You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The National Cancer Institute (NCI) indicates over 300,000 men and women are living with a prior diagnosis of cancer of the oral cavity and pharynx in the United States (US).1 Additionally, the American Cancer Society (ACS) estimated over 48,000 new cases would be diagnosed in 2016.2 Approximately one in 100 men and women will be diagnosed with oral/pharyngeal cancer in their lifetimes.1 OC has a high five-year survival rate (83.3%) when detected early in a localized stage. Unfortunately, most cases are detected after metastasis, when the survival rate can drop by more than half.1
Although evidence regarding the efficacy of the OC screening in reducing mortality exists, it is inadequate.3-4 An American Dental Association (ADA) expert panel developed evidence-based clinical recommendations for OC screening which concluded, while community-based screenings may not reduce the mortality rate of OC in the general population, such screenings may reduce the mortality rate in high risk individuals. Further, the ADA panel concluded community-based screenings may result in detection of OC in earlier stages.5 NCI data indicate OC has an 83.3% five-year survival rate when detected early. However, the survival rate falls to 63.3% once cancer has spread to regional lymph nodes, and drops further to 38% with metastasis.1 Accordingly, the ADA guidelines supported OC screening as part of the visual and tactile oral examination for community-based and dental office settings, noting clinicians should also consider patient history and assess OC risk.5 These evidence-based clinical guidelines identified potential risks and benefits of OC screenings, including the psychological risk of false positives creating fear among patients, yet concluded that the benefit of early detection of treatable malignant lesions outweighed the risk of potential harms. In contrast, recommendations from the United States Preventive Services Task Force (USPSTF) indicate insufficient evidence exists to recommend for or against OC screening in asymptomatic adults in primary care settings, despite benefits of early detection.6
Similarly to OC, the risk of psychological harms was identified by the USPSTF (2016) as a risk of breast cancer (BC) screening.7 This review noted patients frequently report adverse experiences, including pain during screening, anxiety about the procedure, and apprehension about results. Psychosocial barriers identified regarding colon cancer (CC) screening included fear of the procedure, concern regarding preparation for the exam, and fear/apprehension of results.8-9 Despite the risk for these fears and concerns, screenings for breast and colon cancer continue to be recommended by the USPSTF.7,10 None of the studies included in the latest review of evidence from the USPSTF for prostate cancer (PC) screening provided information on potential psychological harms.11 The USPSTF recommendation for PC screening states research does not currently support the benefits of PC screening over potential harms; however, the NCI attributes the high five-year relative survival rate for PC to its early detection as a result of screening.12
In addition to psychosocial risks, cost has been consistently identified as a barrier to BC, CC, and cervical cancer screening utilization among consumers; cost as a barrier to OC screening has not been reported.8,13 Other attributes of these screenings, including time to perform the screening, efficacy, and the screening process itself, also have been identified. Factors including preparation prior to screening, discomfort/pain, and risk of complications have been cited as significant determinants of choice when deciding whether or not to have a screening performed.8,9
USPSTF screening recommendations for various cancers differ based on research available at the time of the recommendation. For many cancers, current ACS screening guidelines meet or exceed those of the USPSTF for average-risk individuals, particularly regarding screenings for BC and CC.7,10,14 The ACS recommendations for OC screening also exceed those of the USPSTF. The ACS recommends, in addition to the regular exam by a dental professional, physicians also examine the mouth and throat as part of a routine checkup, whereas USPSTF recommendations did not recommend for or against routine OC screening by primary care providers.6,15 While the USPSTF recommendations regarding OC screenings in the primary care setting do not apply to the dental setting, seemingly conflicting recommendations for screening from the ADA, ACS, and USPSTF may be confusing for the general public and oral health professionals, and result in fewer people being screened. Although most oral healthcare providers report regularly performing OC screenings, approximately half do not perform head and neck palpations and, therefore, are not performing a comprehensive exam.16-18
Some evidence indicates OC awareness is lacking among consumers, as multiple studies show low overall knowledge of OC, OC risk factors, and clinical signs in populations throughout the US and other countries. Previous studies have indicated consumers were largely unaware of the benefits of OC screenings, many were unaware that their oral healthcare providers screen for OC, and most reported never having received an OC screening.19-24 This low awareness may result from lack of communication from oral healthcare providers, as only half of those who report performing regular OC screenings report discussing the screening with their patients.17
Information regarding perceptions of the risks, benefits, and barriers to OC screening in relation to other cancer screenings is limited. Therefore, the purpose of this pilot study was to explore perceptions of Idaho adults regarding OC screenings as compared to other common cancer screenings including BC, PC, and CC screenings.
Methods
This quantitative pilot study was conducted using computer-assisted telephone interview software (CATI) due to a higher likelihood of an adequate response rate versus questionnaires distributed through an online format.25 An experienced survey firm was employed to conduct the survey.
A non-probability, convenience sample of Idaho adults (N=100) was utilized. The sample size was determined based on feasibility and cost. The random sample was purchased from a large sampling supplier. Inclusion criteria consisted of adults aged 18 years and older residing in Idaho. Exclusion criteria were non-English speaking individuals, those with a history of OC, and those respondents with cellular telephone numbers originating in Idaho but living out-of-state.
The study protocol was approved by the Idaho State University Human Subjects Committee based on expedited review (IRB-FY2015-86). At the onset of the telephone call to each participant, an introduction stating the purpose of the study and participants’ rights was provided, and verbal informed consent was obtained prior to administering the survey. Anonymity was maintained as no personally identifiable information was gathered in the interview or stored with participants’ responses.
The instrument was a self-designed, interview-administered questionnaire. A Content Validity Index was used to establish validity of the questionnaire using five experts in OC and/or health screenings. Questions deemed not relevant or only somewhat relevant by a majority of the experts were eliminated or revised. Each of the questions in the final instrument were deemed relevant or very relevant by the experts. Pilot testing then was conducted on the final instrument with a convenience sample (N=5) that met the inclusion and exclusion criteria. The survey was administered twice to these subjects, one week apart, to establish test-retest reliability, yielding agreement of 95%.
Trained, experienced interviewers were briefed by a supervisor regarding the project content prior to implementation using information supplied by the primary investigator. The interview-administered questionnaire was programmed into the CATI software and tested by the interviewers prior to implementation to ensure correct data were collected and assess whether the instrument was user-friendly for interviewers. Minor modifications were made and approved by the IRB. Landline numbers were programmed through a predictive dialer, which filtered the purchased sample and pre-coded numbers associated with faxes, computer phones, no-answers, etc. (any calls that were not “live”) before sending live calls to the interviewers to administer the survey. Cellular telephone numbers from the sample do not use the predictive dialer and were dialed by interviewers on a one-to-one basis per federal regulations. Participants’ survey responses required approximately five to ten minutes.
Demographic data were analyzed using descriptive statistics and frequencies. Categorical data from closed-ended questions were analyzed using Pearson’s Chi-Square test for association to examine distribution differences and relationships between variables. To minimize the likelihood of a Type I error due to multiple comparisons analyzed in each set of tests (i.e., OC compared to BC, CC, and PC), a Bonferroni strategy was used to maintain the family-wise error rate of 0.05, calculated by dividing the 0.05 error rate by the number of tests, in this case four, which indicated an alpha level of .0125 should be used for statistical significance for each chi-square test within the sets. A phi coefficient was used to determine the magnitude of effect size, or strength of significant associations, identified in the crosstabs according to the following scale: .1 weak, .3 moderate, .5 strong.26
Results
The pilot study sample included a total of 100 subjects, 47 males and 53 females. Participants were predominantly white (90%) and had a mean age of 52.7 years with a median age of 58 years. The majority of participants had some post-high school education (n=80) with most having completed a certificate (n=7) or degree (n=48) program (Table I).
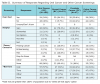
Table II summarizes participants’ responses regarding OC and other cancer screenings. For each of the selected screenings, the interviewer briefly described in layman’s terms what the screening may entail. When asking whether the participant ever had each screening, open-ended responses were coded as yes, no, or unsure/don’t know. No participants selected unsure/don’t know for any of the screenings. Over half of the respondents reported ever having had each of the following cancer screenings: (a) an OC screening (54% of all participants), (b) BC screening (94.3% of females), (c) PC screening (59.6% of males), and (d) CC screening (56% of all participants). The majority of respondents reported believing that cancer screenings were very helpful: (a) OC screening (60% of all participants), (b) BC screening (79.2% of females), (c) PC screening (63.8% of males), and (d) CC screening (84% of all participants). The majority of participants reported having had no fears or concerns regarding screenings for OC (86% of all participants), BC (60.4% of females), or PC (66% of males); however, only 35% of all participants reported having no fears or concerns regarding CC screenings. The most frequently reported barrier to any screening was cost: (a) OC screening (57% of all participants), (b) BC screening (51% of females), (c) PC screening (40.4%), and CC screening (61% of all participants).
Data regarding associations between participants’ responses regarding OC screenings and other cancer screenings are found in Table III. Crosstabs were calculated by gender of respondents because some of the screenings included in the chi-square analyses only applied to one gender (BC for females and PC for males). Although CC screenings are indicated for both groups, analyses were conducted by gender to maintain equality in sample size and statistical power. Crosstabs regarding ever having OC or other cancer screenings indicated the only statistically significant association was between OC and PC screenings (p=.007) with the phi coefficient indicating a moderate to large effect size (Φ =.391). A statistically significant association regarding participants’ opinions on whether or not screenings were helpful was found between OC and BC screenings (p=.006, Φ =.484) and between OC and CC screenings for both females (p=0.010, Φ =.563) and males (p=.000, Φ =.725) with a large effect size.
Further analysis examined associations between OC and other cancer screenings regarding participants’ fears and concerns (Table III). Fear of finding cancer was significantly associated with a large effect size when comparing OC and BC (p=.000, Φ =.564), OC and PC (p=.001, Φ =.474), and OC and CC for females (p=.000, Φ =.605); for males, OC and CC were significantly associated (p=.004) with a moderate to large effect size (Φ =.422). Fear of pain was significant only when comparing OC and CC screenings for females (p=.001, Φ =.438). Responses indicating no fears or concerns were only significant when comparing OC and BC (p=.003) with a moderate to large effect size (Φ =.413).
Crosstabs between OC and other cancer screenings were also examined in relation to participants’ responses regarding barriers to screenings (Table III). Cost of screenings was significantly associated with a large effect size when comparing OC and BC (p=.000, Φ =.492), OC and PC (p=.000, Φ =.531), and OC and CC for females (p=.000, Φ =.579) and males (p=.001, Φ =.500). When comparing time as a barrier to cancer screenings, significant associations with a large effect size were found between OC and PC (p=.000, Φ =.674) and OC and CC for males (p=.000, Φ =.528); a significant association also was found when comparing OC and CC for females (p=.006) with a moderate effect size (Φ =.377). Other barriers reported by respondents were statistically significant with a large effect size for OC and CC for females (p=.001, Φ =.473) and males (p=.000, Φ =.515). Additional barriers specified by participants included lack of awareness regarding need for OC screening and lack of opportunities for OC screening outside of the dental setting, concerns regarding radiation for BC screening, accuracy and risk of false positives for PC screening, and embarrassment, fear, and the preparation process for CC screening. Associations between responses of participants reporting no barriers to OC and no barriers to other cancer screenings were statistically significant with a moderate to large effect size when comparing OC and BC (p=.002, Φ =.424) and OC and PC (p=.007, Φ =.392).
When comparing perceptions of OC and BC screenings, a significant association was found between participants’ opinions on whether screenings were helpful (p=.006), fear of finding cancer as a concern (p=.000), and cost as a barrier (p=.000). When comparing perceptions of OC screening and PC screening, a significant association was found between participants’ fear of finding cancer as a concern (p=.001), and cost (p=.000) and time (p=.000) as barriers; therefore, the null hypothesis predicting no association between Idaho adults’ perceptions of OC screening and PC screening was rejected. When comparing perceptions of OC screening and CC screening, a significant association was found between male participants’ opinions on whether or not screenings were helpful (p=.000), both male and female participants’ fear of finding cancer as a concern (p=.004 and p=.000), female participants’ fear of pain (p=.001), and male and female participants’ perception of cost (p=.001 and p=.000) and time (p=.000 and p=.006) as barriers.
Discussion
Ninety percent of the respondents included in this pilot study were white; however, this proportion is reflective of the 93.5% white racial majority in the population of Idaho.27 Additionally, over half of the respondents in the sample reported having completed a trade/vocational certificate or degree, with four out of ten earning a bachelor’s degree or higher, whereas 24.4% of the Idaho population reportedly has earned a bachelor’s degree or higher.27 These respondents’ perspectives may have been influenced by being more highly educated than the general population. These sample characteristics are important considerations for this discussion of the findings. More diverse populations need to be included in larger national studies.
Slightly over half of these respondents self-reported ever having received an OC screening. This screening rate was high when compared to previous studies which indicated a rate of less than 30% despite the fact that all of these studies provided a description of the OC screening procedure.21,24 This higher screening rate may be due to the predominantly white, more highly educated, English-speaking population. Previous studies appear to indicate individuals with a lower socioeconomic status, blacks, and Hispanics are less likely to have received an OC screening.21,24
Data also indicated the vast majority of respondents reported perceiving no risks related to OC screenings. The most recent USPSTF report indicated no studies have reported harms from OC screenings; thus, it appears that these consumers had accurate perceptions regarding the low potential for risk of harms due to OC screenings. Self-reported rates for PC and CC screenings were comparable to those for OC at just over half; however, more than nine out of every ten females reported having had BC screening.
Similar to perceptions of OC screenings, the majority of respondents reported believing that all of the other cancer screenings were helpful and perceiving no risks regarding screenings for BC and PC. One in three participants, however, reported perceiving risks regarding CC screening, specifically mentioning in open-ended, follow-up questions preparation for the exam, embarrassment, pain, and fear of the unpleasant experience of the exam itself. These findings support those of Young and Womeldorph,8 which identified embarrassment, pain, and fear of invasive procedures, and Mansfield et al,9 which identified preparation and discomfort as barriers to CC screening.
The most frequently reported barrier to all of the selected cancer screenings was cost, despite large differences in cost among the various screenings. Cost has been reported in the literature as a significant determinant in BC, CC, and cervical cancer screening preferences.8,13 This pilot study is the first to identify cost as a potential barrier to OC screening.
Findings supported an association between consumer perceptions of benefits, risks, and barriers between OC and each of the selected cancer screenings. Respondents’ perceptions of the helpfulness of OC compared to BC and OC and CC for both males and females were significantly associated; however, perceptions of the benefits of OC compared to PC were not significantly associated. This finding is interesting because the majority of these respondents perceived all of the screenings as very helpful. There were statistically significant associations between respondents’ fear of finding cancer when comparing OC with BC, PC, and CC screenings, with the majority not experiencing fear of finding cancer as a concern for any of these screenings. This finding appears to indicate oral healthcare providers’ reported concern regarding the potential for fear or anxiety among patients by using the word “cancer” when discussing OC screening may be unfounded.17 In fact, despite low consumer awareness regarding OC overall, consumers have indicated they would like their oral healthcare provider to tell them they are being screened and would like to receive more information from their provider about how to reduce their risk of developing OC.19-24
Significant associations were identified in participants’ responses regarding barriers to OC and other cancer screenings. When comparing time as a barrier to cancer screenings, significant associations were found between OC and PC and OC and CC for both males and females, but not when comparing OC and BC. These associations may be related to a comparable amount of time for receiving OC and PC screenings; however, it appears that consumers were not aware of the significant difference in time required for OC screenings in comparison to CC screenings. OC screening takes minutes to perform as part of a routine dental examination, which typically requires one hour, whereas colonoscopy involves preparation the day before the procedure, sedation the day of the procedure, and the procedure time of approximately 30 minutes.
Cost as a barrier was significantly associated when comparing OC and BC, OC and PC, and OC and CC for both males and females. This finding implies a potential lack of consumer awareness regarding the cost of OC screening in comparison to other cancer screenings. The OC screening is commonly included with no additional cost in the comprehensive dental examination at $35-65, and the cost of a dental examination is low in comparison to costs of other cancer screenings.28 Cost Helper Health29 estimates the average cost of cancer screenings for uninsured and insured individuals. BC screenings average $102 for the uninsured, with an out-of-pocket cost of $10-35 for insured individuals. Estimates for PC screenings were $20-50 for a home PSA screening, increasing to as much as $120 in a hospital setting; a digital rectal exam ranges from $15-215, with copays of $0-30. The cost of CC screening, specifically colonoscopy, varies widely from $2010 to over $3000 with an average cost of $3081 for the uninsured. Out-of-pocket costs for insured individuals ranges from $0-1000 on average.29 The association between consumers’ concerns regarding the cost of OC and other cancer screenings may be related to insurance and reimbursement, as only 50% of the U.S. population was reported as having private dental insurance in 2010.30 In comparison, the CDC reported that 95% of U.S. adults had medical insurance including 67.3% with private insurance and another 17.7% with public health plan coverage in 2014.31 Clearly, there is a need for consumer education regarding the fact that OC screenings are low cost in comparison with other cancer screenings.
Opportunities for increasing OC screening rates will require consumer education regarding the need for regular screenings, increasing access, and addressing concerns about cost and time. Education is necessary, and begins with oral healthcare professionals informing patients about the procedure while it is being performed. The provision of OC screenings by advanced practitioners or dental hygienists in alternative settings may provide less expensive options for receiving OC screenings.32 Seeking broader healthcare coverage for preventive screenings, creating lower cost options, and better reimbursement options may also improve accessibility. Improving OC screening accessibility could lead to earlier detection, and earlier detection prior to metastasis has been shown to result in decreased mortality.1
Limitations of this study include the small, nonprobability sample, which precludes generalizability of the results beyond the sample of Idaho adults; however, the purpose of the study was to explore potential associations between consumers’ perceptions of OC with other exams so a broader study could be designed for a larger population. The primarily white, English-speaking sample may have had different perceptions than more diverse or underserved populations. The volunteer nature of the sample and the higher level of education of respondents also potentially influences the findings of the study as participants may have been more interested, knowledgeable, or motivated than the general population. Age may also be a limitation, as 23% of respondents were under 40, the minimum age at which some screenings (with the exception of oral cancer screening) are recommended. An older population could influence the number of respondents with screening experiences. Nonetheless, the protocol, validated instrument, and the insights gained regarding consumer perceptions of OC screenings in comparison to other cancer screenings can be used to inform subsequent studies.
Telephone surveys are becoming less representative of the general population due to a decrease in landlines and increased use of cellular telephones as the primary method of telephone communication. An attempt to compensate for this decrease in landline use was to purchase a sample consisting of a fifty-fifty combination of landline and cellular telephone numbers originating from Idaho, which is representative of the estimated 56.1% of Idaho homes with only wireless telephone service as reported by the CDC.33
Recommendations for future studies include a larger randomized sample representing a more diverse population, and the addition of a qualitative aspect to investigate reasons for selecting various options or why they were associated. The telephone would be the best method for survey administration; however, focusing on qualitative exploration of the basis of participants’ perceptions. Information regarding the timing of the most recent cancer screening(s) would also be beneficial.
Conclusion
This study of Idaho adults was conducted to compare perceptions of OC screenings to other cancer screenings using a self-designed interview-administered questionnaire. Results indicated the vast majority of participants perceived each of the cancer screenings as very helpful, and reported having no fears or concerns regarding screening. Lack of consumer awareness regarding differences between the selected cancer screenings was apparent based on perceptions of cost and time, the most commonly reported barriers identified for each of the screenings. This pilot study highlights the need to educate the public regarding the OC screening as it is embedded in the relatively inexpensive cost of the dental examination, takes minutes to perform, and is noninvasive and not painful. Future studies including a larger nonprobability sample representing a more diverse population are recommended to further explore the basis of participants’ perceptions and identify ways to minimize barriers to cancer screening.
About the Authors
M. Colleen Stephenson, RDH, MS is a clinical assistant professor; JoAnn R. Gurenlian, RDH, MS, PhD is a professor and graduate program director; Denise M. Bowen, RDH, MS is a member of the graduate faculty and professor emeritus; all from the Department of Dental Hygiene, Idaho State University, Pocatello, ID.
References
1. SEER stat fact sheets: Oral cavity and pharynx [Internet]. US Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2015 [cited 2016 Apr 5]. Available from http://seer.cancer.gov/statfacts/html/oralcav.html
2. Cancer Facts and Figures 2016 [Internet]. American Cancer Society; 2016 [cited 2016 Apr 5]. Available from http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdf
3. Detecting oral cancer: A guide for health care professionals [Internet]. US Department of Health and Human Services, National Institutes of Health, National Institute of Dental and Craniofacial Research; 2013 [updated 2014 Sep 9; cited 2016 Apr 5]. Available from http://www.nidcr.nih.gov/oralhealth/Topics/OralCancer/DetectingOralCancer.htm
4. Brocklehurst P, Kujan O, O’Malley LA, et al. Screening programmes for the early detection and prevention of oral cancer. Cochrane Database of Syst Rev. 2013; 2013 Nov 19(11): 1-34.
5. Rethman MP, Carpenter W, Cohen EW, et al. Evidence-based clinical recommendations regarding screening for oral squamous cell carcinomas. J Am Dent Assoc. 2010 May;141(5): 509-520.
6. US Preventive Services Task Force. Screening for oral cancer: US Preventive Services Taskforce recommendation statement. AHRQ Pub. No. 1305186-EF-2. Rockville, MD: Agency for Healthcare Research and Quality. 2013.
7. Nelson HD, Cantor A, Humphrey L, et al. Screening for breast cancer: a systematic review to update the 2009 U.S. Preventive Services Task Force. Evidence Synthesis No. 124. AHRQ Publication No. 14-05201-EF-1. Rockville, MD: Agency for Healthcare Research and Quality. 2016.
8. Mansfield C, Tangka FK, Ekwueme DU, et al. Stated preference for cancer screening: A systematic review of the literature, 1990–2013. Prev Chronic Dis. 2016 Feb 25;13(E27): 1-15.
9. Young PE, Womeldorph CM. Colonoscopy for colorectal cancer screening. J Cancer. 2013 Mar 15;4(3): 217-226.
10. Final recommendation statement colorectal cancer: screening [Internet]. US Preventive Services Task Force; 2008 [cited 2016 5 Apr]. Available from http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/colorectal-cancer-screening
11. Chou R, Crosswell JM, Dana T, et al. Screening for prostate cancer: A review of the evidence for the U.S. preventive services task force. Ann Intern Med. 2011 Dec 6;155(11): 762-771.
12. SEER stat fact sheets: Prostate cancer [Internet]. US Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2015 [cited 2016 5 Apr]. Available from http://seer.cancer.gov/statfacts/html/prost.html
13. Brown T, Lee JY, Park J, et al. Colorectal cancer screening at community health centers: a survey of clinicians’ attitudes, practices, and perceived barriers. Prev Med Rep. 2015 Jan 1;2(2015): 886-891.
14. American Cancer Society guidelines for the early detection of cancer [Internet]. American Cancer Society; 2015 11 Mar [updated 2015 20 Oct; cited 2016 5 Apr]. Available from http://www.cancer.org/healthy/findcancerearly/cancerscreeningguidelines/american-cancersociety-guidelines-for-the-early-detection-ofcancer
15. Oral cavity and oropharyngeal cancer [Internet]. American Cancer Society; 2014 16 Jul [updated 2016 27 Jan; cited 2016 5 Apr]. Available from http://www.cancer.org/acs/groups/cid/documents/webcontent/003128-pdf.pdf
16. Cruz GD, Ostroff JS, Kumar JV, et al. Preventing and detecting oral cancer: Oral health care providers’ readiness to provide health behavior counseling and oral cancer examinations. J Am Dent Assoc. 2005 May;136(5): 594-601.
17. Awojobi O, Newton JT, Scott SE. Why don’t dentists talk to patients about oral cancer? Br Dent J. 2015 May 8;218(9): 537-541.
18. Walsh MM, Rankin KV, Silverman S. Influence of continuing education on dental hygienists’ knowledge and behavior related to oral cancer screening and tobacco cessation. J Dent Hyg. 2013 Apr;87(2):95-105.
19. Awojobi O, Scott SE, Newton T. Patients’ perceptions of oral cancer screening in dental practice: a cross-sectional study. BMC Oral Health. 2012 Dec 18;55(12): 1-9.
20. Tomar SL, Logan HL. Florida adults’ oral cancer knowledge and examination experiences. J Public Health Dent. 2005 Dec;65(4): 221-230.
21. Patton LL, Agans RA, Elter JR, et al. Oral cancer knowledge and examination experiences among North Carolina adults. J Public Health Dent. 2004 Sep;64(3): 173-80.
22. Horowitz AM, Canto MT, Child WL. Maryland adults’ perspectives on oral cancer prevention and early detection. J Am Dent Assoc. 2002 Aug;133(8):1058-1063.
23. Paudyal P, Flohr FD, Llewellyn CD. A systematic review of patient acceptance of screening for oral cancer outside of dental care settings. Oral Oncol. 2014 Oct;50(10): 956-962.
24. Posorski E, Boyd L, Giblin LJ, et al. Oral cancer awareness among community-dwelling senior citizens in Illinois. J Community Health. 2014 Dec;39(6): 1109-1116.
25. Dillman DA, Smyth JD, Christian LM. Internet, mail, and mixed-mode surveys: The tailored design method. 3rd ed. Hoboken, New Jersey: John Wiley and Sons; 2009. 512 p.
26. Statistical interpretation [Internet]. US Department of the Interior, US Geological Survey, Fort Collins Science Center; 2016 [updated 2016 24 Feb; cited 1026 5 Apr]. Available from https://www.fort.usgs.gov/sites/landsat-imagery-unique-resource/statistical-interpretation
27. Idaho quickfacts [Internet]. United Stated Census Bureau; 2016 [cited 2016 5 Apr]. Available from https://www.census.gov/quickfacts/table/PST045215/16
28. Tarkan L. New oral cancer tests: Crucial or wasteful? The New York Times. 2009 2 Feb. Available from: http://www.nytimes.com/2009/02/03/health/03cancer.html?_r=0
29. Cost helper health [Internet]. Cost Helper [cited 2016 5 Apr]. Available from http://health.costhelper.com/
30. Dental services: Information on coverage, payments, and fee variation (GAO-13-754) [Internet]. US Government Accountability Office. 2013 [cited 2016 5 Apr]. Available from http://gao.gov/assets/660/657454.pdf
31. Health insurance coverage [Internet]. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Service for Health Statistics. 2014 17 Jan [updated 2016 27 Feb; cited 2016 5 Apr]. Available from http://www.cdc.gov/nchs/fastats/health-insurance.htm
32. Pew expert testifies on behalf of dental hygiene practitioners in Massachusetts [Internet]. Pew Charitable Trusts. 2015 29 Sep [cited 2016 5 Apr]. Available from http://www.pewtrusts.org/en/research-and-analysis/speeches-and-testimony/2015/09/pew-expert-testifies-on-behalf-of-dental-hygiene-practitioners-in-massachusetts
33. National health interview survey early release program [Internet]. US Department of Health and Humans Services, Centers for Disease Control and Prevention, National Service for Health Statistics. 2016 Feb [cited 2016 5 Apr]. Available from http://www.cdc.gov/nchs/data/nhis/earlyrelease/wireless_state_201602.pdf