtained from patients with vesicular-ulcerative diseases and should include the following questions:
1. How long have the lesions been present? This helps distinguish between acute and chronic diseases. Genetic diseases are often present from birth or early childhood.
2. Are the lesions recurrent? If yes:
a. How often do they recur?
b. How long does it take for each lesion to heal? Recurrent oral ulcers that heal in the same amount of time for a particular patient are characteristic of aphthous ulcers and recurrent herpes.
c. Do they recur in the same locations? Recurrent herpetic lesions typically recur in the same location.
3. Has the patient noticed blisters? If blisters are seen, the following diseases can be excluded from the differential diagnosis: aphthous ulcers, ulcers of infectious mononucleosis, traumatic ulcers, and ulcers due to bacteria.
4. Has the patient noticed lesions on the skin, eyes, or genitals? Some systemic diseases may occur with extraoral lesions.
5. Has the patient had fever, malaise, lymphadenopathy in association with the lesions? A positive response may indicate an infectious agent, usually viral, caused the lesion.
6. What medications does the patient take? Medications may cause oral ulcers.
7. Have other family members had similar lesions? Epidermolysis bullosa is usually a familial disease.
Vesicular-ulcerative-erythematous lesions are categorized based on their cause, if known. Lesions are classified as hereditary, autoimmune, viral, mycotic (candidosis or candidiasis), and idiopathic (unknown cause). Bacteria rarely cause oral ulcers and are not discussed here.
Hereditary Diseases: Epidermolysis Bullosa
Epidermolysis bullosa* refers to a group of mostly inherited diseases which cause blisters and ulcers of skin and sometimes oral mucosa. In almost all patients the lesions begin at birth or early childhood, and there is often a familial history of the condition. A Nikolsky sign may be present. Lesions of skin are consistently present. Some forms of epidermolysis bullosa can result in scarring and restricted mouth opening. Enamel defects of the teeth can also be present.
There is no cure for this group of diseases. The severity varies from mild (in the simplex form) to fatal (in the junctional and recessive forms). Antibiotics may be necessary to control infection associated with blisters and ulcers.
Autoimmune Diseases
Autoimmune diseases are characterized by blisters and painful ulcers of slow onset. The lesions may get better and worse, but they are persistent and chronic. Lesions do not heal in a predictable period of time. Lymphadenopathy is typically not present.
Pemphigus vulgaris* is a painful autoimmune disease in which the patient forms antibodies to a component of desmosomes located in the stratified squamous epithelium. This results in loss of adherence of epithelial cells and the formation of intraepithelial blisters. The blisters are fragile and quickly rupture forming painful ulcers or erosions which heal slowly. Large areas of skin and mucosa can be involved and may cause serious problems with infection. A Nikolsky sign may be present. Oral lesions eventually form in almost all patients and may be the initial site of lesions. Pemphigus usually begins in mid to late adult life.
Management of pemphigus vulgaris involves an incisional biopsy to establish a definite microscopic diagnosis. Immunofluorescence studies of biopsy material are necessary to make a definitive diagnosis of pemphigus. The disease is treated aggressively with corticosteroids or other immunosuppressive drugs. Without treatment the disease can be fatal. With aggressive treatment, the disease can often be managed successfully, but may still be fatal due to complications associated with the medications.
In mucous membrane pemphigoid (cicatricial pemphigoid)* (Figure 29) antibodies are directed against antigens in the basement membrane. This causes a separation between the surface epithelium and the underlying connective tissue, resulting in a subepithelial blister. Mucous membrane pemphigoid involves primarily oral mucosa, but mucosa of the nose, pharynx and vagina may also be involved, as well as the skin. A Nikolsky sign may be present. Mucosal and skin blisters rupture to form painful ulcers. Involvement of the gingiva can lead to sloughing of the epithelium, sometimes called desquamative gingivitis. Desquamative gingivitis can also be present in lichen planus and pemphigus. Mucous membrane pemphigoid is also known as cicatricial pemphigoid because the ulcers can cause scarring of the mucosa and conjunctiva leading to blindness. It is most common in middle-aged and older adults.
Without treatment it usually requires weeks to months for the ulcers to heal. Mucous membrane pemphigoid may appear clinically similar to pemphigus vulgaris and erosive lichen planus. An incisional biopsy with immunofluorescence studies is important to establish a definitive diagnosis. Mucous membrane pemphigoid cannot be cured, but topical and systemic corticosteroids, as well as other medications, are used to control the disease. The disease has exacerbations and remissions, with or without treatment.
Bullous pemphigoid is a chronic autoimmune disease that involves the skin and, less commonly, the mucosa. The autoimmune reaction is directed against antigens in the basement membrane resulting in separation between the surface epithelium and the underlying connective tissue. Lesions consist of vesicles and bullae that rupture to form painful ulcers. Oral lesions in bullous pemphigoid resemble those of mucous membrane pemphigoid. Bullous pemphigoid does not cause scarring and tends not to be as chronic as mucous membrane pemphigoid. Bullous pemphigoid is managed with systemic corticosteroid medications. The prognosis is good.
Lupus erythematosus* (Figure 30) is an autoimmune disease that may be systemic or involve only skin and mucosa (discoid lupus). Both types can have skin and oral mucosal lesions. Skin lesions may present as erythematous or purple patches, sometimes covered with scales. The center of the lesion may become atrophic and scarred. Lesions are most common on sun-exposed surfaces. Skin lesions usually precede oral mucosal lesions. Oral lesions consist of erythematous patches, painful ulcers and erosions, and white rough epithelial thickening lesions. Candidiasis is common in patients with lupus. An incisional biopsy and direct immunofluorescence testing is usually required to establish the diagnosis of skin and oral mucosal lesions of lupus. Topical and systemic corticosteroids are used to control, but not cure, the lesions.
Idiopathic Diseases
Idiopathic diseases are those of unknown or poorly understood cause. These diseases do not have common historical and clinical features as a class or group, and thus each disease must be considered individually in the differential diagnosis.
Aphthous ulcers* (Figure 31) are a common cause of recurrent oral discomfort. The ulcers have an abrupt onset and resolve in a predictable amount of time for each patient, usually 7-14 days. Aphthous ulcers occur on nonkeratinized mucosal surfaces, such as buccal and labial mucosa, ventral surface of the tongue, floor of the mouth, and soft palate. A familial history is sometimes reported. The ulcers may be menstrually related. “Major” aphthous ulcers are larger and of longer duration than typical aphthae and often heal with scarring. “Herpetiform” aphthae refer to multiple crops of small aphthous ulcers.
Aphthous ulcers are most commonly treated with topical corticosteroids, such as triamcinolone acetonide, 0.1% mouthrinse. A short burst of systemic corticosteroids may be needed for persistent lesions. Intralesional injection of corticosteroids can also be of value for a larger, deeper lesion. It is important to explain to the patient that the goal of therapy is to control the lesions, and that there is currently no definitive cure.
Erosive lichen planus* is a chronic inflammatory disease involving skin and oral mucosa. It represents an immune abnormality involving T lymphocytes directed against antigens in the overlying stratified squamous epithelium. Occasionally lichen planus is associated with medications the patient is taking. The skin lesions consist of pruritic (itching), erythematous to light purple patches, sometimes with white striations. Oral lesions most commonly appear as white epithelial thickening arranged in a network pattern (Wickham’s striae) with erythema of the surrounding mucosa. White patches, erythematous erosions, and ulcers may occur with, or in place of, the striae. The white lesions are asymptomatic, but the erosions and ulcers are usually painful. Lichen planus almost always has multiple lesions bilaterally, with the buccal mucosa commonly involved. Oral lesions may occur without skin lesions. An incisional biopsy is required for diagnosis. Asymptomatic lesions require no treatment other than inspection during annual dental visits. Topical and/or systemic corticosteroids will almost always control, but not cure, symptomatic lesions. Candidal overgrowth is common in association with lichen planus and should be treated with antifungal medications.
Erythema multiforme* (Figure 32) is an idiopathic disease that involves an immunologic abnormality. It may be triggered by infection, especially with herpes simplex virus, or drugs, such as antibiotics. It is characterized by the acute onset of blisters and ulcers of skin and oral mucosa. The appearance of the skin lesions is variable. “Target” or “iris” lesions of the skin are characteristic but not present in all cases, and consist of a blister surrounded by erythematous rings. Oral mucosal blisters and ulcers are present in multiple locations and are painful. Hemorrhagic crusting of the lips is often present. Fever, malaise, and pharyngitis may precede the lesions. Stevens- Johnson syndrome is a severe form of erythema multiforme and demonstrates conjunctivitis and genital ulcers in addition to mucocutaneous lesions. Topical and/or systemic corticosteroids may be useful in treatment. Offending drugs should be discontinued. If it appears to be associated with herpes simplex infection, then anti-viral medications may be used. Erythema multiforme is typically benign and resolves spontaneously, although it may recur. Rarely, Stevens-Johnson syndrome may be fatal.
Medication-induced mucositis* (Figure 33): A number of different medications cause oral mucosal lesions that do not appear to be allergic reactions but rather represent a toxic side-effect of the medication. These mucosal lesions can present as nonspecific ulcers, erosions or may resemble erosive lichen planus. They occur on both keratinized and nonkeratinized mucosal surfaces, and are chronic lesions. They do not necessarily appear immediately after the patient begins taking the medication.
The first step in management is diagnosis. An incisional biopsy usually shows a nonspecific ulcer but may be useful in excluding other causes of chronic mucositis, such as erosive lichen planus and mucous membrane pemphigoid. After the diagnosis is made, the dentist should consult with the patient’s physician to see if a different medication can be used. Once the offending medication is withdrawn, the lesions resolve.
Contact stomatitis: Numerous chemical agents in food, candy, chewing gum, toothpaste, and mouthrinses can cause chronic mucositis. Flavoring agents, especially cinnamon flavoring, are common causes of contact stomatitis. The clinical features of contact stomatitis from cinnamon flavoring include mucosal pain, burning, erythema, edema, erosion, and ulceration. Hyperkeratosis often covers the erythematous areas producing a shaggy thickened surface. The lesions are diagnosed based on the clinical features and a history of cinnamon exposure. The lesions typically resolve within one week following discontinuation of the cinnamon products. Rarely, amalgam restoration or metal materials in crowns can cause a lichen planus-like reaction in the adjacent mucosa.
Erythroplasia (erythroplakia) is a clinical term corresponding microscopically to epithelial dysplasia, carcinoma in situ*, or superficially invasive squamous cell carcinoma*. It appears clinically as asymptomatic, persistent, erythematous, velvety, focal to diffuse mucosal areas. Because these lesions are asymptomatic, the patient is almost never aware of them.
Viral Diseases
Viral diseases typically have an acute or abrupt onset of multiple lesions. Systemic manifestations (including fever, malaise, lymphadenopathy, diarrhea, lymphocytosis) may be present. It is important to realize, however, that not all patients with viral diseases have systemic manifestations. All the viral diseases mentioned below, except for infectious mononucleosis, have a vesicle stage. Vesicles rupture rapidly and are often not apparent to patients or clinicians.
Herpes simplex virus* (HSV) types 1 and 2 commonly infect skin and oral mucosa. Type 1 preferentially involves mucosa and skin above the waist, while type 2 usually infects the genital area, but occasionally the pattern is reversed. Individuals infected with HSV will harbor latent virus in regional nerve ganglia for the remainder of their lives. Primary symptomatic infection with HSV involving the mouth is called primary herpetic gingivostomatitis* (Figure 34). Although primary herpes is most common in children, it can certainly occur in older adults without antibody to HSV.
Signs and symptoms of primary herpes include abrupt onset of fever, malaise, tender lymphadenopathy of the head and neck, and vesicles and ulcers anywhere on oral mucosa, the pharynx, lips and perioral skin. The gingiva is typically enlarged and erythematous. The lesions are painful, making it difficult to eat and drink. The lesions resolve spontaneously, usually within 10-14 days.
A number of systemic and topical antiviral drugs are available for patients needing treatment. An important consideration for drug therapy is that the earlier the treatment is initiated, the better the outcome. Supportive and symptomatic treatment includes maintaining hydration, especially in children, and systemic and topical analgesics.
The best documented causes of recurrent herpetic lesions* (Figure 35) are ultraviolet radiation, mechanical trauma, and immunosuppression. Recurrent herpes has vesicles and ulcers occurring on keratinized mucosal surfaces. The lesions are grouped in a tight cluster (Figure 36). Often a sudden prodrome of pain, tingling, or numbness precedes the onset of lesions. The frequency of recurrence varies with the individual. Resolution of lesions varies from 1 to several weeks but is constant for each person. Since herpetic lesions resolve spontaneously within a relatively short period of time, many patients do not request or require treatment.
Varicella (chickenpox)* (Figure 37) is the primary infection with the varicella-zoster virus. The disease begins with malaise, fever, pharyngitis, and lymphadenopathy. A pruritic skin rash begins on the face and trunk and spreads to the extremities. The skin lesions begin as vesicles which rupture and form crusts. They occur in successive waves or crops. Oral lesions may occur as vesicles which rupture to form non-painful ulcers. Varicella is usually a relatively mild, although annoying, infection in immunocompetent children. It tends to have more severe clinical features in adults. It can be quite serious in immunocompromised patients. Treatment is usually supportive and symptomatic in immunocompetent children. Antiviral medications, such as acyclovir, famciclovir, and valacyclovir, are useful in immunocompromised patients, adults, and infants. A vaccine for varicella is available. It appears to be highly effective, but the duration of immunity is not known.
Herpes zoster, or shingles* (Figure 38), represents reactivation of the varicella-zoster virus in a person previously infected. Zoster tends not to recur as frequently as herpes simplex. Zoster typically begins with the abrupt onset of pain, tingling, or numbness in the distribution of a sensory nerve. It is important to note that neuralgia associated with the prodrome stage of zoster may initially involve one or more teeth in a quadrant, thus simulating a toothache. Patients reporting pain in teeth that show no clinical or radiographic abnormalities should NOT have dental procedures performed on them in an attempt to eliminate the pain.
Neuralgia in the prodrome stage of zoster is followed by vesicles and ulcers similar in appearance to those caused by herpes simplex. Because the lesions follow a nerve distribution, they extend to the midline and stop. The vesicles and ulcers of zoster usually resolve within several weeks. However, the neuralgia may be extremely severe and persist for weeks to months. Antiviral drugs, when given early in the course of the disease, appear to be beneficial in reducing the neuralgia.
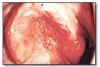
Herpangina* (Figure 39 and Figure 40), most commonly caused by Coxsackievirus A, presents with acute onset of mild fever, malaise, lymphadenopathy, pharyngitis, nausea and diarrhea. Many cases have no systemic manifestations. Oral lesions include vesicles and ulcers of the posterior oral mucosa, especially the soft palate and tonsillar pillar areas. Management includes analgesics, rest and encouraging the patient to drink plenty of fluids. Herpangina is typically a mild disease and resolves within approximately a week.
Hand, foot and mouth disease* (Figure 41) is an infection caused by Coxsackievirus A or B. It has abrupt onset of mild fever and pharyngitis. Oral lesions consist of vesicles and ulcers that may involve any area of oral mucosa. Skin lesions consist of erythematous macules and vesicles of the palms, soles, fingers and toes. The disease typically resolves within a week. Management includes analgesics, rest and encouraging the patient to drink plenty of fluids. The prognosis is good.
Infectious mononucleosis* (Figure 42) is a viral infection caused by Epstein-Barr virus. Infections in children may be asymptomatic. Symptomatic patients may demonstrate pharyngitis, cervical lymphadenopathy, fever, malaise, enlargement of liver and spleen, and sometimes a skin rash. Oral lesions are sometimes present and include palatal petechiae, hyperplasia of palatal tonsils, necrosis of surface mucosa overlying tonsils, and necrotizing ulcerative gingivitis. Diagnosis is confirmed by serologic testing for heterophil antibodies. Infectious mononucleosis is treated with rest and analgesics. It usually resolves within 4 to 6 weeks.
Rubeola (measles) is a potentially serious viral infection which can cause fever, malaise, cough, lymphadenopathy, pharyngitis, and an erythematous maculopapular skin rash. Oral lesions occur early in the disease and consist of red macules with white centers on the buccal mucosa, known as Koplik spots. The most important aspect of rubeola is the potential for complications to arise, including pneumonia and encephalitis. Vaccination is critically important. For infected patients, rest and supportive care is indicated. Rubeola is currently rare because of mandatory vaccination programs.
Mycotic Diseases-Candidosis (Candidiasis)
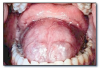
Candidosis (candidiasis) (Figure 43) is caused by overgrowth of candidal organisms due to systemic and/or local factors.
Candidosis can occur in a variety of clinical forms:
- Pseudomembranous (thrush): White plaques which rub off leaving an erythematous base. Pain, burning, and taste alterations are common.
- Acute atrophic (erythematous): Red mucosa accompanied by burning or pain.
- Angular cheilitis: Cracks, crusts, pain in commissure area.
- Chronic atrophic candidosis (Figure 44): Erythematous mucosa confined to denture bearing mucosa. Variably painful.
- Chronic hyperplastic candidosis (Figure 45): White epithelial thickening similar to leukoplakia.
- Median rhomboid glossitis (Figure 46): Erythematous patch anterior to circumvallate papillae.
- Mucocutaneous candidosis: May involve skin and oral, vaginal mucosa and nails. May be familial.
Part III: Soft Tissue Enlargements of Oral Mucosa
Soft tissue enlargements are swellings or masses that are divided into two categories: reactive enlargements and soft tissue tumors.
Reactive Soft Tissue Enlargements
Reactive soft tissue enlargements are caused by injury, such as infections, physical trauma, chemical trauma, or allergic reactions. Reactive soft tissue enlargements usually have a rapid onset (short duration) and may increase and decrease (fluctuate) in size and usually eventually regress. Reactive enlargements are often, but not always, tender or painful and usually have a more rapid growth rate (measured in hours to weeks) than tumors. Sometimes patients with reactive enlargements will be able to report the source of injury. Sometimes reactive lesions are associated with tender lymph nodes and systemic manifestations, such as fever and malaise. Once it is decided that a soft tissue enlargement is reactive, the next step is to determine what the lesion is reacting to, such as bacterial, viral, or fungal infections or chemical or physical injury.
Some examples of reactive soft tissue enlargements:
• Mucocele (salivary extravasation phenomenon)
• Necrotizing sialometaplasia
• Periodontal abscess
• Radicular (periapical) abscess
• Fibrous hyperplasia
• Inflammatory papillary hyperplasia
Salivary extravasation phenomenon, usually called a “mucocele” (Figure 47 and Figure 48) occurs when a salivary gland duct is ruptured and mucus forms a pool in the surrounding connective tissue. It most commonly occurs in locations that are easily traumatized, such as the lower lip. Clinical features include a well localized, compressible or fluctuant soft tissue enlargement. The patient may report that the lesion increases and decreases (fluctuates) in size. The surface of the lesion may be blue to purple or normal in color. Sometimes these lesions resolve spontaneously. Persistent lesions should be excised to minimize recurrence. Lesions must be examined microscopically to exclude salivary gland tumors.
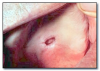
Necrotizing sialometaplasia (Figure 49) is a reactive lesion of salivary gland origin. The cause is local ischemia producing infarction of salivary acini. The ensuing inflammation causes squamous metaplasia of ducts and hyperplasia of the surface stratified squamous epithelium. The vast majority of cases occur on the posterior lateral hard palate. The lesion begins acutely with swelling and pain or numbness. Eventually an ulcer forms within the enlargement. Necrotizing sialometaplasia resembles squamous cell carcinoma and/or mucoepidermoid carcinoma clinically and microscopically. Treatment is incisional biopsy and microscopic diagnosis. No further treatment is necessary once the diagnosis is established, as the lesion resolves spontaneously in weeks to several months.
Periodontal abscess (Figure 50) is an accumulation of pus within a periodontal pocket. It may be associated with pain, tenderness to palpation of the gingiva, tooth mobility, and erythema of the overlying gingiva. Radiographs may reveal loss of alveolar bone. Probing the pocket often allows release of purulent material. Tender lymphadenopathy may accompany a periodontal abscess. Treatment consists of draining the purulent material and debriding the pocket. The presence of fever and malaise indicates a systemic infection, and the patient should be placed on antibiotics. Follow-up periodontal therapy is necessary.
Periapical abscess (Figure 51) is an accumulation of purulent material in the periapical region of a tooth with a necrotic pulp. The involved tooth may or may not be symptomatic. As a periapical abscess becomes larger it can perforate the cortical bone, accumulate in the connective tissue, and form a compressible, painful soft tissue enlargement. Sometimes the purulent material perforates the overlying oral epithelium and forms a channel (sinus track) through which the material may drain into the oral cavity. Parulis (“gumboil”) is the soft tissue enlargement resulting from the accumulation of acute and chronic inflammation and granulation tissue at the opening of the sinus track onto the oral mucosa. Treatment of periapical abscess involves treatment of the involved tooth by root canal therapy or extraction.
Inflammatory papillary hyperplasia (Figure 52) represents an overgrowth of epithelial and fibrous connective tissue, usually as a response to chronic irritation from a denture. The lesion occurs on the hard palate or mandibular alveolar mucosa underneath a denture. The surface of the lesion is bumpy, nodular, or velvety, and often erythematous. The patient may complain of pain or burning in association with the lesion, or the lesion may be asymptomatic. Lesions often have concomitant overgrowth of candidal organisms. The patient should remove the denture as much as possible, and the lesion should be reevaluated. If the papillary overgrowth is minimal, the lesion does not need to be removed. More extensive lesions should be excised. The denture should be remade and the patient educated about removing the denture at night and cleaning the denture. If candidosis is present it should be treated with a topical antifungal ointment or cream applied to the inner surface of the denture.
Soft Tissue Tumors
Soft tissue tumors are characterized by being persistent and progressive; they do not resolve without treatment. They are usually not painful early in their development, and the growth rate varies from weeks to years.
If a soft tissue enlargement appears to be a tumor, the clinician must next determine if the enlargement is benign or malignant. Benign tumors are typically better defined or circumscribed and have a slower growth rate, measured in months and years, than malignant neoplasms.
Malignant neoplasms are more likely to be painful and cause ulceration of the overlying epithelium than benign lesions. Malignant neoplasms are more rapidly growing, with growth rate measured in weeks to months. Since malignant neoplasms have the potential to invade or infiltrate surrounding muscle, nerve, blood vessels, and connective tissue, they are fixed or adherent to surrounding structures during palpation. Some benign tumors are also fixed to surrounding structures, but others are surrounded by a fibrous connective tissue capsule, which may allow them to be moved within the tissue independent of surrounding structures (freely movable). If located in the area of teeth, benign tumors are more likely to move teeth, while malignant lesions loosen teeth. It is important to note that occasionally malignant lesions, especially of salivary gland origin, have clinical features that are deceptively benign.
Benign Epithelial Tumors of Oral Mucosa
Benign tumors of squamous epithelium covered in this course are firm, non-tender, white to tan, and have a rough, cauliflower, or warty surface. They are fixed to the surface mucosa. Papilloma, verruca, and condyloma are warts caused by human papillomavirus.
Papilloma (squamous papilloma)* (Figure 53) is a benign epithelial enlargement that is caused by human papilloma virus infection. It is firm, non-painful, and pedunculated. It has a rough white cauliflower or warty surface with numerous fingerlike processes. It arises from the surface stratified squamous epithelium, is exophytic, and it does not invade underlying tissue. Excisional biopsy including the base of the lesion is the treatment. Recurrence is unlikely.
Verruca vulgaris* is a benign epithelial enlargement of skin and mucosa caused by human papilloma virus. It is asymptomatic, exophytic, and has a broad base. The surface is white, rough, and warty. Verruca may be solitary or multiple. Verrucae may spread to other body surfaces by autoinoculation. Sometimes they resolve spontaneously. Verrucae on the skin are usually treated by liquid nitrogen, chemical agents, or surgical excision. Oral verrucae are treated by excisional biopsy.
Condyloma acuminatum* (Figure 54) is a warty soft tissue enlargement caused by human papilloma virus. It is a sexually transmitted disease and is most common in the anogenital region. It often has multiple lesions. Condyloma is treated by surgical excision. The patient’s sexual partner should also be treated.
Benign Mesenchymal Tumors of Oral Mucosa
For purposes of this discussion, mesenchymal tumors are composed of fibrous connective tissue, smooth muscle, skeletal muscle, blood and lymphatic vessels, adipose tissue, and peripheral nerve tissue. Unless otherwise noted in the following descriptions, benign mesenchymal tumors clinically present as well-circumscribed, persistent, slowly growing, non-tender, soft tissue enlargements.
Irritation fibroma, epulis fissuratum, and peripheral ossifying fibroma represent an overgrowth of fibrous connective tissue.
Irritation fibroma* (Figure 55) is a common reactive soft tissue enlargement due to chronic irritation or trauma. It most commonly presents as an exophytic, dome-shaped enlargement which may be firm or compressible to palpation. The mucosa overlying the lesion may be normal or ulcerated due to trauma. It is most common on the buccal and labial mucosa. Treatment for irritation fibroma is excisional biopsy and microscopic diagnosis. Recurrence is uncommon.
Epulis fissuratum (inflammatory fibrous hyperplasia)* (Figure 56) represents hyperplasia of dense connective tissue due to chronic irritation from the flange of a denture. It appears as an enlargement in the vestibule. Often a fissure will be present in the lesion, corresponding to the location of the denture flange. Treatment consists of surgical excision of the mass and microscopic diagnosis, and usually remaking or relining the denture.
Peripheral ossifying fibroma (peripheral fibroma)* (Figure 57) is a reactive soft tissue enlargement arising from cells of the periodontal ligament. It is always located on the gingiva or attached alveolar mucosa, often ulcerated, and may be red or have a normal mucosal color. It is most common in adolescents through young adults. An interesting feature microscopically is that peripheral ossifying fibroma frequently forms a mineralized product within a cellular fibrous stroma. Treatment is excisional biopsy and microscopic diagnosis. The lesion should be removed down to periosteum. It has a good prognosis although recurrence rates up to 16% have been reported. Treatment for recurrent lesions is re-excision.
Schwannoma* (Figure 58) is a benign neoplasm of Schwann cells. It is firm, encapsulated, and often freely moveable. Treatment is excisional biopsy and microscopic diagnosis. Recurrence is uncommon.
Neurofibroma is also a benign neoplasm of Schwann cells. Neurofibroma most commonly occurs as a solitary lesion, but multiple neurofibromas are a characteristic feature of neurofibromatosis. Solitary neurofibroma is fixed to surrounding structures and may be firm or compressible upon palpation. Treatment consists of excisional biopsy and microscopic diagnosis. Recurrence is not expected.
Traumatic (or amputation) neuroma* represents a reactive proliferation of nerve bundles following severing of a nerve. It arises most commonly in locations containing relatively large peripheral nerves, such as the mental foramen, tongue and lower lip. Neuroma is often, but not always, painful to palpation. Multiple neuromas unassociated with trauma are part of multiple endocrine neoplasia type III syndrome. Treatment consists of excisional biopsy and microscopic diagnosis. Lesions usually do not recur.
Granular cell tumor* (Figure 59) is a benign neoplasm previously called granular cell myoblastoma. The tumor cells are of Schwann cell origin. The lesion is fixed to surrounding structures. The most common location is the dorsum of the tongue. Microscopically, the lesion often appears infiltrative; however, conservative excision and microscopic diagnosis is usually curative.
Rhabdomyoma of the oral mucosa is a rare benign neoplasm of skeletal muscle origin. It is located only where skeletal muscle is found. The most common location is the tongue. It is fixed to surrounding structures. Treatment is excisional biopsy and microscopic diagnosis.
Congenital epulis* (Figure 60) is a benign soft tissue enlargement that occurs on the attached alveolar mucosa of infants. Almost 90% of these lesions occur in females. Treatment is surgical excision and microscopic diagnosis. Prognosis is excellent.
The following benign mesenchymal tumors have clinical features of vascular lesions: peripheral giant cell granuloma, pyogenic granuloma, hemangioma, leiomyoma, and sometimes peripheral ossifying fibroma as discussed above. A vascular soft tissue enlargement is red, blue, or purple and blanches upon pressure.
Peripheral giant cell granuloma* (Figure 61) is a reactive soft tissue enlargement that occurs only on gingiva or attached alveolar mucosa. Treatment is excisional biopsy and microscopic diagnosis. The microscopic features consist of giant cells that are identical to those of central giant cell granuloma.
Pyogenic granuloma* (Figure 62) is a soft tissue enlargement that develops in reaction to minor injury or irritation. It can be found on any oral mucosal surface at any age, but is most common on the gingiva in children and pregnant females. Pyogenic granuloma is compressible, can be lobulated and is often pedunculated. Ulceration is frequently present. The initial growth rate is quite rapid. In lesions of longer duration collagen replaces much of the vascularity and the lesion begins to resemble an irritation fibroma. Treatment is excisional biopsy and microscopic diagnosis. Recurrence is not unusual, and recurrent lesions should be re-excised. For pregnant patients excision can be deferred until after the pregnancy is completed.
Hemangioma* (Figure 63) is a proliferation of blood vessels which usually is noted at birth or early childhood. It may be well circumscribed or diffuse. The arteriovenous malformation is a different lesion. It represents a direct communication between an artery and a vein, and it will demonstrate a thrill and bruit. A hemangioma requires no treatment unless it is a functional or cosmetic problem. Many hemangiomas will regress spontaneously during childhood. Incision of an arteriovenous malformation may lead to fatal hemorrhage.
Leiomyoma is a benign neoplasm of smooth muscle. In the oral cavity it arises from smooth muscle in the wall of blood vessels. It is firm and sometimes has a vascular appearance. Treatment is excisional biopsy and microscopic diagnosis. It does not tend to recur.
Lymphangioma is a developmental overgrowth of lymphatic vessels and not a true neoplasm. In almost all cases lymphangioma is present at birth or appears during the first 2 years of life. The most common locations are the neck and the tongue. Tongue lesions can cause macroglossia, leading to problems with eating and speaking. Tongue lesions are usually compressible and fixed to surrounding structures. The mucosa overlying the lesion often has multiple nodules resembling small vesicles. Lymphangiomas are unlikely to undergo spontaneous regression. Surgical removal of the lesion is difficult if the lesion is poorly circumscribed. The prognosis for most patients is good, but occasionally lymphangioma can cause airway obstruction and be life-threatening.
Benign Salivary Gland Neoplasms of Oral Mucosa
Benign tumors of salivary gland origin are typically encapsulated, slowly growing, and non-tender. The overlying mucosa is normal in appearance unless it has been traumatized. Salivary gland tumors can originate throughout the oral mucosal except for the following locations: midline and anterior hard palate, gingiva, and attached alveolar mucosa. It is important to remember that some malignant salivary gland neoplasms can sometimes be slowly growing, well circumscribed and non-tender, and thus simulate a benign tumor. Tumors that can mimic a benign neoplasm include adenoid cystic carcinoma, polymorphous low-grade adenocarcinoma, low-grade mucoepidermoid carcinoma and acinic cell adenocarcinoma.
Pleomorphic adenoma* (Figure 64), also known as mixed tumor, is the most common tumor of salivary gland origin. The parotid gland is the most common location. The posterior lateral quadrant of the hard palate is the most common location for tumors of minor salivary glands, but it may be found in any mucosal region that contains salivary glands. Pleomorphic adenoma has clinical features similar to many other benign tumors arising from salivary glands and mesenchymal tissue. Complete surgical removal and microscopic diagnosis is the treatment. Very rarely carcinoma arises in a pre-existing pleomorphic adenoma.
Monomorphic adenoma is a generic term that refers to a group of benign salivary gland neoplasms with microscopic features different from pleomorphic adenoma. This term is seldom used currently. Instead, the specific name of the adenoma is used, such as canalicular adenoma, basal cell adenoma, oncocytoma and others. Treatment is excisional biopsy and microscopic diagnosis. Complete excision of the lesion results in cure.
Papillary cystadenoma lymphomatosum, also known as Warthin’s tumor, probably arises from salivary gland tissue trapped within lymph nodes. Almost all cases arise in the parotid gland, and it is more common in older adults. It has been reported to occur bilaterally in 5 to 14% of cases. Surgical removal and microscopic diagnosis is the treatment for papillary cystadenoma lymphomatosum. Some authorities believe that the lesion is often multicentric, accounting for an approximately 10% recurrence (or persistence) rate. The prognosis is good.
Polymorphous low-grade adenocarcinoma* (Figure 65) is a malignant neoplasm of salivary gland origin. It is included in the category of benign salivary neoplasms because it is usually slowly growing, of long duration, and not painful. This tumor occurs almost exclusively in minor salivary glands. Treatment is wide surgical excision. Metastasis to cervical lymph nodes is not common, and distant metastasis is rare. If the lesion recurs it can often be successfully treated by another surgical excision. The prognosis is relatively good, and few cases are fatal.
Acinic cell adenocarcinoma is a malignant salivary gland neoplasm that is most common in the parotid gland. It typically presents as a slowly growing well circumscribed lesion that can be confused with a benign tumor. Occasionally it can be accompanied by pain or paresthesia. Complete surgical excision and microscopic diagnosis is the recommended treatment. Lesions in the major glands may require removal of the entire gland.
Adenoid cystic carcinoma* is an adenocarcinoma of salivary gland origin. It may mimic a benign tumor, but it may also present with pain. The tumor has a tendency to invade nerves. Treatment is complete surgical excision. Adenoid cystic carcinoma is characterized by recurrence and metastasis and has a very poor 20-year survival rate.
Mucoepidermoid carcinoma* (Figure 66) is a carcinoma of salivary gland origin that contains mucous cells and squamous cells. Mucoepidermoid carcinoma has a range of microscopic features that generally correlate with the clinical behavior. Lesions that are composed predominantly of mucous cells (low-grade lesions) are slowly growing, compressible, and relatively less aggressive. Lesions composed predominantly of squamous cells (high-grade lesions) tend to be more rapidly growing, firm, and infiltrative. It should be emphasized that all mucoepidermoid carcinomas are malignant neoplasms and have the potential to recur and metastasize. Treatment is complete surgical excision and microscopic diagnosis. The prognosis depends upon the stage (extent of spread of the tumor) and microscopic grade. Low-grade tumors have a relatively good prognosis, but high-grade tumors have a prognosis similar to squamous cell carcinoma.
Cysts of Oral Mucosa
Cysts of oral mucosa have similar historical and clinical features as benign mesenchymal and salivary gland tumors and are often included in the differential diagnosis of these benign tumors. Cysts are typically well-circumscribed, compressible, non-tender, and slowly growing. The overlying mucosa is normal unless traumatized. Location is often helpful in the differential diagnosis of possible soft tissue cysts.
Epidermoid/dermoid cyst* (Figure 67) is most commonly seen in the skin and oral mucosa. The most common location in the oral cavity is the floor of the mouth. It is “doughy” to palpation. Treatment is surgical removal and microscopic diagnosis.
Gingival cyst* (Figure 68) of the adult is found in the gingiva anterior to the first molars, with a marked predilection for the mandibular canine-premolar region. Simple surgical excision and microscopic diagnosis is the recommended treatment. The prognosis is excellent.
Lymphoepithelial cyst* (Figure 69) develops when epithelium entrapped within oral lymphoid tissue undergoes cystic transformation. The typical lymphoepithelial cyst is a small (less than 1 cm), well-circumscribed, yellow or white, soft tissue nodule located in the floor of the mouth or ventral-lateral surface of the tongue. Treatment for lymphoepithelial cyst is excisional biopsy and microscopic diagnosis. There is little tendency for recurrence.
Thyroglossal tract cyst develops from epithelial remnants of the thyroglossal duct that extends from the foramen cecum to the thyroid gland. Cysts can form anywhere along this tract, but most commonly develop in the neck inferior to the hyoid bone. They are non-painful, movable, and fluctuant. Complete surgical excision which removes the cyst, part of the hyoid bone and portions of surrounding muscle, is the recommended treatment. Recurrence is a possibility.
Malignant Neoplasms of Oral Mucosa
A challenge in differential diagnosis of soft tissue enlargements is the distinction between malignant and reactive lesions. Both can be rapidly growing and painful. The key distinction is that malignant neoplasms are persistent and progressive, while reactive lesions fluctuate in size or eventually regress. Reactive lesions may be associated with soft, tender lymph nodes, while lymph nodes involved with metastatic malignant neoplasms are firm and non-tender.
Squamous cell carcinoma* is the most common malignant neoplasm of the oral cavity. Tobacco and alcohol use have been identified as risk factors, but squamous cell carcinoma can occur in patients with no known risk factors. This tumor can occur anywhere on the oral mucosa, but it is most common on the ventral and lateral surfaces of the tongue, floor of the mouth, soft palate, tonsillar pillar area, and retromolar trigone. Advanced squamous cell carcinoma presents as an indurated (hard) tumor mass fixed to surrounding structures. It is often ulcerated and may be painful. It may be associated with cervical lymphadenopathy representing metastatic lesions. Early squamous cell carcinoma and its precursor lesions are almost invariably asymptomatic, and thus patients do not know they have a lesion. Early lesions may be white rough epithelial thickening lesions (leukoplakia), red persistent non-painful lesions (erythroplakia) or a combination of the two. It is important to discover squamous cell carcinoma in its early stages when cure is possible without disfiguring surgery. The main treatment is complete surgical excision. Lymph node dissection is performed when lymphadenopathy is evident. Radiation therapy is often used as an adjunct to surgery. Chemotherapy is reserved for palliative therapy. Verrucous carcinoma is a slowly growing, low-grade variation of squamous cell carcinoma. The lesion has a rough warty surface and is usually asymptomatic. Verrucous carcinoma can invade underlying tissue but almost never metastasizes. It has a good prognosis compared to typical oral squamous cell carcinoma.
Salivary gland adenocarcinoma (Figure 70) includes polymorphous low-grade adenocarcinoma, adenoid cystic carcinoma, acinic cell adenocarcinoma, mucoepidermoid carcinoma, carcinoma arising in pleomorphic adenoma, and a number of other lesions. These lesions may grow rapidly or slowly and present with pain and paresthesia or be asymptomatic. They all demonstrate infiltrative growth. Treatment is generally complete surgical excision. Prognosis depends upon the stage or extent of the tumor and its microscopic features.
Lymphomas* (Figure 71) are a diverse group of malignant neoplasms of lymphocytes and their precursors. They form solid tumor masses and usually arise within lymphoid tissue. Lymphomas are subdivided into Hodgkin’s disease and non-Hodgkin’s lymphomas. The most common presentation of Hodgkin’s disease in the head and neck area is persistent, progressive enlargement of cervical and supraclavicular lymph nodes. Hodgkin’s disease only rarely has intraoral lesions. Non-Hodgkin’s lymphomas include numerous different lesions that may arise in lymph nodes or in extranodal sites. Lesions arising in lymph nodes are non-tender, slowly enlarging masses that eventually become multiple fixed enlargements. Extranodal lymphoma in the oral cavity may be the first manifestation of lymphoma or may be part of a disseminated process. Extranodal oral lymphoma of soft tissue is typically a non-tender, poorly circumscribed, compressible, soft tissue enlargement, sometimes with erythema and ulceration of the overlying mucosa. The most common sites are Waldeyer’s ring, posterior hard palate, buccal mucosa, or gingiva. Lesions may also arise within the jaws. Jaw lesions have clinical features similar to other malignancies of bone. Malaise, fever, and weight loss may accompany both Hodgkin’s disease and non-Hodgkin’s lymphoma. The management of lymphoma involves biopsy of the lesion to obtain a definitive diagnosis. This is followed by staging to determine the extent of the disease. Chemotherapy and/or radiation therapy are used for treatment. The prognosis is extremely variable.
Carcinomas metastatic to oral soft tissue: Metastatic neoplasms to the oral cavity make up only 1% of all oral cancers, and these tumors are found much more frequently in the bone of the jaws than in the oral soft tissues. The vast majority of tumors that metastasize to the oral cavity are adenocarcinomas. The most common primary locations of these tumors include breast, lung, kidney, gastrointestinal tract (stomach and colon), thyroid and prostate.
The most common oral mucosal locations for metastatic carcinoma are the gingiva and tongue. Early lesions are dome-shaped nodules with a smooth, normal-appearing surface. These lesions may appear benign clinically. Later, the surface may become ulcerated and necrotic, and the lesion may bleed easily. These lesions appear malignant clinically.
Sarcomas are relatively rare malignant neoplasms of non-epithelial tissue. Sarcomas may arise in soft tissue or bone. Examples include fibrosarcoma, rhabdomyosarcoma (skeletal muscle origin), and leiomyosarcoma (smooth muscle origin). Sarcomas generally are rapidly growing, poorly circumscribed, infiltrative, and cause ulceration of the overlying tissue. Treatment is usually surgical removal combined with chemotherapy and/or radiation therapy. The prognosis depends upon the stage of the disease and microscopic features.
Melanomas are relatively rare in the oral cavity. They are discussed in the section on localized pigmented surface lesions.
Part IV: Summary of Clinical Features of Oral Mucosal Lesions
The Summary of Clinical Features of Oral Mucosal Lesions are presented in the following tables:
• Table 1. White Surface Lesions of Oral Mucosa
• Table 2. Localized Pigmented Surface Lesions of Oral Mucosa
• Table 3. Vesicular-Ulcerated-Erythematous Surface Lesions of Oral Mucosa
• Table 4. Soft Tissue Enlargements
• Table 5. Benign Epithelial Tumors
• Table 6. Benign Mesenchymal Tumors
• Table 7. Benign Salivary Gland Tumors
• Table 8. Soft Tissue Cysts
Conclusion
Successful management of patients with lesions of oral mucosa can be accomplished by dental health care providers if a step-by-step approach is used to gather information and apply it in a systematic manner to diagnostic decision trees. This course provides general guidelines that can be used to eliminate or exclude most oral lesions from the clinical differential diagnosis. Those lesions that cannot be excluded constitute the clinical differential diagnosis. The value of formulating a clinical differential diagnosis for an oral lesion is that it eliminates guessing at the best diagnosis and thus guides the next steps in managing the patient’s lesion. Determining the definitive or final diagnosis of an oral lesion often requires additional testing, such as obtaining a biopsy specimen and having it microscopically diagnosed.
References
1. Darling MR, Daley TD. Blistering mucocutenous diseases of the oral mucosa - A review: Part 1. Mucous membrane pemphigoid. J Can Dent Assoc 2005; 71:851-4.
2. Darling MR, Daley TD. Blistering mucocutenous diseases of the oral mucosa - A review: Part 2. Pemphigus vulgaris. J Can Dent Assoc 2006; 72:63-6.
3. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology, 3rd ed. W.B. Saunders Co., Philadelphia, 2009.
4. Neville BW, Damm DD, White DK. Color Atlas of Clinical Oral Pathology, 2nd ed. Lippincott Williams & Wilkins Co., Philadelphia, 1999.
5. Regezi JA, Sciubba JJ, Jordon RCK. Oral Pathology: Clinical Pathologic Correlations, 4th ed. Saunders Co., Philadelphia, 2003.
6. Sapp JP, Eversole LR, Wysocki GP. Contemporary Oral and Maxillofacial Pathology, 2nd ed. Mosby, 2003.
7. Scully C, Felix DH. Oral Medicine – Update for the dental practitioner. Oral white patches. British Dental Journal 2005; 199:565-72.
8. Vincent SD, Lilly GE. Clinical, historic, and therapeutic features of aphthous stomatitis. Literature review and open clinical trial employing steroids. Oral Surg Oral Med Oral Pathol 1992;74:79-86.
9. Vincent SD, Lilly GE, Baker KA. Clinical, historic, and therapeutic features of cicatricial pemphigoid. A literature review and open therapeutic trial with corticosteroids. Oral Surg Oral Med Oral Pathol 1993;76:453-9.
10. Woo S, Sonis ST. Recurrent apthous ulcers: A review of diagnosis and treatment. JADA 1996; 127:1202-13.
Electronic Resources
Oral Pathology Image Database: http://guides.lib.uiowa.edu/c.php?g=131885&p=864394
Disclaimer: Participants must always be aware of the hazards of using limited knowledge in integrating new techniques or procedures into their practice. Only sound evidence-based dentistry should be used in patient therapy.