You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Preparation design should be the primary factor for cement choice when seating any type of ceramic restoration. Too often, clinicians use the ceramic type as the first consideration for the type of cement to use, and preparation design becomes the last factor contemplated (Figure 1). When preparation design dictates the decision pattern (Figure 2), cement selection is more definitive and clear, leading to the ultimate step of how to prepare the ceramic for the proper cement chosen.
With non-retentive preparations, a limited number of cement options are suitable, whereas a retentive preparation offers a broader selection. In addition, non-retentive preparations require further decisions about which adhesive and primer will be most effective with the selected cement and ceramic.
A retentive preparation bases the long-term retention and stability of the restoration primarily on the form of the tooth preparation itself, thereby expanding the clinical cementation options to virtually all cements available. These include self-adhesive resin cements, resin-modified glass ionomer cements, and bioceramic cements. However, the stability and long-term retention of a ceramic on a non-retentive preparation is based on the adhesive bond between the restoration and the preparation. Therefore, resin cements are required for ensuring predictability. Clarifying the parameters behind which cement and protocols should be used is essential to achieve the most esthetic, predictable long-term restoration.
ZIRCONIA CEMENTATION OF RETENTIVE PREPARATIONS
When the preparation is providing most of the retention, the sole focus can be on the luting agent. Ceramic primers can still be used but are not essential to the success of the restoration. Yet, if resin cement is the luting agent of choice, the proper ceramic primer should always be incorporated into the ceramic preparation before cementation. For retentive preparations, three basic types of cements are good options: self-adhesive resin cements, resin-modified glass ionomer cements, and bioceramic cements.
CAPABILITIES OF BIOCERAMIC CEMENTS
Bioceramic cements offer a number of distinct advantages over other cements. Because of their unique chemistry and high amount of calcium aluminate, these cements form apatite crystals where any phosphates are present, ranging from the phospholipids found in saliva, to tooth structure, to the phosphates on the ceramic itself.1 These characteristics allow the formation of new hydroxyapatite layers between the ceramic and the tooth structure, with the potential to seal cement gaps that are inevitably a part of every cementation procedure, no matter how microscopic.
A recent study explored the potential of cements to seal marginal gaps between the tooth structure and the restoration by using test material to create artificial gaps.2 Calcium silicate, which has been shown to repair damage in tooth structures (also known as MTA), demonstrated the ability to repair the margin in this study, after 13 days and 30 days. With calcium aluminate, after 4 days, artificial gap repair was evident, and by 48 days, no evidence of a gap was visible (Figure 3).
The other test materials studied (self-adhesive resin cement, glass ionomer, and resin-modified glass ionomer) showed no evidence of marginal gap closure. Even at 8 months follow-up, the glass ionomer and the resin-modified glass ionomer cements continued to show the artificial gap.
The study investigators concluded that there was no evidence of marginal gap closure for the three conventional cements. Researchers did not find this surprising, as the properties of these cements include nothing that would facilitate closure. With the bioactive properties in calcium silicates and calcium aluminates, active closure of the artificial gap was evident. These bioactive surface apatite-forming cements appeared to seal or re-seal the artificial marginal gaps, suggesting a new functional property for bioactive dental materials. This ability to improve marginal stability significantly and predictably could enhance the survival and serviceability of dental restorations, researchers suggested.
Bioceramic cements are also beneficial for patients with oral hygiene challenges, as the properties of these cements may help prevent recurrent decay. With a pH of approximately 8.5, this material is basic. Basic cements are ideal in the oral environment as they counteract acidic attacks so prevalent in the oral cavity.
CASE STUDY
A male patient presented with an unrestored endodontically treated tooth. Because of the retentive qualities of this preparation, a bioceramic cement was considered. When the temporary was removed, there was inflammation in the tissue surrounding the distal margin. In addition, this patient showed significant plaque issues (Figure 4 and Figure 5). This is a difficult situation we all face in dentistry. Any type of resin cement would be prone to long-term failure due to the high likelihood of bacterial contamination, as well as moisture contamination, that could undermine the quality of the bond.
A cement that can seat predictably in a moist environment and self-seal against bacterial contamination allows the clinician to be more confident in the cementation of this ceramic. Another chairside advantage is easy cleanup (Figure 6). With resincements, often the material hardens so quickly with a tack-cure that ensuring proper cleaning and removal of all the cement proves difficult.
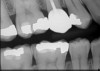
Figure 7 shows the final zirconia crown post cementation. A postcementation radiograph (Figure 8) is essential to ensure that no cement is retained interproximally and to verify accurate margin seating.
CEMENTATION PROTOCOL
Bioceramic cements require no preparation on the tooth surface or on the intaglio of the crown. To clean the restoration after try in, the operator may simply rinse and air dry, or sandblast the intaglio. Sandblasting will not change the morphologic structure of the zirconia restoration, but does serve as an effective method to thoroughly clean the restoration. While glass ceramics can be predictably cleaned with phosphoric acid etchants, zirconia restorations should never be cleaned with phosphoric acid etch. Zirconia restorations have an affinity for phosphate groups, so all of their potential phosphate adhering sites would be occupied by the phosphate groups used in the etchant, greatly reducing the bond strengths of any cement to the zirconia restoration.
Once the zirconia restoration has been properly cleaned, the bioceramic cement is placed into the crown and the restoration seated. Constant pressure should be applied for 4 minutes to allow complete set of the material. At two minutes, the bioceramic cement becomes pliable and initial removal at the margins can be done, but pressure should continue to be applied until the 4-minute set time. This rule should be applied to all cementation procedures of any type of cement to allow for complete polymerization of the material before any occlusal adjustments are made where the vibrations can alter the final set of the cement.
Bioceramic cements are opaque and may not be an ideal choice for a thin restoration where esthetics are crucial. A more translucent and esthetic resin cement may be better suited in these cases. In cases over 1.5 mm in thickness, there should be no show-through with bioceramic cement; in cases approximately 1 mm or less, show-through is likely.
Despite having similar bond strengths to glass ionomer cements and bonding well to the dentine and other substrates,3 bioceramic cements should not be used with a non-retentive preparation, as it could result in crowns dislodging. Bond strengths of bioceramic cements, self-adhesive resin cements, and glass ionomer cements are all consistently low and are only suitable for retentive preparations. Resin cements when used properly are routinely three times as strong as these cements.4,5
SELF-ADHESIVE RESIN CEMENT
Advantages of self-adhesive resin cements include ease-of-use and bonding capability. In addition, in situations where the full bonding process is not needed but esthetics are particularly important (such as in a premolar, a canine, or a single lateral), self-adhesive resin cement is preferred.
Using a self-adhesive resin cement becomes difficult when working in the posterior, due to isolation issues. Traditionally, a disadvantage of self-adhesive resin cement is the tack-cure hard-ness setting time, making it difficult to use and remove from unwanted areas applied in error. For this reason, products are being introduced with a longer gel phase and a wider tack-cure window.
Evidence indicates that self-adhesive resin cements are not suitable for non-retentive preparation. A 2009 study compared self-adhesive resin cements versus complete adhesive resin cement and found that the bond strength of conventional multistep systems was much better than that of self-adhesive agents.4
RESIN-MODIFIED GLASS IONOMER
Resin-modified glass ionomer cements are often less expensive than other cements and have a long history of use in dentistry, with effective marginal seal in difficult isolation areas. One of the benefits of using resin-modified glass ionomers is fluoride release. However, the effectiveness of the fluoride release long-term remains questionable. Disadvantages of using resin-modified glass ionomers are that they expand, are acidic, and have low bond strength.
ZIRCONIA CEMENTATION OF NON-RETENTIVE PREPARATIONS
When proper ferrule and resistance-retention form are not present with the tooth preparation, several steps are required for predictable cementation of a zirconia restoration. As indicated previously, the clinician must take into account the bonding surface of both the ceramic and the tooth (including primers and bonding agents) as well as the type of cement to be used, whereas when an appropriate rententive preparation exists, only the cement alone is considered (Figure 9). With resin cements, it is advantageous to use adhesive and cement from the same manufacturer, as they have been formulated and tested to work together.
When priming the ceramic restorations, con-sider the substrate type. Two main categories exist: glass-based ceramics (eg, lithium disilicate, feldspathic porcelain, leucite reinforced) and zirconia- or metal-based (eg, zirconia, alumina, noble metals) ceramics. Both types require use of a primer, but they have different needs. Glass-based ceramics are etchable by hydrofluoric acid, while zirconia/metal-based restorations are not. Silane can be used for glass-based ceramics, but a zirconia/metal-specific primer must be used for zirconia/metal-based restorations.
Priming zirconia- and metal-based ceramics differs from that of glass-based ceramics because it is not possible to micromechanically etch zirconia. Instead, the bonding action is strictly chemical. The polycrystalline structure of zirconia- and metal-based ceramics is impervious to hydrofluoric acid-etching. Although some manufacturers recommend sandblasting zirconia-based ceramics, research has also found this approach to be ineffective at changing zirconia’s morphologic microstructure.6 Nonetheless, use of appropriate primers can improve the bond strength of such ceramics. For zirconia, the use of a phosphonic acid monomer or a phosphate ester monomer has been found to improve the bonding of resin to zirconia ceramic.7 Another study in 2011 confirmed that silane treatment had no positive impact on bond strength of polished zirconia. But after applying a phosphate/carboxylate-based primer to the zirconia restoration, bond strength doubled.8
As stated previously, zirconia has a high affinity for phosphate groups. As a consequence, the phospholipids in saliva can easily contaminate zirconia surfaces. Indeed, when zirconia was first introduced, manufacturers were recommending cementation with certain self-adhesive resin cements, but the crowns tended to quickly debond. After try-in, zirconia crowns would be coated by the phospholipids in saliva that would occupy all the phosphate spots needed for the resin cement; hence, debonding would occur. To avoid this, it is important to use a cleaning paste product rather than a phosphoric acid-etch that will further contaminate the surface. The author prefers using a concentrated form of liquid zirconia that removes phospholipids from the zirconia surface. Zirconia primer can then be applied and allowed to set for 30 seconds before the final step of resin cement application. As with glass-based ceramics, the primer develops a chemical bond to both the zirconia and the cement.
After appropriate bonding of the tooth, either a light-cure resin or a universal resin is an acceptable cement choice to permanently seat the zirconia restoration.
CONCLUSION
Clarifying the parameters behind which cement and protocols should be used is essential to achieve the most esthetic, predictable long-term indirect restoration with no recurrent decay. In deciding which cement to use, clinicians should categorize their options based upon the preparation style first and foremost, followed by cement type and then the ceramic. For retentive preparations, cement choice is broad. Bioceramic cements offer several advantages for retentive zirconia restorations. For non-retentive preparations, resin cements should be used in conjunction with a primer that is specific for zirconia restorations.
REFERENCES
1. Pameijer CH. Ceramir™ Crown & Bridge luting agent—a treatise on biocompatibility. August 2009. http:// ceramir.se/BinaryLoader.axd?OwnerID=34f41d5a-9511- 49fd-908a-2d973293c9b7&OwnerType=0&PropertyN ame=relatedArticles&FileName=Ceramir+C%26B- +A+treatise+on++biocompatibility-.pdf&Attachment=True. Accessed April 5, 2017.
2. Jefferies SR, Fuller AE, Boston DW. Preliminary evidence that bioactive cements occlude artificial marginal gaps. J Esthet Restor Dent. 2015;27(3):155-166.
3. Jefferies SR, Lööf J, Pameijer CH, et al. Physical properties of XeraCem. J Dent Res. 2008;87(B):3100.
4. Viotti RG, Kasaz A, Pena CE, et al. Microtensile bond strength of new self-adhesive luting agents and conventional multistep systems. J Prosthet Dent. 2009;102(5):306-312.
5. Nagai T, Kawamoto Y, Kakehashi Y, et al. Adhesive bond-ing of a lithium disilicate ceramic material with resin-based luting agents. J Oral Rehabil. 2005;32(8):598-605.
6. Borges GA, Sophr AM, de Goes MF, et al. Effect of etching and airborne particle abrasion on the microstructure of dif-ferent dental ceramics. J Prosthet Dent. 2003;89(5):479-488.
7. Kitayama S, Nikaido T, Takahashi R, et al. Effect of primer treatment on bonding of resin cements to zirconia ceramic. Dent Mater. 2010;26(5):426-432.
8. Chen L, Suh BI, Kim J, et al. Evaluation of silica-coating techniques for zirconia bonding. Am J Dent. 2011; 24(2):79-84.
Disclosure
Dr. Gillespie has received an honorarium for his work on this article.
About the Author
Gregory Gillespie, DDS
Private Practice, Vancouver, Washington