You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Bruxism, a common condition seen in adults, is becoming more prevalent in adolescents and children.1 This course will provide information for the dental healthcare team on the common causes, assessment, diagnosis, and treatment of this condition. Early treatment can help prevent acute pain and, in severe cases, chronic pain, periodontal involvement and possible tooth loss.2 Educating the patient on bruxism and the importance of maintaining a healthy oral environment will also be covered.
Overview
Typically, bruxism has been considered a normal habit. Frequency of episodes and strength of forces on the orthodontia and periodontium can cause the habit to evolve into extensive pathological consequences. It may be as minor as slight wear on the teeth, to major consequences of consistent jaw pain to eventual loss of teeth. Early invention will lead to longevity of a properly functioning oral cavity and improved overall health.
History of Bruxism
The references of gnashing the teeth historically were described in negative annotations. The phrase to “grit one’s teeth” refers to grinding or clenching of the teeth in anger or to accept a difficult or unpleasant situation and deal with it in a determined manner.3 Clenching the teeth is generally used in humans and animals to display anger, hostility or frustration. In humans it was once an evolutionary instinct to clench the teeth for display to use as weapons to threaten a rival or predator. In many cultures the gnashing of teeth has been associated with suffering, physical pain, madness and possession. The history of bruxism, in the terms of gnashing and clenching, is mentioned in the Bible in several verses. Examples include: Psalm 35:16 “Like profane mockers at a feast, they gnash at me with their teeth.” Psalm 112:10 “The sinner shall see and be angry as he shall gnash his teeth and consume away.”
Over the years research has identified many reasons why people grind their teeth. In the beginning of the twentieth century, Moritz Karolyi, a Viennese dentist, described bruxism as “traumatic neuralgia” and stated “it was the cause of a periodontal condition called pyorrhea (periodontitis).” In 1907 the French term “Bruxamine” was introduced by Marie and Pietkiewicz. In 1931 Bertrand Frohman, MD created the term bruxism, which comes from the Greek expression “brychien odontas.”4 Sigmund Freud, scholar and psychiatrist, also had a theory concerning bruxing in the oral cavity. He claimed it to be a prime significance in the psychosexual development and behavior of the individual. Between 1966 and 2007 research and treatment were focused on occlusal adjustments and oral splints. During the 1960s, a periodontist, Sigurd Peder, DDS, PhD,5 promoted the theory that occlusal factors were responsible for bruxism. While therapy centered on the removal of occlusal interference remained unsatisfactory, behavioral approaches in research also declined during 1966-1986.
Occlusal habits can be a source of gratification or an outlet for aggression or frustration. For example, children suck their thumb for satisfaction or conversely children bite objects or people in anger or frustration. The adult is guided by morals, customs, traditions and other behavioral patterns where they cannot satisfy their emotional requirements as easily as children. Through the oral structure the adult will tend to resort to nail, lip and cheek biting along with clenching, grinding, clamping, and tapping of the teeth to release aggressions.6
The most recent research identifies there are many factors that are involved with bruxism including: lifestyle, stress factors, medications, mental and physical disorders and malocclusion.4
Definition of Bruxism
Bruxism is the involuntary gnashing, grinding, or clenching of teeth. It is usually an unconscious activity, whether the individual is awake or asleep; often associated with fatigue, anxiety, emotional stress, or fear and frequently triggered by occlusal irregularities. This usually results in abnormal wear patterns on the teeth, periodontal breakdown, and joint or neuromuscular problems.7
Patients may use clenching and grinding interchangeably, as if they are the same behavior, since their actions can cause similar results. While many people audibly grind and silently clench, they are different actions. Clenching is defined as clamping the teeth together firmly and tightening the jaw muscles.2 Clenching causes less obvious wear to the teeth but still results in substantial muscular soreness, pain and damage to the temporomandibular joint (TMJ) and periodontium. The terms grinding and bruxism are used interchangeably and involve repetitive movement of the TMJ with the teeth held together and/or by bracing or thrusting the mandible.2 Grinding visibly shows wear and flattening of the teeth along with substantial muscular soreness, pain and damage to the TMJ and periodontium.
Categories
Bruxism is classified into two categories:
- Primary (idiopathic) is when the disorder is not a related medical condition, or
- Secondary (iatrogenic) is when side effects of medications, neurological or developmental disorders are causing the behavior.8
Primary bruxism is further divided into two types: awake and sleep bruxism. Clenching or grinding of the teeth is a common activity that can occur both during the day and at night.
Awake bruxism happens during the day with clenching being more prominent. It is defined as awareness of jaw clenching and appears to be semi-voluntary. It is usually correlated with high anxiety and stress. Awake bruxism is relatively common involving 20% of the adult population and 18% of children. It affects females more than males.1 Awake bruxism symptoms usually worsen throughout the day. Clenching during the day increases the risks of clenching or grinding at night.
Sleep bruxism occurs at night while sleeping with grinding being more prominent. It is defined as a sleep-related movement and is involuntary. It occurs in about 8%-10% of the population, with a lack of awareness from about 80% of the bruxers. It effects both males and females equally.1,8 Sleep bruxism symptoms are usually worse in the morning, especially upon waking, and improve during the day.
One study reported sleep arousals induced sensory stimulation, which triggered episodes of sleep bruxism. Sleep arousals are a sudden change in the depth of the sleep stage and may also be accompanied by increased heart rate, respiratory changes and muscular activity, such as leg movements. It has been shown the majority (86%) of sleep bruxism episodes occur during periods of sleep arousal as a person goes from a deeper stage of sleep to a lighter stage of sleep.9
A typical sleep cycle is 90 to 110 minutes of sleep with three to five cycles per night. Sleep is determined by two categories: non-REM (quiet sleep) and REM (active sleep). There are four stages of sleep. Stages 1-2 are light sleep and stages 3-4 are deep sleep, with REM occurring in the third stage. A micro-arousal is a shift in sleep occurring in the deeper sleep. In this stage there are 3-10 second rises in brain activity, heart rate and muscle tone. Micro-arousals occur 8-15 times an hour, leaving bruxism secondary to these arousals. More destructive bruxers have greater amount of episodes and time in the REM stage.10
Children and Bruxism
Bruxism is very common in children. One in 5 children up to the age of 11 are reported to have sleep bruxism, although the real figure is probably higher as parents often are unaware. Children who brux usually begin at 4-8 years of age, the numbers increase between 10-14 years of age and then start declining after age 14. Many factors associated with children who brux are anxiety, personality, Attention Deficit/Hyperactivity Disorder (ADHD), and other parafunctional habits.4
It is challenging to determine if children have anxiety, although an anxiety state is a prominent factor in the development of bruxing behavior among children. A recent study concluded children with bruxism are more anxiety prone.11
Studies of personality traits in bruxism have been limited, but a conclusion was found that children who brux tend to be more tense than children who do not brux.11 Children with persistent anti-social and aggressive personality traits are diagnosed with having disruptive behavior disorder. Evidence proved anti-social children with persistent behavior problems as they grow older have a range of neurobiological characteristics, including bruxism.12
ADHD is considered to be a developmental disorder, mainly neurologic in nature, affecting 5% of the world’s population. Externalizing behavioral problems such as aggression and hyperactivity was proven as a correlation with anxiety and bruxism. This disorder is prevalent with bruxing and children. Children taking ADHD medication also have a higher occurrence of bruxism.13
Children tend to have a greater intensity, frequency and duration of parafunctional habits; finger and pacifier sucking and nail biting can increase the likelihood of grinding. These particular oral actions cause a motor stimulus to the central nervous system, which reacts with the alteration in the neurotransmission of dopamine–with the final result being clenching and grinding of teeth.4
Teeth grinding often occurs after children develop their first teeth and again after they develop their permanent teeth. The habit usually stops after the adult teeth are fully formed and erupted. The different heights and sizes of teeth in a mixed dentition causes the natural instinct to want to make the bite feel balanced. The body reacts by wanting to even out the taller teeth with the shorter teeth.
Management of bruxism in children can be challenging. As with adults, a night guard could be a treatment option; however, while children are still growing a night guard would not be the best recommendation. Another recommendation is to try relaxation techniques before bedtime to ease anxiety or restlessness. Children who fall asleep watching television or listening to the radio are more prone to bruxing at night. Reading aloud to children right before bedtime and having children sleep alone can decrease sleep bruxism.11
Common Causes of Bruxism
Stress, lifestyle habits, medications, medical conditions and occlusion are major contributors to grinding.
Stress
Stress is defined as a physical, chemical or emotional factor that causes bodily or mental tension and may be a factor in disease causation. Bruxism may be related to a person’s state of mind. Our bodies react to stress whether it is wanted or not.2 In a medical or biological context stress is a physical, mental or emotional factor that causes bodily or mental tension.14 Stress can be caused by external environmental sources, psychological or social situations. Internal sources such as illness or a medical procedure can also cause stress. Stress can initiate the “fight or flight” response, a complex reaction of neurologic and endocrinologic systems.8
Stress is simply a reaction to a stimulus that disturbs our physical or mental equilibrium creating unresolved emotions such as frustration, anger, competitiveness, aggressiveness, anxiety, tension, hyperactive personality or unresolved conflict. Suppression of feelings can also cause undue stress. The psychological factor is related to depression, anxiety and emotional stress, which plays an important role in starting and perpetuating bruxism as well as its frequency and severity. It is also believed depressed, anxious and emotionally stressed individuals present a greater predisposition for developing sleep bruxism as a response to releasing daily emotional stress.15 Since bruxism can be considered an emotional response, people who tend to suppress their feelings of frustration and anger and who tend to have aggressive, competitive, hurried personalities, and built up nervous tension are at an increased risk of grinding their teeth. Type A and hyperactive personalities also lead to bruxism. Stressful periods such as examinations, family bereavement, divorce or marriage, relocating, overworking, excessive worrying or any other situation that can add extra pressure can intensify bruxism.16,17
Lifestyle Habits
Many lifestyle choices can increase the cycle of bruxism, especially with the use of psychoactive substances such as alcohol, tobacco, drugs and caffeine.18
Alcohol. Drinking alcohol excessively doubles a patient’s chance of developing sleep bruxism. Bruxing tends to intensify after alcohol consumption. The occasional drink such as a glass of wine or two before going to bed to help one sleep better sounds good–but in reality, alcohol is known to break up sleeping patterns. If your patient sleeps poorly, this triggers their muscles to hyperactivate and the teeth to grind. It also increases the amount of arousal sleep.18
The mechanisms of action of alcohol on the central nervous system include alterations of the levels of:
- glutamate (neurotransmitters that send signals in the brain and throughout the nerves in the body),
- dopamine (the reward and pleasure center),
- serotonin (neurotransmitters that relay messages from one brain area to another, affecting mood, sleep, appetite, memory and learning, temperature regulation and social behavior),
- extrapyramidal regions (help regulate and modulate motion).
When these alterations are affected, it decreases the modulating role the glutamate neurons play on the dopaminergic system in the central nervous system. This action generates important alterations in behavior and motor activity, which in turn increases bruxism.4
Tobacco Use. Tobacco is a stimulant and affects the dopaminergic system. Bruxism in tobacco users is twice as prevalent as in non-users with sleep bruxism episodes five times more frequent per night. Bruxism related symptoms are three times higher in tobacco users than non-users. Users also notice and report bruxing more than non-users.4
Recreational Drugs. Stimulants in recreational drugs such as ecstasy, cocaine, methamphetamine (meth) and heroine increase bruxism. These drugs are central nervous system stimulants. Their mechanism of action is based on the neuronal transmitters in the brain with the dopaminergic system being the most involved. Neuronal transmitters are essential for functions in the central nervous system that involve learning, memory, sleep cycle, body movement, hormone regulation and many more.19 They also initiate motor disorders causing bruxism. Ecstasy generates the most concern in relation to severe awake and sleep bruxism. It can last in the system for 6-8 hours, with bruxism as a side effect in one-third of users. With regular use these drugs can promote bruxism leading to severe attrition in a short amount of time.4
Caffeine. Drinking caffeinated drinks, such as soda, high energy drinks, tea and coffee (six or more cups a day) increases the risks of bruxing. Caffeine has a half-life of six hours after it has been consumed. Caffeine is a stimulant that can promote muscle activity and cause frequent waking periods at night.20-22
Medical Conditions and Bruxism
ADHD – One of the most common childhood disorders that can continue through adolescence and into adulthood.23 A person is unable to control behavior due to difficulty in processing neural stimuli, accompanied by an extremely high level of motor activity.17 In ADHD, bruxism is caused by extensive sleep disturbances and medications used to treat the disorder.24
Autism – A neurodevelopmental disorder described by impaired social interaction, verbal and non-verbal communication and restricted and repetitive behavior. Bruxism can be caused by the antipsychotic medications used in its treatment, high stress and anxiety experienced with autism.25
Brain Injury – There are many conditions that fall into this category. The most common include: strokes, brain damage, dementia or Alzheimer’s disease and traumatic brain injuries, including concussions. Bruxism is a secondary disorder of these conditions.4
Cerebral Palsy – Considered a neurological disorder caused by a non-progressive brain injury or malformation that occurs during development of the brain. This condition primarily affects body movement and muscle coordination. Bruxism is a secondary disorder due to accompanying abnormal conditions in the oral cavity. These patients usually have a higher incident of crowding, variable sizes, shapes and misaligned teeth, all which can promote bruxing. They also experience frequent seizures and are more prone to head and mouth trauma, biting the lips and cheeks and grinding the teeth. Cerebral palsy patients can have trouble swallowing, chewing and can also be more susceptible to gagging and choking.26
Depression – A mental illness that causes sadness. A patient experiences a mood of sadness or a more severe condition of deep depression with possible suicidal thoughts. Patients may only have one episode depending on a particular life situation or with most people it is a reoccurring condition. Episodes may last a few months to many years. The state of mind including unconscious unresolved emotions and medications taken for depression may cause bruxing. Depressed individuals wanting to forget their problems tend to turn to alcohol and/or drugs, which is another source of bruxism.27
Down Syndrome – Also known as Trisomy 21, is a genetic disorder caused by all or part of a third copy of the chromosome 21. This condition is usually associated with physical growth delays, characteristic facial features and mild to moderate intellectual disability. These patients tend to have smaller than average teeth with shorter roots, missing teeth, and a Class III occlusion with crowding. This crowding results in some permanent teeth being unable to erupt. Bruxism is a common side effect of these oral conditions.28
Obsessive-compulsive Disorder – An anxiety disorder in which people have unwanted and repeated thoughts, feelings, ideas, sensations (obsessions) or behaviors that make them feel driven to do something (compulsion). Bruxism can be caused from the anxiety involved and from the side effects of the serotonin reuptake inhibitors medications used to treat this disorder.29,30
Parkinson’s Disease – A chronic and progressive disorder of the central nervous system, which involves the malfunction and death of vital nerve cells–causing a movement disorder. This condition is often treated with Levodopa, also known as L-DOPA. The brain converts it into dopamine which aids in body movement. Bruxism is a side effect of the long-term use of the medication Levodopa.31
Sleep Disorders – Conditions include snoring, breathing pauses during sleep, sleep apnea, obstructive sleep apnea, sleep talking or mumbling and consistent nocturnal awakenings. Violent injurious behaviors during sleep may include hypnagogic and hypnopompic hallucinations (visual, auditory or other sensory events that occasionally occur with the transition of falling asleep or waking up).32 These sleep disorders, along with the previously discussed mini arousals, prevent a sound consistent sleep and tend to increase the risks of bruxing.
Alternately sleeping on the left or right side can determine right or left side bruxing. Sleeping on one side for a long time may induce unilateral bruxism. Sleeping in the horizontal supine position can lead to bilateral bruxism with a high level of posterior neck pain and stiffness.33
Medications
Teeth grinding may also result as a medication’s side effect among those being treated for depression, developmental disorders, schizophrenia and those taking recreational drugs. Certain medications and drugs act on the brain by stimulating it. The results suggest brain stimulation is believed to contribute to grinding. Scientific data shows several neurotransmitters are involved in the effect of various drugs on bruxism. The dopaminergic systems in the striated body and the frontal lobe of the brain is of special importance, since hyperactivity generates bruxism, particularly the mandibular movement with tooth grinding.4
Common Medications With Side Effects of Bruxism
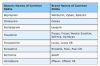
Selective Serotonin Reuptake Inhibitors (SSRIs) (Table 1) – Prescribed for depression, obsessive-compulsive disorder, anxiety, panic disorder, post-traumatic stress disorder, seasonal affective disorder, and depressive episodes of bipolar disorder, social phobia, premenstrual dysphoric disorder and menopause.2,34
In some reported cases where bruxism is thought to be initiated by SSRIs, decreasing the dosage may resolve the issue. Other sources state reports of SSRIs causing bruxism are rare and it only happens with long-term use.
Monoamine Oxidase Type B Inhibitors (MAO-B) (Table 2) – Prescribed for Parkinson’s disease and major depressive disorder.2,34
Dextroamphetemine Sulf-Saccharate (Table 3) – Prescribed for concentration, focus and fidgeting.34
Occlusion
Malocclusion, or bad bite, is more common among bruxers than in the general population. Misaligned teeth may serve as the cause of bruxism, not as its consequence. When bruxism involves more pressure on one side than on the other, it then becomes the cause of malocclusion.35 As the teeth wear down and the distance between the jaws decreases, overclosure may develop. Overclosure causes the anterior maxillary teeth to close in front of the anterior mandibular teeth, causing the vertical dimension to collapse.36
If occlusion is the cause of bruxism, orthodontics is the treatment of choice. Malocclusion is the main cause of bruxism in children and adolescents. The mixed dentition stage is a prime time for bruxism to occur. In a mixed dentition, the permanent teeth are larger than the primary teeth and may have erupted malaligned. This eruption or partial eruption may cause crowding and displacement of teeth, making it natural for the mind to want the teeth to be in centric occlusion.35
Clinical Signs of Bruxism
Attrition and Vertical Dimension
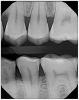
Attrition (Table 4) is the normal loss of tooth substance that results from friction by physiologic forces.7 Dental attrition is caused by tooth-to-tooth contact, resulting in loss of tooth tissue, usually starting at the incisal or occlusal surfaces. Clinical crown damage of the teeth can significantly thin the enamel structure, thus exposing the underlying structure called dentin (Figure 1). Dentin is softer and darker, increasing the risks of sensitivity, decay and discoloration. The etiology of dental attrition is multifactorial, with the most common cause being bruxism.
Due to attrition, the teeth will appear flattened from the wearing down of the occlusal surfaces of the enamel, causing enough reduction to alter the vertical dimension. Changes may be noticed not only by the reduction of the crown height, but also with the interproximal contact relationships. What was once a tight contact can eventually open up due to grinding the teeth down past the contact point.5 In this situation it eventually puts the mandible and maxilla closer together when in occlusion, bringing the nose and chin nearer to each other. This effect may also portray an older appearance. The jaw will appear sunken and deeper wrinkles of the skin around the mouth cause the lips to seemingly disappear.36
Wear Patterns
Wear facets are damage to the tooth, recognized as highly polished, smooth, flattened wear patterns on the enamel. This happens in unusual places for wear to logically occur through regular chewing. The distal corners of the maxillary central and lateral incisors are very common areas where damage from bruxism is noticed. Common canine wear facets are rounded over to the labial surface of the cusp tip, whereas normal mastication wear blends over to the lingual surface.5
Canines tend to show the first visual signs of bruxism because the anatomy of a canine is longer and more pointed than other tooth types. Wear facets or flat canines are obvious visual signs of grinding (Figure 2). As the canines become shorter and become in line with the occlusal line of the premolars, the force is then shared with the rest of the molars (Figure 3). Signs of attrition on molars start with the cusps flattening out and can even wear through to the dentin.37
First molars can show significant wear since they are one of the first permanent teeth to erupt in the oral cavity. Having the longest longevity in the mouth leaves them exposed to maximum activity over a lifetime. They withstand bruxing through mixed dentition and before orthodontics is initiated to adjust malocclusion. Usually if there are wear signs on the mandibular, there will be complementary wear signs on the maxillary. Wear facets may also show unilaterally (for a more dominant side of bruxing) or bilaterally (equal throughout the mouth).5
Abfractions
Abfraction is a mechanism that explains the loss of enamel and dentin caused by flexure and ultimate tissue fatigue of susceptible teeth at locations away from the point of loading. The breakdown is dependent on the magnitude, duration, frequency and location of the forces located at the cervical area of the tooth.4,7 This happens when the tooth has flexed greatly during the grinding process and the root surface begins to break down and form a scooped or notched out appearance. It is the mechanical failure of the tooth structure.10
Chipping, Breaking, Cracks and Fractures
Putting a constant amount of force on the enamel weakens the area and can contribute to small fractures, which lead to chips and breaks.7 As teeth wear, the edges of the anterior teeth and the cusps or corners of the posterior teeth will begin to show micro-fractures or cracks, which usually cannot be seen on radiographic images (Figure 4 and Figure 5). Sometimes patients think these fractures are cavities because they can become stained or discolored and may be sensitive to hot and/or cold. As these fractures deepen to the constant pressure, they will eventually chip, break a corner, or damage the pulp requiring endodontic (root canal) therapy. In extreme cases the tooth may need to be extracted. The fracture begins on the outer surface of the tooth and eventually deepens until the crack enters the nerve, which leads into cracked tooth syndrome–an etiology of bruxism.21,37
Periodontal Recession and Bone Loss
Periodontal patients can be the most challenging group of patients to control the repercussions of grinding. Bruxism can be a serious, aggravating factor in periodontal disease because it can interfere with the normal recovery time of the periodontium. Regeneration of the tissue is constantly taking place, and adding bruxism disturbs the circulation by interfering with the functional adaptability and regeneration of the periodontal tissues. Bruxism and periodontal disease in all stages contributes additional stress and strain on the diseased tissues. This increases the risks for tissue breakdown and reduces the rate of regeneration. Disturbances caused in the periodontium by altering the circulation can cause interference with the nutrition of the periodontal tissues.38,39
When patients grind their teeth, they add axial and bone-in stress. Axial stress is excessive force applied vertically to the teeth and periodontum.7 Bone-in stress is the response of the bony structure to applied force. Application of excessive pressure stimuli to bone may cause the formation of thicker and more numerous trabeculae. If tissue components cannot compensate for excessive stress, bone resorption will occur. Localized bone destruction or an isolated periodontal pocket may occur with bruxing.37
Mobility
If mobility is caused by bruxing, there usually will not be any signs of periodontal pocketing. The periodontal ligament may respond to increased occlusal forces by resorbing some of the bone of the alveolar resulting in mobility.4 With bruxing, the teeth are forcefully rocked back and forth in the socket, which can cause temporary mobility, progressing to risks of permanent mobility.5 Tooth mobility with sleep bruxism is greater in the morning and is significant when found in teeth with little or no evidence of periodontal disease. Such teeth may exhibit a dull percussion sound and patient may report soreness when biting on the tooth or teeth.5
Buccal Exostosis and Tori
Bony out-growths that form where there is an excessive amount of stress and tension placed on the teeth’s underlying structures are called tori or exostosis. With excess strain and tension placed on the teeth and jaws, the body’s defense is to produce extra boney material to support the teeth. This bone grows and becomes visible under the soft tissue. They are commonly seen in patients who clench or grind their teeth. Exostosis of the maxilla and/or mandible may be the result of bruxism. Exostosis tends to recur if bruxism continues after their removal.5,42
Force and Wear
The masseter muscle is considered one of the strongest single muscles in the body and can produce substantial force.43 In the natural relaxed state the maxillary and mandibular teeth are separated by about 2-3 mm of space. Teeth usually come into contact with each other when chewing and swallowing, using a force of less than 25 pounds of pressure, with food to buffer direct contact with chewing. When bruxism is involved, there is an abnormal increase in magnitude, frequency and duration elevating the pounds of pressure to increase to the maximum biting force of 200 to 300 pounds of pressure.5,16,39,43,44 The grinding force compared to regular mastication is three to ten times more powerful–enough to crack a walnut.10,45 Functional tooth contact during a 24-hour period is approximately 20 minutes. Excessive forces generated by bruxism extends for more than 20 minutes.16 Normal tooth wear in non-bruxers is considered to be ~29 um (micrometer) in molars and ~15 um in premolars per year. Dental enamel loss of ~10-40 um occurs from friction of normal biting or chewing, while the forces generated for mastication are between 20-120 Newtons (N). When bruxing, the load can be as high as 1000 N, changing normal physiologic wear to severe wear, leading to fatigue failure and fractures.4
Audible Occlusal Sounds
Bruxism many times is diagnosed from a bed partner or someone observing the patient during a napping time who is disturbed due to the noise produced by grinding. The audibility is determined by the tooth-to-tooth friction, the area in which the grinding occurs and the force of the grinding.5 The sounds can be described as crunchy, chewing on gravel, rocks or marbles.
Symptoms
Acute or Chronic Pain
Fortunately or unfortunately, bruxism aches and pains are a functional, healthy response. It is the body’s way of sending a message that something is not in sync and an adjustment needs to occur. Any injury to the body causes other muscles, ligaments or tendons to overcompensate for the injury. Over time, those compensations also become weak and unproductive. Common aches or pains can progress from mild to severe depending on the aggressiveness and repetitiveness of the bruxing.
Any of these pains can be acute (comes and goes) or chronic (comes but never goes). Teeth sensitivity can be very specific or generalized. Jaw pain can be from the muscles or joints and can feel overworn, fatigued, stiff or throbbing. Headaches can be in the morning or night, constant or fluctuating and can range from a slight dull pain to an intense migraine. Cheeks can feel tired, worn or sore when chewing. The TMJ can have inflammation, become locked or have limited opening of the mouth. Earache pain can feel like a dull pain or an intense shooting pain leading into the ear. Neck and shoulder pain can feel dull, stiff, achy or intense.46
When grinding with the anterior teeth, there may not be any pain beyond those specific teeth. But when grinding the posterior teeth, the masseter and temporalis muscles are more involved, which can create more facial and head pain.4 Myalgia may worsen during function, along with tenderness on palpation.16
Sensitivity of the Teeth
Sensitivity can be localized, generalized, constant or sporadic. One of the first symptoms of bruxism is hot and cold sensitivity to the teeth. This is caused by the flexing that occurs when teeth are ground from side to side. Teeth were not designed to flex, so they deteriorate at the areas of bending above the gingiva.4 This area can become very sensitive with abfractions developing at the roots and causing receding gingiva. Many times patients do not know which exact tooth is causing the sensitivity, or even if it is maxillary or mandibular. When there are not obvious signs of bruxism, treatment is usually desensitizing toothpaste, which temporarily resolves the problem.
Sensitivity related bruxism can be challenging to diagnose. The thinning of enamel can cause underlying dentinal sensitivity. The tooth may acclimate to the new conditions. Additional enamel loss and reacclimation may lead to the “coming and going” symptoms of sensitivity.
Jaw Pain
A common symptom is pain in and around the TMJ. This pain is usually felt when opening and closing the mandible; however, it can also occur while the mandible is in the resting position. Discomfort can occur through hyperactivity, spasms or overworked muscles. As with any other muscle, when contracted for a long period of time, the muscle fibers start to present fatigue or inflammation that produce the pain. Overt tissue damage, injury or trauma and overloading stress of the jaw muscles and TMJ during bruxism can activate nociceptors (receptors for pain stimulated by various kinds of tissue injury and pain).4,46 These conditions can cause inflammation of the stressed areas and coincidentally cause pain as well. This type of pain is characterized as a fairly prolonged, deep dull ache, often similar to the discomfort associated with a nagging headache. A sharp, brief shooting pain or a feeling of numbness in the orofacial area is another symptom. Bruxism can cause stiffness in the TMJ and masseter muscles.
TMJ Discomfort
Changes that happen in the TMJ arise from pathologic processes more than physiologic adaptation, which can cause the entire dentition to undergo a continuous adaptation to functional wear. Adjustments in the orofacial region are constantly being supported by the wear caused by bruxing.47 Repetitive overloading of the TMJ through bruxing can be a factor in osteoarthritis. Bruxing pain in the TMJ area includes the retrodiscal pad, synovial membranes of the joint capsule and collateral ligaments of the disc-condyle complex.47 Bruxism can cause nightly bruising of the TMJ with a dislocated disk and can sometimes function as a sustaining factor in the cycle of pain and muscle tightness.47
Patients with Temporomandibular Disorder (TMD) often hear clicking, popping, or grating noises in their TMJ.4,46,47 The clicking noise commonly heard and palpated during opening or closing is a result of this disc slipping out of place, sticking, or malfunctioning. Although some clicking and popping sounds in the TMJ can be normal and insignificant, when the sound is grating or gravel like, the joint and disc may be breaking down (degenerating). This requires a more involved evaluation. Clicking sounds may occur in one or both joints when the bony joint and disc movement are not coordinated. The click may occur when opening or closing and with lateral movements as well. The jaw may shift to the side and may catch or lock during any of its movements.48 Although the disc can quickly reorient itself and normal jaw function can be restored, sometimes this problem can worsen. The disc wear can continue and result in a more severe displacement. Occasionally, this can be a painful event that results in a reflex contraction of the chewing muscles which locks the TMJ in an open dislocated position. This is referred to as an open lock.48 When these situations arise, a referral to a TMD dental specialist would be most beneficial for the patient.
Muscles, Neck Pain and Headaches
Since the masseter muscle is considered one of the strongest single muscles in the body, when the muscle is worn and fatigued from bruxing, it can cause localized and referred pain.43,49 The masseter alone can be inflamed and fatigued, causing localized pain. The masseter attachment trigger points at the upper superficial layer can have referred pain points to the mandible, teeth and gingival area. The mass superficial layer can also have referred pain patterns to the mandible, teeth and gingival area. The attachment trigger point of the lower superficial layer refers pain to the mandible and above the eyebrows. The trigger point of the upper posterior deep layer below the TMJ refers pain to the ear area.49-51
Even if muscle pain does not occur, muscle hypertrophy can result.16 Bruxism involves excessive muscle use, which can lead to enlargement of the facial muscles. In long-term bruxers this enlargement can cause a square jaw appearance.52
Bruxism may lead to chronic headaches, although the correlation is not entirely clear. One perspective could be the aches and pains are from disturbed circulation in the muscles. Another suggestion is the tightening of the entire mandible and face during bruxing can cause headaches.5,50 Bruxers are three times more likely to experience headaches than non-bruxers.18 The use and tightness of the masseter muscles and the clamping down of the dentition connects with the neck muscles causing neck pain.52
Diagnosis
Diagnosis initially starts with the patient’s concerns during the dental appointment. The common chief complaint with patients is usually some level of pain, whether it is persistent or inconsistent, from slight sensitivity to intense pain. Patients will usually state generalized or localized hypersensitivity or pain in their teeth and/or jaw. The patient may also become aware of their clenching habits during times of stress or depression. They will sometimes know exactly which tooth. Other times they will know the area but are unable to pinpoint the exact tooth.
After determining decay is not the issue, noticing any wear facets could be the confirmation of teeth grinding. Symptoms related to the mandible or face are: pain, soreness, tiredness, achiness, tightness or stiffness usually from the pressure and overuse of the masseter muscles or TMJ. Headaches are another common symptom, especially when it is experienced after wakening. These headaches can be dull or intense, sometimes leading to migraines.17
Over the years, the accumulated toll of bruxing can produce a wide range of damage or oral changes. Duration, frequency and intensity of bruxing significantly contributes to the resulting effect.4,16,52,53
Radiographic Appearances
Enamel appears flat or thin on the incisal and occlusal surfaces. It may be localized, but usually is generalized. Small chips on the incisal edges may show radiographically along with broken teeth or restorations. Radiographically it would show widening of the periodontal ligament and bone resorption due to trauma enforced by the grinding.4 Pulpal necrosis may be visible (Figure 6 and Figure 7).
Habits
Bruxism is considered the most destructive functional disorder of the dentition. Certain habits can increase the chances of developing and exacerbating bruxism.15
These include:
- Verbal grinding noise when sleeping
- Sleep talking
- Restlessness at night
- Snoring which can alternate the sleeping arousals increasing the chance of grinding
- Biting or chewing on the cheeks, lips, fingernails, pencils or other objects. Also, candy sucking or any activity that keeps the mouth busy or on alert regularly, trains the mouth to stay active even when sleeping. These habits make patients more susceptible to grinding their teeth since these habits have a typical cyclic occurrence similar to bruxism.5
- Chewing gum keeps the cheek muscles tight and tense when ideally the muscles should be relaxed.
- Tobacco use
- Drug use
- Alcohol use
- Caffeine consumption
Treatment Modalities
The goals of treatment are to reduce the pain, prevent permanent irreversible damage to the teeth and surrounding structures and reduce grinding as much as possible. Starting with home self-care remedies would be the initial conservative approach for treatment.4,54
Home Care
- Apply ice or heat to sore jaw muscles
- Avoid eating hard foods
- Avoid chewing gum
- Drink plenty of water
- Do stretching exercises for the face
- Massage the muscles of the neck shoulders and face
- Relax the face and jaw muscles
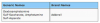
Night Guards – Custom Made or Generic
Night guards are one of the most popular treatment options for sleep bruxism (Figure 8). The goal of a nighttime therapy appliance is to redistribute occlusal forces, relax the masticatory muscles, stabilize the TMJ, protect the dentition and dental work, decrease the symptoms and, hopefully, reduce bruxism.16,55 Night guards can last an average of a few months to years depending on the force and frequency of grinding. There are a variety of night guards; choosing and advising the patient on the correct night guard is important.
Night guards should be worn to protect restorations and be recommended to patients who grind and have multiple crowns, bridges or implants due to quicker failure of restoratives. Periodontal patients who show any symptoms of bruxism, or if the patient acknowledges they grind their teeth, should be educated on the need of a night guard for protection. The patient must maintain the periodontium since they have less bone and tissue attachment, and additional loss is more detrimental to periodontal treatment plans. Night guards also maintain space between the teeth so the muscles of the jaw cannot fully contract and remain relaxed.
Custom Night Guards. For aggressive consistent grinders, a harder night guard should be recommended. A hard/ soft type is 1 mm soft polyurethane for the inner layer and a 3 mm hard, more durable co-polyester outer layer.53 For less aggressive and episodic grinders, a softer night guard may be recommended.
Custom made night guards are usually the best option for the patient. The fact they are custom fitted makes them the most comfortable and, therefore, patient compliance is improved with custom guards.
The process for constructing this appliance is a two-appointment procedure. At the first appointment, impressions of the maxillary and mandibular arches are taken. The impressions can be sent to a dental laboratory or the appliance can be fabricated in the office. Usually mouth guards are fitted to the maxillary. Sometimes a mandibular night guard will be made if the patient has trouble with gagging or comfort. The second appointment is for delivery and to confirm the night guard fits, feels right to the patient and to instruct them on the care of the night guard.
Generic Night Guards. Since custom-made night guards can be expensive and insurance companies sometimes do not cover the cost, another option would be to purchase an over-the counter generic night guard. There are “stock” night guards which come in small, medium and large. These night guards tend to be bulky, uncomfortable and hard. Their discomfort can lower patient compliance.
Another option is boil and bite night guards. These tend to be more comfortable than the stock night guards, although damage due to biting pressures reduce the life of this type of guard. The night guard is boiled until the plastic softens, cooled enough so as not to burn the soft tissues, and then placed in the mouth. The patient is instructed to press against their lips to aid in overall formation. As it hardens, it conforms to the teeth for a better fit.
Some patients may have a learning curve period with an oral appliance. Many times patients will wake up during the night or in the morning with the night guard out of their mouth. It is suggested the patient wear the appliance for short amounts of time throughout the day or right before bedtime. This will help the night guard not feel as foreign, make it easier to fall asleep and increase the chance it will remain in place all night.
Medications
Different medications have been prescribed by a physician or dentist to treat bruxism including benzodiazepines, anticonvulsants, beta-blockers, dopamine agents and muscle relaxants.
Anxiolytic (muscle relaxers) are prescribed for sedation and hypnotics to treat anxiety and insomnia. These drugs have a temporary effect on jaw muscle activity. The maintenance of their therapeutic efficacy is resourceful, however the long-term tolerability and risk of addiction could be harmful.4
Benzodiazepines have hypnotic, anti-anxiety, anticonvulsive and muscle relaxing effects. They affect the central nervous system and focus on the inhibitory neurotransmitter, mainly the GABA. The effects on the spine are mainly related to the muscle relaxing effect, while the action in the limbic system and cortical areas affect behaviors and emotions.4
Buspirone’s mechanism of action is based on its agonism for serotonergic receptors, interacting mainly with the 5-HT1A receptor, at both the presynaptic and postsynaptic levels. Its treatment in bruxism is owed to its anxiolytic action and its interaction with the serotonergic and dopaminergic systems.4
Antiepileptics (anticonvulsants) are prescribed for epilepsy and clinical management of orofacial pain such as idiopathic trigeminal and postherpetic neuralgia.4 The beneficial effects on neuromotor diseases, such as epilepsy, have led clinicians to test for the treatment of bruxism.
Gabapentin was studied and used for severe bruxism incurred by SSRI drugs and showed significant improvement.4
Clonazepam has evidence-based proof in managing sleep bruxism for the short term. Its risks include addiction and mild respiratory depression.29,33
Tiagabine is used for muscle spasms, neuropathic pain, anxiety and post-traumatic stress disorder. It inhibits the reuptake of the neurotransmitter GABA at the synaptic terminals. Besides its anticonvulsive actions, it increases the sleep stages 3 and 4, therefore decreasing sleep bruxism. It is the only antiepileptic drug which helps increase the sleep stages.4,29,56
Adrenergic antagonists and agonists are beta blockers that are prescribed for hypertension, ischemic cardiopathies and some arrhythmias.54 These medications have shown a beneficial effect on bruxism–specifically the medications propranolol and clonidine. The hypothesis is these adrenergic antagonist drugs are useful in the clinical management of bruxism through the cardiac rhythm increasing during episodes of sleep bruxism. This suggests a possible relation between the activation of the sympathetic system and bruxism. Since tachycardia occurs in bruxism episodes, the data has strongly suggested a relationship between the autonomous nervous system and mechanisms of bruxism.20
Propranolol has shown relief for bruxism. Clonidine’s pharmacological effect is generating changes in arterial pressure and heart rate. This medication decreases the sympathetic activity during sleeping and decreases sympathetic tone during the minutes preceding the onset of sleep bruxism.
Dopamine agents (agonists of dopaminergic receptors) are prescribed to activate dopamine receptors. Bromocriptine is a dopaminergic D2 agonist that works both at the central and peripheral levels. Small doses have proven to reduce bruxism, but in the study many participants abandoned the drug because of the side effects.4
Another Dopaminergic D1/D2 agonist is Pergolide (Prascend). This drug was used for severe bruxism and used and studied in patients prior to receiving dental implants. Studies showed a significant improvement in bruxism episodes lasting up to a year even with interrupted use.52 This medication is no longer available in the US market due to a link of increased rates of valvular heart disease. It is still used in other countries for the treatment of Parkinson’s disease.57
Acupuncture
Acupuncture is meant to re-align structural imbalances, reduce muscular tension, pain management and calm the nervous system. By unblocking the energy circuits that run through the jaw area, along with a general tonification of yin energy will usually do the trick. When dental pain is the issue, acupuncture treatment opens the channels toward the maxillary or mandibular jaw and soothes and detoxifies the meridians near the affected area, bringing pain relief.58
Massage
Grinding and clenching affects the masseter muscle the most often, since it is the largest and strongest muscle of the orofacial structure. When patients grind their teeth, it is usually the masseter muscle that is sore and inflamed. Massaging brings the circulation of the blood and nourishments to the muscles for healing while releasing the inflammation of the jaw, face, TMJ, neck, shoulders and upper back areas.43
Other massage benefits are: decreasing muscle pain and tension, relieving anxiety, stress and tension, relaxing muscles, alleviating headaches, facilitating removal of waste and inflammation by-products, stimulating the immune system and promoting relaxation and comfort.59
Botulinum Toxin (Botox)
Botulinum toxin (Botox) can lessen bruxism’s effects. In an extremely diluted form, botulinum toxin is injected to weaken (partially paralyze) muscles and has been used extensively in cosmetic procedures to “relax” the muscles of the face.60 Bruxism is regarded as a disorder of repetitive, unconscious contraction of the masseter muscle. In the treatment of bruxism, Botox weakens the muscle enough to reduce the effects of grinding and clenching, but not so much as to prevent proper use of the muscle. Although the intent of Botox injections is for the Botox to go into the muscle and not into the rest of the body, it has been shown some percentage of injected Botox winds up in the vascular system and migrates to other parts of the body. Botox treatment typically involves five or six injections into the masseter muscles.61 It takes a few minutes per side, and the patient usually starts feeling the effects the next day. Headaches and TMJ injuries could also be relieved with these injections.60
Biofeedback
Biofeedback is a treatment used to treat daytime clenchers by using electronic instruments to measure muscle activity and teach patients how to reduce muscle activity when the biting force becomes too great.4
Exercise
Exercise helps relieve stress by increasing the immune and circulatory systems which helps with a peaceful night’s sleep and increases serotonin and dopamine. Hobbies for relaxation such as meditation or yoga can relieve bruxism tendencies.
Natural Remedies
Calcium and Magnesium. Some research states bruxism could be caused by deficiencies in magnesium and calcium. Magnesium’s vital role is in nerve and muscle function. A magnesium deficiency causes muscle spasms. Increasing magnesium intake will help relieve muscle tension. Calcium deficiency causes muscle cramps and involuntary movement of muscles, the facial muscles included. Increasing calcium levels will help with muscle cramps and support bone strength which can prevent bruxism by supporting neural development.61
There are some recommended calming herbs such as Chamomile, Hops, Skullcap, and Valerian. These all have relaxing properties known to reduce anxiety and to help the body fall into a deeper sleep.62 The use of essential oils, such as lavender and chamomile oil, may also promote a deep energizing sleep.
Patient Education
Diagnosing the cause of bruxism is important for determining treatment options. Over 80% of bruxers are unaware, in denial or ashamed they have a grinding habit.40 Utilizing printed patient education materials as well as educational sources, intraoral cameras, radiographic images, websites and pamphlets will help give patients a visual view. Also, educating patients by personalizing and making them aware of the damage already done and what the future consequences could be for them if they do not accept treatment.
Discussing costs of restorative treatment such as restorations, crowns and even possible future implants versus the cost of a night guard or behavioral changes will usually motivate a patient into positive action.
It is always more beneficial if the problem can be resolved rather than only treating the symptoms. If the bruxism is caused by stress, then stress-relieving techniques should be implemented, possibly involving the patient’s physician. The following points are important to patient education:
- Periodontal patients who show any symptoms of bruxism, or patients who acknowledge they grind their teeth, should be informed of the need for a night guard.
- If bruxism is caused by medication, discuss ways to have the medication lowered or completely eliminated. Consult with the patient’s physician. If the medication is temporary, let the patient know bruxism is a side effect so they can be aware of changes in the oral cavity.
- If the patient engages in tobacco use, drinking or recreational drugs caused the bruxism, then cessation discussions should be considered.
- If bruxism is caused by occlusion dysfunction, whether it is a slight or severe malocclusion, missing teeth or a high bite, a thorough examination with a treatment plan would be more beneficial for the patient than maintaining the symptoms.
- Caution the patient to avoid stimulating substances in the evening. Avoid caffeinated drinks such as coffee, tea or soda after dinner and avoid alcohol and tobacco use during the evening, as they may worsen bruxism.
- Advise the patient to reduce stress. Listening to music, taking a warm bath or exercising can help the patient relax and may reduce the risk of developing bruxism.55
- Ask the patient about their sleep habits, i.e., do they talk in their sleep, move, twitch or jump (muscle spasms) a lot while sleeping? Do they feel unrested after sleep, do they experience nocturnal awakenings? These could be signs of not sleeping well, which could be a cause of bruxism.55
- Schedule regular dental examinations. Dental examinations are the best way to identify bruxism. Will monitor growth and eruption patterns for children to detect and negate future bruxism issues. The dental team can spot signs of bruxism during periodic oral tissue exams. Regular visits for early intervention and diagnosis will be most beneficial before too much damage has occurred.
Conclusion
Bruxism can be multi-factorial, with no one factor to identify as the major trigger. This disorder can be difficult to diagnose in patients of all ages because of the variety of symptoms and overlap with other conditions. It can create challenges in applying effective comprehensive management.16 Diagnosing bruxism requires a careful process of assessment that incorporates questionnaires, history taking and radiographic and visual examination. Treatments may include a home care course, use of a mouth guard and prescription medications. Early diagnosis and treatment of bruxism and grinding is key to reducing extensive and harmful results.
REFERENCES
1. BrainCoreTherapy of New York. Awake Bruxism versus Sleeping Bruxism. Accessed August 1, 2016.
2. The Academy of Oral Medicine (AAOM). Tooth Clenching or Grinding. Accessed August 1, 2016.
3. Dyett L. Consumer Guide to Dentistry. Teeth Grinding (Bruxism): What’s Behind the Grind? Accessed August 1, 2016.
4. Paesani D, Restrepo C, Barreiro M, et al. Bruxism theory and practice. Quintessence Publishing. 2010. Accessed August 1, 2016.
5. Ramfjord S, Ash Jr M. Occlusion. 2nd Edition. W.B. Saunders Company, 1971. 115-24, 127.
6. Thaller JL, Rosen G, Saltzman S. Study of the relationship of frustration and anxiety to bruxism. J Periodontol. 1967 May-Jun;38(3):193-7.
7. Mosby’s Dental Dictionary. St. Louis, MO: Mosby, 2014. 1,60,92.
8. Ilovar S, Zolger D, Castrillon E, et al. Biofeedback for treatment of awake and sleep bruxism in adults: systematic review protocol. Syst Rev. 2014 May 2;3:42. doi: 10.1186/2046-4053-3-42.
9. Lavigne GJ, Huynh N, Kato T, et al. Genesis of sleep bruxism: motor and autonomic-cardiac interactions. Arch Oral Biol. 2007 Apr;52(4):381-4. Epub 2007 Feb 20.
10. Rouse JS. The Bruxism Triad: Sleep bruxism, sleep disturbance, and sleep-related GERD. Inside Dentistry Continuing Education. 2010 May:32-44. Accessed August 1, 2016.
11. Restrepo CC, Vásquez LM, Alvarez M, et al. Personality traits and temporomandibular disorders in a group of children with bruxing behaviour. J Oral Rehabil. 2008 Aug;35(8):585-93. doi: 10.1111/j.1365-2842.2007.01838.x. Epub 2008 Apr 15.
12. van Goozen SH, Fairchild G, Snoek H, et al. The evidence for a neurobiological model of childhood antisocial behavior. Psychol Bull. 2007 Jan;133(1):149-82.
13. Vernallis FF. Teeth-grinding: some relationships to anxiety, hostility, and hyperactivity. J Clin Psychol. 1955 Oct;11(4):389-91. Accessed August 1, 2016.
14. Medical Marijuana. Cannabinoids Alleviate Symptoms of Bruxism. Accessed August 1, 2016.
15. Carvalho AL, Cury AA, Garcia RC. Prevalence of bruxism and emotional stress and the association between them in Brazilian police officers. Braz Oral Res. 2008 Jan-Mar;22(1):31-5.
16. SlideShare. Hamdan BA. Bruxism, An Overview and Management. Accessed August 1, 2016.
17. MedicineNet.com Teeth Grinding (Bruxism) Index. Accessed August 1, 2016.
18. The Bruxism Association. Symptoms of Bruxism. Accessed August 1, 2016.
19. Reis HJ, Guatimosim C, Paquet M, et al. Neuro-transmitters in the central nervous system & their implication in learning and memory processes. Curr Med Chem. 2009;16(7):796-840.
20. Bader GG, Kampe T, Tagdae T, et al. Descriptive physiological data on a sleep bruxism population. Sleep. 1997 Nov;20(11):982-90.
21. Lynch CD, McConnell RJ. The cracked tooth syndrome. J Can Dent Assoc. 2002 Sep;68(8):470-5.
22. National Sleep Foundation.Teeth Grinding. Accessed August 1, 2016.
23. National Institute of Mental Health (NIHM). Attention Deficit Hyperactivity Disorder. Last Revised March 2016. Accessed August 1, 2016.
24. Cohen-Zion M, Ancoli-Israel S. Sleep in children with attention-deficit hyperactivity disorder (ADHD): a review of naturalistic and stimulant intervention studies. Sleep Med Rev. 2004 Oct;8(5):379-402.
25. autismspeaks.org Accessed August 1, 2016.
26. MyChild at CerebralPalsy.org Accessed August 1, 2016.
27. National Alliance on Mental Illness (NAMI). Depression. Accessed August 1, 2016.
28. National Down Syndrome Society (NDSS). Dental Issues & Down Syndrome. Accessed August 1, 2016.
29. Friedland B, Manschreck TC. Compulsive bruxism: How to protect your patients’ teeth. Current Psychiatry. 2009 Mar;8(3). Accessed August 1, 2016.
30. Psychology Today. Obsessive Compulsive Disorder. Accessed August 1, 2016.
31. Parkinson’s Disease Foundation. Noble JM. Dental Health and Parkinson’s Disease. Accessed August 1, 2016.
32. Ohayon MM, Li KK, Guilleminault C. Risk factors for sleep bruxism in the general population. Chest. 2001 Jan;119(1):53-61.
33. Lavigne G, Palla S. Transient morning headache: recognizing the role of sleep bruxism and sleep-disordered breathing. J Am Dent Assoc. 2010 Mar;141(3):297-9.
34. Griffith HW, Moore SW. Complete guide to prescription & nonprescription drugs. New York, NY 2015 ed. 548-9, 708-9.
35. Davies SJ, Gray RJ, Linden GJ, James JA. Occlusal considerations in periodontics. Br Dent J. 2001 Dec 8;191(11):597-604.
36. Schuurs A. Pathology of the Hard Dental Tissues. New York, NY John Wiley & Sons 2012. 200- 204. Accessed August 1, 2016.
37. RDH magazine. Wall RT. The Clues behind bruxism. Accessed August 1, 2016.
38. Lavigne GJ, Khoury S, Abe S, et al. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008 Jul;35(7):476-94. doi: 10.1111/j.1365-2842.2008.01881.x.
39. Stuart A. Greene, DDS. QualityDentistry. Bruxism Night Grinding. Accessed August 1, 2016.
40. Gottleib B. Histologic considerations of the supporting tissues of the teeth. J Am Dent Assoc. 1943 Dec 30;(23):1872-83.
41. Orban B, Wentz F, Everett F, et al. Periodontics a concept–theory and practice. C.V. Mosby Company St. Louis. 1958. 476-82.
42. Collins Dentistry and Aesthetics. Exostosis – What It Is and How to Fix It. Accessed August 1, 2016.
43. Pain Science.com. Ingraham P. Massage Therapy for Bruxism, Jaw Clenching, and TMJ Syndrome: Perfect Spot No. 7, the masseter muscle of the jaw. Updated November 6, 2015. Accessed August 1, 2016.
44. The Washington Post. Janzito C. Health & Science. What Does Determination Sound Like? Could it be the Noise of Grinding Teeth? February 9, 2015. Accessed August 1, 2016.
45. Nissani M. A bibliographical survey of bruxism with special emphasis on non-traditional treatment modalities. J Oral Sci. 2001 Jun;43(2):73-83.
46. Bender SD. Headache, Temporomandibular Disorders, and Bruxism: Uncovering Connections. Practical Neurology. Jan/Feb 2013 21-24. Accessed August 1, 2016.
47. The TMJ Clinic. Causes. Accessed August 1, 2016.
48. Scident Family Dental Clinic. Clenching and Grinding Bruxism. Accessed August 1, 2016.
49. DeLany J. TMJ: Self-Care for Your Masseter. MassageToday July 2010;10(7). Accessed August 1, 2016.
50. Berlin R, Dessner L. Bruxism and chronic headache. Lancet. 1960 Aug 6;2(7145):289-91.
51. The Migraine Trust. Jaw tension in migraine and other headache disorders. Accessed August 1, 2016.
52. Symptoms, Signs, and Consequences of Bruxism. Accessed August 1, 2016.
53. Mayo Clinic. Diseases and Conditions. Bruxism (teeth grinding). Accessed August 1, 2016.
54. Cawson RA, Porter S, Odell EW. Cawson’s essentials of oral pathology and oral medicine. 7th edition London, UK. Churchill Livingstone 2002. 6,364,366,566.
55. Massachusetts Dental Society (MDS). Breaking the Habit of the Daily Grind. Accessed August 1, 2016.
56. Psychology Today. Borigini M. Getting to the Crux of Bruxism: Chomping at the Bit. Posted January 21, 2010. Accessed August 1, 2016.
57. FDA. Pergolide (marketed as Permax) Information. Accessed August 1, 2016.
58. CT Acupuncture Center. Clenched? Acupuncture Relieves Bruxism. Accessed August 1, 2016.
59. Gorski D. Does massage therapy decrease inflammation and stimulate mitochondrial growth? An intriguing study oversold. Posted February 13, 2012. Accessed August 1, 2016.
60. Medscape. Burgess J, Meyers AD. Bruxism Management. Accessed August 1, 2016.
61. Persaud R, Garas G, Silva S, et al. An evidence-based review of botulinum toxin (Botox) applications in non-cosmetic head and neck conditions. JRSM Short Rep. 2013 Feb;4(2):10. doi: 10.1177/2042533312472115. Epub 2013 Feb 12.
62. The Dr. Oz Show. Curatola GP. Are You a Grinder? Posted March 29, 2011. Accessed August 1, 2016.
ABOUT THE AUTHOR
Lara James, RDH, graduated from Portland Community College in 2004 with an AAS in Dental Hygiene. She has practiced for the last 11 years in private practice and recently added corporation dentistry to her career.