You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
With advances in imaging technologies and changing recommendations for radiographic protocols, dental practices should review the variables that may entail modifications to their protocols. Setting appropriate imaging protocols in a dental practice, based on the clinician’s preferred diagnostic procedures, can impact all aspects of a practice, by building patient relationships and utilizing technology that can improve the practice workflow and productivity. With the advent of nonionizing radiation (NIR) transillumination technology, dental professionals have another diagnostic tool that may be better suited for certain clinical situations.
In 2012, the American Dental Association (ADA) issued recommendations for dental radiographic examinations, focusing on an individualized approach. The ADA recommends that, before prescribing X-rays, dentists first conduct a clinical exam, taking into consideration individual factors such as age, medical history, caries risk, periodontal status, overall physical health, home care, vulnerability to environmental factors, and signs and symptoms.1 Every patient is unique, with her or his own dental conditions and challenges, which should be recognized before any imaging protocol is determined. This diagnostic and evaluative information may determine the type of imaging used and the frequency. Using a cookie-cutter approach in which all patients receive standard X-rays every year is no longer recommended.
Despite advances in other technologies, radiographs remain the most used imaging modality. However, in many instances, patients or parents of patients will refuse dental X-rays. Patients who have compromised health, pregnant women, parents who do not want their children exposed to radiation, or patients who wish to avoid all radiation exposure may request other options. Offering alternative comprehensive imaging, such as one that utilizes transillumination technology and produces no cumulative ionizing radiation, is safe and effective, and can be used as often as necessary.
Adjusting Imaging Protocols
Dental practices should develop their own protocols for determining type and frequency of imaging modalities. Certain patient subsets would benefit from the use of diagnostic options not limited to visual exams and X-rays. In order to provide the most thorough exam for certain patients, dentists should utilize non-ionizing radiation (NIR) transillumination technology in conjunction with visual exams and bitewing X-rays. Under the ADA radiographic protocols, NIR caries detection technology can be integrated into a practice for the benefit of middle-aged, geriatric, and young patients.
How might this technology affect imaging protocol? These patients illustrate how adjustments could be made in imaging for their benefit:
Middle-aged patients. For example, a middle-aged patient who had a high caries rate when younger (leading to numerous restorations), but who currently exhibits good oral hygiene and maintains regular recall appointments, would require a specific imaging protocol based on the clinician’s judgment. The ADA states that these patients should receive bitewings to determine caries and periodontal status, along with panoramic and selected periapical images, caries detection for recurrent caries and cracks, and intraoral camera images for any failing restoration, especially in the posterior regions. A full-mouth intraoral radiographic exam is preferred when the patient has clinical evidence or a history of extensive dental treatment.1 With integrated NIR technology, a dental office could adjust this protocol by offering detection for occlusal, interproximal, and recurrent caries at every visit, along with the use of intraoral camera images for failing restorations. Although a failing restoration may be evident visually, newer devices allow it to be captured and shown to patients. Even if the clinician is not diagnosing with intraoral camera images, these photographs and videos are beneficial for education and documentation.
Geriatric patients. With a geriatric patient, there may be a higher incidence of root caries, receding gums, and dry mouth. While the patient may maintain fair oral hygiene, those with arthritis could have difficulty flossing and brushing. These patients typically have regular recall appointments. A high caries rate when younger may have resulted in many restorations. ADA protocol recommends taking bitewings or panoramic images every 12 to 36 months, as well as a full-mouth intraoral radiographic exam when there is evidence of generalized oral disease or a history of extensive dental treatment.1 This protocol could be adapted by using caries detection devices for recurrent caries and cracks, and intraoral camera images for failing restorations and new cervical root caries.
Young adults with transitional dentition/ adolescents with permanent dentition. These patients may exhibit moderate-to-high caries rate, along with frequently postponed recall appointments and only fair oral hygiene. These patients should receive bitewing radiographs at 12-month intervals, caries detection imaging at each visit for detection of occlusal and interproximal caries, caries detection for recurrent caries, and intraoral camera images for areas of plaque buildup. Where indicated, selected periapical images and a panoramic exam may also be necessary.1 Adding fluorescence or NIR caries detection can aid in caries detection at all visits.
Younger patients. Prior to the eruption of the first permanent tooth or when there is mixed dentition, there is low caries risk. Recommended imaging protocol for this population includes bitewings every 2 years or less, as well as a panoramic image to review growth and development, although offices could consider doing these less frequently if caries detection technology is available.1 Detection for occlusal and interproximal caries, as well as caries around sealants, can be integrated into imaging protocol, which will reveal pits and fissures, and decay that might not be visible on bitewings.
Dental practices have admitted success changing their imaging protocols to include caries detection devices. It is possible that over time, changing imaging protocol to use NIR transillumination technology on patients under 20 years old, unless they have a high incidence of caries, could become standard. Because of the accuracy and relative comfort of this system, it is a preventive service that improves the patient experience.
Technology in Practice
Nonionizing radiation (NIR) transillumination technology supports identification of occlusal, interproximal, and recurrent carious lesions and cracks, and is considered a safe diagnostic tool because it does not use ionizing cumulative radiation. This technology is often available in a compact and portable device, making it easy to utilize in clinical practice.
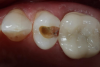
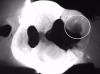
Transillumination technology bathes the tooth in safe, near-infrared light, which makes the enamel appear transparent. This allows clinicians to see through the tooth, exposing its structure and allowing for highly accurate detection of the structure of any carious lesions. In porous tissue such as lesions, the light is trapped and absorbed. Images using transillumination technology are similar to X-rays, with lesions appearing as dark areas and healthy tooth structure as light areas (Figure 1). Therefore, this familiarity facilitates interpretation. In addition, NIR results are not affected by the presence of bacteria, and calibration is not required, as it is with other devices.2
As another safe diagnostic tool, fluorescence technology can be used as an imager or scanner, each with its own capabilities. The imager bathes teeth and tissue in a blue light that highlights abnormalities (Figure 2), while the scanner aims a yellow-red light directly onto areas of interest. These devices can be used to detect bacteria, plaque, enamel, and dentin through fluorescence stimulation. Imagers utilize a range of colors or numbers to indicate the range of conditions (Figure 3), whereas scanners display a number correlated to the degree of demineralization. Fluorescence devices are indicated for occlusal caries; however, they are not indicated for interproximal caries or for use around restorations, nor do they detect fractures.3,4
Although bitewing radiography has been used for many years, research has shown that even digital bitewing images have a lower sensitivity for diagnosing caries and therefore are not the most effective modality in certain cases.5 In addition, bitewing images are often imperfect. Diagnosing interproximal carious lesions using this technology is difficult due to variations in tooth shape and alignment, patient anatomy and cooperation, and levels of operator expertise.6 It is difficult to detect interproximal caries on radiographs unless they are larger than 2 mm to 3 mm deep into the dentin or one-third the buccolingual distance.7 For example, when there is an overlapping area in a bitewing, clinicians must determine whether to attempt to retake the bitewing (exposing the patient to additional radiation) or shift to another technology.
A recent study found that visual inspection can detect approximately 2% of interproximal caries, whereas bitewing radiography may be able to detect 96%. However, that same study found that the use of NIR transillumination technology resulted in 99% detection.8 This research may help change treatment considerations in clinical practice.
Figure 4 through Figure 11 compare various imaging modalities in three different cases, illustrating the potential of these devices to improve diagnostic capabilities.
Integrating Technology to Advance the Practice
Expanding imaging capabilities provides an opportunity for the dental team to put those images to work in all aspects of the practice. In addition to improving examinations and diagnostics, producing oral images utilizing this technology provides staff members the opportunity to discuss treatment options with the patient and answer questions related to care, improving the patient experience. This visual resource can also aid in improving treatment acceptance. Data show a 5% improvement in case acceptance when dentists use intraoral images to help illustrate the oral health concerns being discussed.9
Another factor in improved practice production is a new procedure Current Dental Terminology (CDT) code issued by the ADA. The code D0600 (which is a procedure code, not an image code) is for fluorescence and non-ionizing diagnostic procedure capable of quantifying, monitoring, and recording changes in structure of enamel, dentin, and cementum.10 Until insurance carriers become more familiar with the new code, however, issues may arise when submitting claims, so a narrative is suggested.
Finally, establishing a workflow for different situations allows the team to utilize appointments efficiently, making time for other types of caries or oral cancer detection. A successful workflow entails knowing the patient and where he or she fits in the office’s imaging protocol.
In addition, recognizing an appropriate time during the appointment to use that technology is key. Allot the appropriate amount of time to provide patient education using these images, while standardizing the messaging used for educational scenarios. If the technology is not being used to full capacity, the team can aid in determining why: is it a factor of training, time, accessibility, or routine?
Conclusion
How might this technology affect imaging protocol? The ADA states that the radiographic guidelines are “subject to clinical judgment, after reviewing the patient’s health history and completing a clinical examination.”1 In addition, practitioners should remain informed on advances in equipment and techniques that could further improve their diagnostic abilities.
Certainly, patients and practices would benefit from the use of diagnostic options as they become available. To provide the most thorough exam, dental practices should develop their own protocols for determining type and frequency of imaging modalities, and for integrating these advances into their workflow. It is time for an individual approach not only in radiographs, but for other forms of diagnostics.
References
1. U.S. Department of Health and Human Services Public Health and American Dental Association. Dental radiographic examinations: recommendations for patient selection and limiting radiation exposure. Revised 2012.
2. DEXIS website. CariVu – Caries detection device. http:// www.dexis.com/carivu. Accessed September 30, 2016.
3. KaVo Dental website. DIAGNOdent Caries Detection Aids. http://www.kavo.com/us/caries-detection. Accessed September 30, 2016.
4. AirTechniques. CamXElara/CamXSpectrainstallationandoperating instructions. http://www.airtechniques.com/wp-content/uploads/CamXElaraAndSpectraInstallationAndOperatinManual. pdf. Accessed September 30, 2016.
5. Sochtig F, Hickel R, Kuhnisch J. Caries detection and diagnostics with near-infrared light transillumination: clinical experiences. Quintessence Int. 2014;45(6):531-538.
6. Dykstra BA. Interproximal caries detection: how good are we? Dentistry Today. April 1, 2008.
7. Rock WP, Kidd EA. The electronic detection of demineralisation in occlusal fissures. Br Dent J. 1988;164(8):243-247.
8. Kuhnisch J. Benefits of the DIAGNOcam procedure for the detection and diagnosis of caries [study project]. Munich: Ludwig Maximilian University; 2013.
9. Practice Analytics. Dental practice productivity: how does your practice measure up? http://practiceanalytics.com/ wp-content/uploads/Practice-Analytics-Dental-Practice- Productivity-Whitepaper.pdf. Accessed July 5, 2017.
10. American Dental Association. Committee adds 11 new codes to CDT. ADA News. March 15, 2016.
About the Author
Jan Myskowski, RDH: Temple University graduate with degrees in Dental Hygiene and Public Health. Worked In private practice and in the dental forensic field. Has held corporate positions including Certified Instructor, Manager of Training, Customer Advocate, Training and Operations Leader for KaVo Kerr. Currently serving as KaVo Kerr’s Clinical Program Manager. Was selected as one of Dental Product Reports’ Top 25 Women in Dentistry in 2016