You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
In 2011, the United States Census Bureau on Child Care Arrangements reported that 12.5 million (61%), of the 20.4 million US children under age 5, were in some type of regular child care arrangement over the course of a typical week.1 Findings also indicate that this age group spent most of their time with a child care provider when not with their parents.1,2 Dental injuries among preschool-age children has been reported with a prevalence as high as 30%; generally occurring as a result of falls.3 Eighty percent of these injuries occur in the home and are particularly due to poor muscle coordination between the ages of 12 to 24 months.3-12 Risk of dental trauma peaks at age four due to increased physical activity, with twice the average incidence within this age group as compared to all other age groups.3,5,10 In the instance of dental injury, first aid measures include: compressing the injured area with cotton or gauze for five minutes to stop bleeding, use of a cold cloth or ice pack to reduce swelling and seeking emergency treatment from a pediatric dentist.13,14
Existing research shows first aid provided by parents and teachers following dental injury is inadequate.15-17 Previous studies investigating parent/teacher knowledge, attitudes, and management regarding dental injuries have had a number of limitations including underpowered sample sizes comprised of convenience samples, low response rates, and selection bias. There is currently little information in the literature regarding child care provider knowledge, attitudes, and management of dental injuries in preschool-age children. Given the high likelihood of being the first responders to preschool-age dental injuries, it is important that child care providers understand the significance of prompt first aid measures.
The purpose of this study was to assess child care providers’ level of knowledge, attitudes, and first aid management of dental injury among preschool-age children.
Materials and Methods
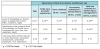
This descriptive, cross-sectional study design used a non-probability, convenience sample of twenty child care centers in Fairfield County, Connecticut and in Boston, Massachusetts. The questionnaire was developed by modifying previous research survey instruments.16-19 The questionnaire was composed of 4 sections; Section I: demographics including gender, age, race, employment status, years of experience as a child care provider, level of education, and number of children for the respondent; Section II: multiple choice questions on level of dental injury knowledge, experiences with dental injuries, and first aid training; Section III: five-point Likert response questions scaled from “strongly agree” to “strongly disagree” on attitudes towards dental injuries; Section IV: multiple-choice questions regarding dental injury first aid and 2 case study questions with images (See Table 1). Case studies were developed based on American Academy of Pediatric Dentistry Dental Trauma Guidelines.20
During the development of the survey questionnaire, content validity index (CVI) was assessed by a panel of 5 dental experts.21 Three of the dental experts were authors of related research and were initially contacted in the development phase of the questionnaire.16-18 The two other dental experts were specialists in pediatrics. Individual question relevance (I-CVI) as well as the overall content of the questionnaire (S-CVI) were quantitatively assessed by the expert panel. Items with an I-CVI of 0.78 or higher for 3 or more experts are considered evidence of good content validity; S-CVI of 0.90 or higher is considered acceptable.21 For the present study I-CVI question scores ranged from 0.8-1. The S-CVI for the survey was 0.95. The questionnaire was then pilot tested with a group of 6 child care providers at a child care center that met inclusion criteria, for comprehension and feedback only. The Massachusetts College of Pharmacy and Health Sciences (MCPHS) University Institutional Review Board oversaw the protection of all human subjects in this research study.
Forty child care centers in Connecticut and Massachusetts were solicited for study participation with 20 centers agreeing to participate. Directors of the centers were contacted and given a flyer providing information about the study including an electronic link to the survey instrument via Survey Monkey®. Directors were asked to disseminate the survey link to the child care providers in the facility. The principal investigator was blinded to the number of child care providers within the centers solicited for study participation by the center directors. Therefore, a response rate could not be accurately enumerated.
The statistical analysis included descriptive statistics using frequency percentiles. Non-parametric Spearman Rank Correlation tests were performed to test for statistical associations between independent and dependent variables.22 Independent variables were age, years of experience as a child care provider, if the child care provider had children of their own, prior experience with dental injuries and history of first aid training with or without dental injury first aid. Dependent variables were level of knowledge regarding dental injury, attitudes regarding dental injury, and first aid management knowledge following dental injury. An alpha threshold of 0.05 was set for all statistical testing. All statistical analyses were performed in STATA® statistics/data analysis software, version 11.2.
Results
A total of 100 child care providers completed the web-based questionnaire. Age categories of study respondents were as follows:19-29, 30-39, 40-49, 50-59 and >60 years old. Figure 1 and Figure 2 show descriptive statistics of participant knowledge and attitudes about dental injury, respectively. Of the respondents, 84% self-reported little to no knowledge about dental injury management, suggesting lack of education and training on the subject. Similarly, 78% of child care providers reported very low to low satisfaction with their personal level of knowledge about dental injury management. Nearly two-thirds of child care providers reported not feeling adequately informed about dental injuries, with 77% expressing interest in receiving more information. Of the respondents, 60% agreed that child care providers are responsible for managing dental injuries. However, when asked to respond to the question, “Due to some legal concerns, it is recommended that child care providers avoid getting involved in the event of a dental injury,” 43% of respondents were undecided whether they agreed or disagreed.
Table 1 shows the two case study questions asked of the participants. In case I, a 14-month-old girl falls from her high chair causing her front tooth to dislocate and appear pushed back towards the palate, 61% of child care providers chose the appropriate action which included bringing the child to the dentist immediately. When asked about their advice upon the arrival of the child’s parents following the event of a traumatic dental injury, 87% recommended referring the parents and child to their dentist. In case II, regarding the 5-year-old boy knocking his front tooth and fracturing it on the slide, 57% gave the correct response on how to manage the injury. When asked about replanting a primary tooth, 76% chose the correct response not to replant. Two-thirds of the child care providers were aware that immediate emergency action was needed for the treatment of traumatic dental injuries.
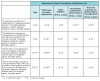
Table 2 and Table 3 show the results of Spearman Rank Correlation Tests between select demographic variables and dental injury knowledge and management questions, respectively. Self-reported level of knowledge on dental injury management was found to have a statistically significant direct correlation with increasing age (p<0.05), increasing child care provider experience (p<0.01), having children of their own (p<0.05), witnessing a dental injury (p<0.05), and having training on dental injury management (p<0.01). These predictors suggest age, training and personal experiences with dental injuries prepare child care providers for dealing with dental injury events.
Level of satisfaction with knowledge on dental injury management was found to have a statistically significant direct correlation with witnessing a dental injury (p<0.05), and training on dental injury management (p<0.01), further suggesting confidence in knowledge with increased exposure to dental injury management. Results indicated that providers who had previously witnessed a dental injury or had training in dental injury management were more likely to recognize child care providers are responsible for managing dental injuries. Experienced providers with children of their own were more likely to agree timeliness plays an important role in tooth survival.
Regarding legal concerns, older providers were more likely to agree that legal concerns prevented them from getting involved in the event of a dental injury, while more experienced providers were likely to disagree. However, additional analyses showed no significant associations between age and legal concern response. Lastly, the 43% of “undecided” responses to the question surrounding legal concerns suggests child care providers’ lack an understanding about their legal role in such an event.
Discussion
Past research regarding knowledge and management of dental injury has been conducted among teachers and caretakers, primarily concerning injury to the permanent dentition.15-19,23-35 However, regarding the primary dentition, there is a lack of research regarding knowledge and first aid management of child dental injury among child care providers.1,2,5,10,36 This study provided insight on child care providers’ knowledge regarding dental injury, and first aid management concerning the primary dentition. Permanent dentition is seen as more urgent since parents do not understand the importance of primary teeth. However, primary dentition helps permanent teeth to grow in the proper position and if injured, underlying damage may occur to the permanent teeth, leaving significant risk of infection, decay, long lasting aesthetic affects or even tooth loss.19,20,26 As with most dental diseases, prevention is key. There is a general lack of information about this subject.
Similar to this study, Fux-Noy et al found elementary school teachers had limited knowledge about emergency care of dental injuries, and revealed comparable predictors of greater knowledge about dental injuries to the current study: being parents to children, previous experience with dental injuries, and increased age.17 Likewise, Fux-Noy et al reported 81% of elementary school teacher respondents were aware that replantation of primary dentition is not recommended,17 corresponding to the 76% found in this study.17 However, Fux-Noy et al reported that participants demonstrated less interest (42%) in receiving more information on the subject, compared to the 78% within this study, suggesting a lack of awareness on the importance of dental injury first aid among the elementary school teachers in Tel-Aviv, Israel.17 Fux-Noy et al also allowed participants to withdraw from the survey if respondents had a lack of knowledge on the subject, resulting in possible outcome bias.17
Level of satisfaction with knowledge on dental injury management was found to have a statistically significant direct correlation with witnessing a dental injury and training on dental injury management. These same predictors of knowledge on the management of dental injuries were found within previous studies.16,17,23,24
As per the results of the Spearman Rank Correlation analysis, there are some key findings from this study that could help inform future education in dental injury management. The finding that providers with less experience and no children were less likely to realize timeliness plays an important role in tooth survival suggests early education and training is essential. Additionally, this study’s findings indicated that older providers were more likely to allow legal concerns to prevent them from involvement in dental injury management, suggesting targeted education to older providers on the legalities of emergency dental intervention may be useful. Staff education and training on dental injury management should also aim to include a risk management component since participants indicated uncertainty regarding their specific role of responsibility in such an event.
This study had several limitations. The effective sample size of the study (100 respondents) may lack sufficient statistical power to detect important associations. In addition, survey participants were drawn from a convenience sample which may affect generalizability of the results to a broader population of child care providers. Furthermore, study findings may have been skewed due to the large percentage of white/Caucasian respondents and participants within the 19-29 year old age group. Lastly, due to the logistics used to solicit participants, the total number of potential respondents asked to partake in the study could not be enumerated, leaving the study response rate unknown.
Regarding generalizability of results, it is important to note that Connecticut and Massachusetts require a health or dental consultant be available regarding health and dental advice, to make quarterly visits (CT), as well as to review safety measures at child care centers.37,38 The 50 State Child Care Licensing Study of 2011-2013 reported that only 19 states within the US require health consultants (including dental consultants) be available to staff at child care centers. These states are Colorado, Connecticut, Delaware, Hawaii, Indiana, Maryland, Maine, Massachusetts, Minnesota, North Carolina, North Dakota, New Jersey, Nevada, New York, Oklahoma, Rhode Island, Washington, Wisconsin and West Virginia.39 The availability of a dental consultant could enhance health promotion education to child care providers and parents alike. A dental consultant could proactively address children’s oral health needs in a timely manner, and assist families with establishing a dental home.40
Conclusion
The findings from this study suggest a need for additional education on dental injury first aid for daycare providers. A dental injury management module could be included in conjunction with the required annual first-aid training for the day care center directors and staff, to promote professional development and oral health awareness. Further investigation on successful outcomes of these types of oral health interventions could be beneficial.
ABOUT THE AUTHORS
Kristine L. Sienkiewicz, RDH, MS, is a practicing dental hygienist in Milford, Connecticut; Lori Rainchuso, RDH, MS, DHSc, is the graduate program director at Forsyth School of Dental Hygiene; Linda D. Boyd, RDH, RD, EdD, is the dean of Forsyth School of Dental Hygiene; Lori Giblin, RDH, MS, is an associate professor at Forsyth School of Dental Hygiene; all are at the Massachusetts College of Pharmacy and Health Sciences University, Boston, MA.
References
1. Laughlin L. Who’s minding the kids? child care arrangements: Spring 2011. current population reports. Washington (D.C.): U.S. Census Bureau (U.S.); 2013 Apr. 23 p. Report No.: P70-135. Available from: http://www.census.gov/prod/2013pubs/p70-135.pdf.
2. Federal Interagency Forum on Child and Family Statistics. America’s children: National key indicators of well-being, 2013: Family and social environment figures. Washington (D.C.): U.S. Government Printing Office, National Center for Health Statistics (U.S.); 2013 July. 224 p. Report No.: AC-2013. Available from: http://www.childstats.gov/pdf/ac2013/ac_13.pdf.
3. Zaleckiene V, Peciuliene V, Brukiene V, et al. Traumatic dental injuries: etiology, prevalence and possible outcomes. Stomatologija, Baltic Dent Maxillofac J. 2014 Mar 21;16(1)7-14.
4. de Lourdes Drachler M, de Carvalho Leite JC, et al. Effects of the home environment on unintentional domestic injuries and related health care attendance in infants. Acta Paediatr. 2007 May 7;96(8):1169-1173.
5. Flores MT. Traumatic injuries in the primary dentition. Dent Traumatol. 2002 Sept 12;18(6):287-298.
6. Kargul B, Caglar E, Tanboga I. Dental trauma in Turkish children, Istanbul. Dent Traumatol. 2003 Mar 24;19(2):72-75.
7. Oliveira LB, Marcenes W, Ardenghi TM, et al. Traumatic dental injuries and associated factors among Brazilian preschool children. Dent Traumatol. 2006 Dec 5;23(2):76-81.
8. Onetto JE, Flores MT, Garbarino ML. Dental trauma in children and adolescents in Valparaiso, Chile. Endod Dent Traumatol. 1994 Jan 10;10(5):223-227.
9. Rodriguez JG. Traumatic anterior dental injuries in Cuban preschool children. Dent Traumatol. 2007 Aug;23(4):241-242.
10. Feldens CA, Kramer PF, Vidal SG, et al. Traumatic dental injuries in the first year of life and associated factors in Brazilian infants. J Dent Child (Chic). 2008 Jan 1;75(1):7-13.
11. Saroglu I, Sonmez H. The prevalence of traumatic injuries treated in the pedodontic clinic of Ankara University, Turkey, during 18 months. Dent Traumatol. 2002 Dec 11;18(6):299-303.
12. Skaare AB, Jacobsen I. Primary tooth injuries in Norwegian children (1-8 years). Dent Traumatol. 2005 Oct 28;21(6):315-319.
13. American Academy of Pediatrics. Dental emergencies: What parents need to know. [Internet]. Illinois: American Dental Association; 2015 Nov [cited 2016 Apr 2]. 1p. Available from: http://www.healthychildren.org/English/health-issues/injuries-emergencies/Pages/Dental-Emergencies.aspx.
14. Mouth Healthy. Dental emergencies. [Internet]. American Dental Association; 2014 [cited 2016 Apr 2]. 1p. Available from: http://www.mouthhealthy.org/en/dental-care-concerns/dental-emergencies.
15. Al-Jame Q, Andersson L, Al-Asfour A. Kuwaiti parents’ knowledge of first-aid measures of avulsion and replantation of teeth. Med Princ Pract. 2007 Jun 6;16(4):274-279.
16. Young C, Wong KY, Cheung LK. Emergency management of dental trauma: Knowledge of Hong Kong primary and secondary school teachers. Hong Kong Med J. 2012 Oct;18(5):362-370.
17. Fux-Noy A, Sarnat H, Amir E. Knowledge of elementary school teachers in Tel-Aviv, Israel, regarding emergency care of dental injuries. Dent Traumatol. 2011 Apr 28;27(4):252-256.
18. Raoof M, Zaherara F, Shokouhinejad N, et al. Elementary school staff knowledge and attitude with regard to first-aid management of dental trauma in Iran: A basic premise for developing future intervention. Dent Traumatol. 2012 Nov 20;28(6):441-447.
19. McIntyre JD, Lee JY, Trope M, et al. Elementary school staff knowledge about dental injuries. Dent Traumatol. 2008 Apr 10;24(3):289-298.
20. Malmgren B, et al. International association of dental traumatology guidelines for the management of traumatic dental injuries 3. Injuries to the primary dentition. Dent Traumatol. 2012 Jun;28(3):174-182.
21. Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? appraisal and recommendations. Research in Nursing and Health. 2007 July 24;30:459-467.
22. Caruso J, Cliff N. Empirical size coverage and power and confidence intervals for spearman’s rho. Ed and Psy Meas. 1997 Aug 1;57:637-654.
23. Arikan V, Sonmez H. Knowledge level of primary school teachers regarding traumatic dental injuries and their emergency management before and after receiving an informative leaflet. Dent Traumatol. 2012 Mar 13;28(2):101-107.
24. Al-Obaida M. Knowledge and management of traumatic dental injuries in a group of Saudi primary schools teachers. Dent Traumatol. 2010 Jul 14;26(4):338-341.
25. Karande N, Shah P, Bhatia M, et al. Assessment of awareness amongst school teachers regarding prevention and emergency management of dentoalveolar traumatic injuries in school children in Pune City, before and 3 months after dental educational program. J Contemp Dent Pract. 2012;13(6):873-877.
26. Sae-Lim V, Lim LP. Dental trauma management awareness of Singapore pre-school teachers. Dent Traumatol. 2001 Dec 21;17(2):71-76.
27. Addo ME, Parekh S, Moles DR, et al. Knowledge of dental trauma first aid (DTFA): The example of avulsed incisors in casualty departments and schools in London. Br Dent J. 2007 Apr 13;202(10):E27.
28. Al-Jundi SH, Al-Waeili H, Khairalah K. Knowledge and attitude of Jordanian school health teachers with regards to emergency management of dental trauma. Dent Traumatol. 2005 Aug;21(4):183-187.
29. Al-Jundi SH. Knowledge of Jordanian mothers with regards to emergency management of dental trauma. Dent Traumatol. 2006 Aug 10;22(6):291-295.
30. Bayrak S, Tunc ES, Sari E. Evaluation of elementary school teachers’ knowledge and attitudes about immediate emergency management of traumatic dental injuries. Oral Health Prev Dent. 2012;10(3):253-258.
31. Caglar E, Ferreira LP, Kargul B. Dental trauma management knowledge among a group of teachers in two south European cities. Dent Traumatol. 2005 Aug 30;21(5):258-262.
32. Chan AW, Wong TK, Cheung GS. Lay knowledge of physical education teachers about the emergency management of dental trauma in Hong Kong. Dent Traumatol. 2001 Dec 21;17(2):77-85.
33. Feldens CA, Kramer PF, Ferreira SH, et al. Exploring factors associated with traumatic dental injuries in preschool children: A poisson regression analysis. Dent Traumatol. 2010 Jan 11;26(2):143-148.
34. Lieger O, Graf C, El-Maaytah M, Von Arx T. Impact of educational posters on the lay knowledge of school teachers regarding emergency management of dental injuries. Dent Traumatol. 2009 Jun 9;25(4):406-412.
35. Mesgarzadeh AH, Shahamfar M, Hefzollesan A. Evaluating knowledge and attitudes of elementary school teachers on emergency management of traumatic dental injuries: A study in an Iranian urban area. Oral Health Prev Dent. 2009;7(3):297-308.
36. Arikan V, Sari S, Sonmez H. The prevalence and treatment outcomes of primary tooth injuries. Eur J Dent. 2010 Oct;4(4):447-453.
37. State of Connecticut, Department of Public Health. Statutes and regulations for licensing child care centers and group day care homes. Sect. 19a-79. (2013). http://www.ct.gov/dph/lib/dph/daycare/pdf/Statutes_and_Regulations_Centers.pdf.
38. Commonwealth of Massachusetts, Executive Office of Education. Family, group and school-age child care regulations and policies. Sect. 606 CMR 7.00 (2012). http://www.mass.gov/edu/docs/eec/licensing/regulations/2010-reg-family-group-school-age-child-care-programs.pdf.
39. Melusky R, Slavinsky E, Strauser M, Le A. The 50 state child care licensing study 2011-2013. Lexington (KY): National Association for Regulatory Administration (US); 2013 Apr. 729 p. Report No.:043 http://www.naralicensing.org/assets/docs/ChildCareLicensingStudies/2011-2013_child%20care%20licensing%20study.pdf.
40. American Academy of Pediatrics. Policy on oral health in child care centers. Pediatr Dent. 2016 Oct;38(6):34-36.