You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Plaque has long been associated with periodontal problems and, to a lesser extent, caries related to the bacteria contained within it. Oral bacteria, especially those contained in plaque, were long ignored for any affects outside the oral cavity. Yet, research has been accumulating that directly indicates a link between oral health and systemic disease, with the American Dental Association reporting 200 possible connections between systemic diseases and oral health.1
Poor oral hygiene resulting in worsening periodontal conditions locally within periodontal pockets can have negative repercussions throughout the entire body. Harmful microorganisms are always present in periodontal disease, and specific patients are predisposed to harboring these oral organisms, increasing their health risks. Accumulating evidence links periodontal disease and chronic oral inflammation to multiple health conditions, including cardiovascular and renal issues, diabetes, osteoporosis, and pulmonary disorders. With this research in mind, plaque has been recognized as a more complex environment than previously understood and has been re-termed “oral biofilm.”
What Is an Oral Biofilm?
Plaque is a community of microorganisms found on the tooth surface or within the sulcus (periodontal pocket) that are embedded in a matrix of polymers of host and bacterial origin. This is a more complex bioenvironment then previously recognized and, therefore, has been re-termed “biofilm.”2,3 Typically, more than 700 different species of bacteria naturally reside in the mouth. Most are considered innocuous, but some of these microorganisms have been identified as pathogenic. The mouth is the perfect incubator for bacteria, which can double in number in a few hours if left undisturbed. As bacteria increase in number, they quickly create an intricate network of protective layers (ie, matrix) and channels that develop into a biofilm and become a major cause of periodontal disease.
Bacteria in biofilms are less susceptible to antimicrobial agents, either locally applied or systemically administered. It has been long demonstrated that these microbial communities can display enhanced pathogenicity (pathogenic synergism).4,5 Additionally, the structure of the biofilm might restrict penetration of antimicrobial agents, while bacteria growing on a surface (planktonic) are susceptible to antimicrobial agents.6 The aggregated bacteria work together as a community, producing specific proteins and enzymes by way of quorum sensing, utilizing oral fluids as the vector for transmission.7 Bacteria in these oral environments have evolved as part of multispecies biofilms and may require interaction with other bacterial species to grow, forming complex bioenvironments.8
Bacteria in the biofilm are able to regulate numerous processes via quorum sensing. Quorum sensing is a cell-to-cell communication mechanism that synchronizes gene expression in the biofilm in reaction to the density of the cell population.9 This includes secreting specific enzymes to activate or deactivate the genes of other bacteria. These bacterial byproducts provoke an immune response from the host, which recruits white blood cells (WBCs) to the site to kill the invading bacteria, resulting in localized inflammation in the surrounding gingiva. Using quorum sensing, the bacteria can confuse the defending WBCs chemotactically by releasing chemicals into the local environment, rendering the immune response ineffective. Because WBCs have a 3-day lifecycle, if they do not engulf a bacterium and destroy it within that timeframe, they lyse and die.10 Thus, components within the WBCs that were intended to kill the bacteria are now available to damage the very tissue they were meant to protect, contributing to periodontal bone loss and a deepening of the pockets and inflammation.11
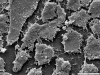
The composition of the bacterial community in the biofilm is diverse, with variations in the many species being detected and differing from site to site in the same patient (Figure 1). Once formed, the species composition at a site is characterized by a degree of stability among the component species due to a balance between synergism and antagonism.12
Formation of the biofilm involves a series of steps beginning with the initial colonization of the pellicle and ending with a complex formation of a mature biofilm. Biofilms exist on a variety of tooth surfaces, including fissures, smooth surfaces, and within the gingival sulcus; they are, however, most likely to be seen in their mature state in the periodontal pockets, which provide protection from removal by the patient via homecare.13,14 As the biofilm matures, the microbial composition changes from one that is primarily gram-positive and streptococcus-rich to a structure filled with gram-negative anaerobes.15
The first step in biofilm development is adsorption of host and bacterial molecules to the tooth surface (Figure 2). The resulting pellicle acts like an adhesive, causing bacteria to adhere to the tooth surface. This directly influences the initial microbial colonization, and additional bacteria continue to adsorb to the tooth surface. Initially, this consists of mostly gram-positive cocci bacteria (Streptococcus mutans, Streptococcus mitis, Streptococcus sanguis, Streptococcus oralis, Rothia dentocariosa, and Staphylococcus epidermidis), followed by some gram-positive rods and filaments (Actinomyces viscosus, Actinomyces israelis, Actinomyces gerencseriae, and Corynebacterium species) and a very small number of gram-negative cocci. Veillonella parvula and Neisseria species, which make up some of the gram-negative cocci, are aerobes or facultative aerobes. This early biofilm is able to withstand frequent mechanisms of the oral bacterial removal such as chewing, swallowing, and salivary fluid flow. These early colonizers are also able to survive in the high oxygen concentrations present in the oral cavity. Always present orally, this initial biofilm forms immediately after cleaning.
Co-adhesion of subsequent bacterial colonizers to the initial biofilm continues to involve specific interactions between bacterial receptors. These interactions build up the biofilm, creating a more complex and diverse environment. These diverse bacterial species create synergistic and antagonistic biochemical interactions among the colonies’ inhabitants. This may contribute metabolically to other bacteria that are located physically close to them. When obligate aerobes and anaerobes are involved in co-adhesion, these interactions can ensure the survival of the anaerobic bacteria in the oxygen-rich oral cavity. The bacteria continue to divide until a 3-dimensional mixed-culture biofilm forms that is specially and functionally organized. Polymer production causes development of an extracellular matrix. This matrix is a key structural aspect of the biofilm offering the inhabitants protection from external factors. As the biofilm thickens and becomes more mature, those anaerobic bacteria are able live deeper within the biofilm, further protecting them from the oxygen-rich environment within the oral cavity.
The Systemic Connection
Harmful strains of bacteria in the oral biofilm can enter the bloodstream during the inflammatory response and travel to other areas of the body, exerting a distant systemic effect that has been linked to numerous diseases. Increasing evidence indicates patients with periodontal disease have a much higher risk of developing cardiovascular and other systemic issues than individuals who take preventive measures to eliminate and control the biofilm in their mouth.1
Cardiovascular Disease
Cardiovascular disease (CVD) is an umbrella term for heart and blood vessel conditions such as atherosclerosis, coronary heart disease, stroke, and myocardial infarction. CVD is the result of a complex set of genetic and environmental factors.16 Genetic factors include age, lipid metabolism, obesity, hypertension, and diabetes. Environmental risk factors also play a key role and include socioeconomic status, exercise, stress, diet, smoking, and chronic infections. Classic risk factors such as hypertension, hypercholesterolemia, and cigarette smoking may only account for one-half to two-thirds of the incidence of CVD.17 There is increasing evidence linking chronic infection and inflammation to CVD with biofilm as a predisposing factor.18,19
The connection between oral bacteria and cardiac disease is not a recent development in the literature. Oral bacteria, specifically Streptococcus mutans (cariogenic) and Porphyromonas gingivalis (periodontitis), induce platelet aggregation, leading to thrombus formation.20 One or more periodontal pathogens as reported in the literature are found in 42% of atheromas in patients with severe periodontal disease.21 It has been reported that P gingivalis actively can adhere to and invade fetal bovine heart endothelial cells and aortic endothelial cells.22 Additionally, a 14-year study found patients with periodontal disease had a 25% higher risk to develop CVD than their healthy counterparts.23 Men younger than 50 years with periodontal disease demonstrated 72% more risk to develop CVD. Moreover, periodontal disease increased risk for both fatal and nonfatal strokes two-fold.24 Despite the strong evidence of an association between periodontal disease and CVD, it is unknown if it is a direct or causal relationship.
Periodontal disease releases bacteria that may enter the circulation, invading the heart and vascular tissue, causing harmful effects. People with higher levels of bacteria in their mouth tend to have thicker carotid arteries, an indicator of CVD.25 Bacteria near diseased gingiva appears to induce clumping of blood platelets, which can then cause the clotting and blockages that can lead to heart attacks or strokes. The body’s response to periodontal infection includes production of inflammatory mediators, which travel through the circulatory system and may cause harmful effects on the heart and blood vessels. Inflammatory mediators such as lipoprotein and triglycerides are significantly higher in patients with periodontitis than in control groups.26 Increased levels of C-reactive protein, a biomarker for inflammation associated with periodontitis, shows increased clotting, which is associated with an elevated risk of heart disease.27 The emergence of periodontal disease as a potential risk factor for CVD is leading to a convergence in oral and medical care. Proper management of oral health may very well be key to prevention of cardiac disease or worsening of existing heart conditions.
Chronic Kidney Diseases
CVD and chronic kidney disease (CKD) share many risk factors, with periodontal inflammation linked to the development of kidney disease.28 Pathogens found in oral biofilms have been shown to have the ability to adhere to and invade coronary endothelial cells, leading to atheroma formation and impaired vasculature relaxation. Similar effects are noted within the vasculature of the kidney.29 Symptoms of diminishing kidney function are nonspecific and may include feeling generally unwell and experiencing a reduced appetite. CKD, identified by increased levels of blood creatinine, indicates a falling glomerular filtration rate and decreased kidney filtration of waste products.
The most common causes of CKD are diabetes mellitus, hypertension, and glomerulonephritis, which together cause approximately 75% of all adult cases.30 Patients with CKD are characterized by a few well-established risk factors of periodontal disease, including poor oral hygiene and diabetes.31 A strong correlation appears to exist between patients on dialysis and the high number of patients suffering from gingivitis (46%) and severe periodontitis (35%).32 The correlation appears to be bidirectional, as patients with CKD have higher prevalence of periodontal disease.
Diabetes
A significant public health problem, diabetes affects 29.1 million patients (9.3% of the US population), with an estimated 8.1 million (27.8%) patients going undiagnosed.33 Those with diabetes have twice the risk for periodontal disease of those without the metabolic disorder. In addition, periodontal disease is more prevalent, progresses more rapidly, and is often more severe in patients with type I or type II diabetes.34,35
Periodontal disease has been classified as the sixth most common complication of diabetes and is a strong, well-established risk factor for severe periodontal disease. Patients with periodontal infections have worse glycemic control over time and, thus, have greater difficulty managing their diabetes. Treatment of periodontitis appears to improve glycemic control.36 Therefore, control of the periodontal infection and associated biofilm should be part of the standard treatment for a diabetic patient.
Pulmonary Disease
Periodontal biofilm is a reservoir of bacteria and a source of lower-airway infections, especially in older patients or those who are debilitated. Oral biofilm can inoculate the respiratory tract when aspirated. Severity of the disease is correlated with the pathogenicity of the bacteria in the biofilm. Periodontal pathogens and cariogenic bacteria increase risk factors for aspiration pneumonia.
The highest-risk patients for respiratory infection (bronchitis and pneumonia) are medically compromised patients with or without respiratory disease who are unable to perform adequate oral homecare. Evaluation of 328 articles published over an 11-year period reported linking oral hygiene to oral healthcare–associated pneumonia or respiratory tract infection in elderly people. The authors reported, “There is good evidence that mechanical oral hygiene practices reduce the progression or occurrence of respiratory diseases in high-risk elderly people in nursing homes or hospitals. Mechanical oral hygiene practices may prevent the death of about 1 in 10 elderly residents of nursing homes from healthcare-associated pneumonia.”37 Proper oral homecare is critical in preventing these oral infections by minimizing the potential of aspirating biofilm into the pulmonary system. One author reported, “Oral hygiene intervention significantly reduced occurrence of pneumonia in institutionalized subjects.”38 Frequent tooth brushing and preoperative use of 0.12% chlorhexidine mouthrinse or gel reduced nosocomial respiratory tract infections.39 Therefore, placing all elderly patients on chlorhexidine daily rinses as a preventive measure may be recommended to aid in preventing potential aspiration pneumonia. It has also been demonstrated that use of low-concentration peroxides in custom trays has a positive affect on oral biofilms, thus reducing the bacterial load and decreasing pathogenic material that may be aspirated. This may be a more predictable approach in elderly patients who lack manual dexterity to perform oral homecare with a toothbrush.
Patients who are elderly tend to also be denture wearers (higher incidence compared to younger populations) and can be susceptible to aspiration of biofilm growing on the denture. Because this patient population has decreased immune systems and an increase in systemic issues, they are particularly susceptible to pulmonary infections, which can be induced via the bacteria within the biofilm attached to the denture. This becomes more problematic in the nursing home setting or for those patients unable to care for their own dentures due to either physical or mental limitations. Immersion in a peroxide-based cleanser solution effectively reduces the quantity of microorganisms surviving on dentures.40 Those patients who are unable to mechanically scrub their dentures would benefit from immersion of the denture in a peroxide solution, such as found over the counter in any drug or food store pharmacy. Unlike other solutions that have been recommended, such as diluted sodium hypochlorite (NaOCl) (ie, bleach), the peroxide appears to have no negative effects to the denture base, its teeth, or soft liners present.41,42 This can be performed daily by nursing staff or homecare aids to help prevent potential aspiration of biofilm in this compromised population.
Prostate Disease
Prostate-specific antigen (PSA), an enzyme created in the prostate normally secreted in very small quantities, has been reported to be secreted at much higher levels in men with periodontal disease.43 Inflammation of the prostate or when infection is present or affected by cancer demonstrates elevated PSA levels. Research has demonstrated that men with indicators of periodontal disease and prostatitis have higher levels of PSA than men who do not have periodontal disease.44 Elevated PSA levels are a classic indicator of prostate cancer.45
Colon Cancer
The link of colon cancer to an oral connection and periodontal disease via biofilm is just becoming known in recent years. The bacteria Fusobacterium nucleatum, found in the mouth and in periodontal biofilm, has a role in periodontal disease. This bacteria has also been shown to colonize the gut and attach to cells in the colon, triggering a sequence that can lead to colon cancer. It has been reported that patients with periodontal disease have much higher levels of F nucleatum then those with normal periodontal status.46,47 Although a possible association was found between oral infection and colon cancer, a cause-and-effect relationship has not been found. Published studies show how F nucleatum can speed the accumulation of cancer cells.48,49 Minimizing F nucleatum by controlling and managing oral biofilm may lower the risk for those who are at increased risk of developing colorectal cancer.
Pancreatic Cancer
While pancreatic cancer risk factors include cigarette smoking and chronic pancreatitis, the role of inflammation from periodontal disease may promote this cancer.50 Harvard School of Public Health and Dana-Farber Cancer Institute researchers found that periodontal disease may be associated with an increased risk of cancer of the pancreas. Additionally, research shows men with periodontal disease had a 63% higher risk of developing pancreatic cancer compared to those reporting no periodontal disease.51
Preterm Pregnancy
Evidence shows an association between the presence of periodontitis and preterm delivery and low-birth-weight infants. Biofilm inflammatory molecules can enter the circulatory system and cross the placenta to reach the fetal membranes and cause preterm delivery. Oral bacteria has been identified in fetal membranes. The inflammation of the periodontal tissues due to the formation of the biofilm increases dramatically in size and severity during the course of a normal pregnancy.52 Mechanisms have been suggested to explain how periodontal disease may influence preterm, low-birth-weight babies. Lipopolysaccharides from cell walls of periodontal pathogens can trigger production of prostaglandins; periodontal infection leads to release of these prostaglandins into the circulatory system. Translocation of these periodontal bacteria to the fetus occurs via the placenta, which stimulates the release of prostaglandins.53 These prostaglandins stimulate oxytocin production, which can initiate preterm labor and result in lower-birth-weight babies.
How Can Clinicians Better Manage Oral Biofilms?
Mechanical debridement of the periodontal pocket cannot remove all of the biofilm. This is because, despite patients’ best efforts, toothbrushes are ineffective more than 4 mm subgingival as their bristles simply don’t extend further than this distance into the pocket to mechanically contact the biofilm located at deeper depths. Similarly, oral irrigators do not enable irrigation to the bottom of pockets. For most patients, the sulcular environment is difficult to reach with brushing and flossing, making it virtually impossible to control oral biofilms by mechanical means alone, particularly because the bacteria grow and replicate so rapidly; regrowth of the biofilm occurs within 3 hours, resulting in a four-fold (400%) increase in biofilm mass54 (Figure 3). Post-cleaning biofilm redevelopment is more rapid and complex, exceeding pre-cleaning levels within 2 days.55,56
Because bacteria embedded in the biofilm are up to 1000-fold more resistant to antibiotics compared to planktonic bacteria,57 use of antibiotics either systemically or in oral rinses and site application are unable to eliminate or manage the biofilm bacteria adequately.58,59 This has implications both with natural teeth and regarding periodontal issues around dental implants leading to periimplantitis.60
Chlorhexidine has been reported to have an effect on young biofilms, but the bacteria in mature biofilms and nutrient-limited biofilms have been shown to be more resistant to its effects.61,62 Hydrogen peroxide (H2O2), on the other hand, has been documented as a very effective means of both eliminating the biofilm and preventing its reformation without bacterial resistance issues found with other site-specific treatment modalities. H2O2 has been documented to be used daily up to 6 years with no adverse effects or carcinogenic activity while showing a decrease in biofilm (plaque) and enhanced wound healing, improving gingival bleeding.63 Further, no allergic reactions have been reported and bacterial strains demonstrate no resistance. Functionally, H2O2 debrides the biofilm slime matrix and bacterial cell walls, essentially peeling the biofilm back layer by layer. This causes irreversible cleaving/converting of the amino acids in the protein chains of the bacteria in the biofilm, acting to break down the protein pellicle attaching the biofilm to the tooth surface and decreasing localized inflammation in the pocket by inhibiting IL-8 mRNA.64
Oxygen is required for successful wound healing due to increased demand of the reparative processes such as cell proliferation, bacterial defense, angiogenesis, and collagen synthesis.65 New cell growth requires oxygen, which induces the growth of new blood vessels. This increases flow of oxygenated blood to the wound, beginning the healing process. As healing progresses, new granulation tissue that is exposed to oxygen is better vascularized, leading to higher tensile strength collagen being formed during wound healing. Hyperbaric oxygen has been well documented to be bactericidal for anaerobic bacteria.66
H2O2 oxygenates the pocket, changing the environment from anaerobic to aerobic and creating a hyperbaric oxygen chamber in the sulcus to destroy the biofilm occupants. Additionally, neutrophils in the presence of H2O2 and chloride will produce ozone through the cholesterol ozonolysis process.67 Ozone has antimicrobial activity by oxidation of biomolecule precursors and microbial toxins that have been implicated in periodontal diseases, thus causing healing and tissue regeneration.68
Published studies have documented that the ideal concentration of hydrogen peroxide is 1.7%, which is effective in breaking down the biofilm and virtually eliminating any irritation issues reported with higher concentrations. A 10-minute exposure to a 1.7% H2O2 gel penetrates the biofilm slime matrix, debriding the bacterial cell walls within. Maintaining the peroxide in the periodontal pocket releases oxygen and changes the subgingival microenvironment, making survival of the anaerobic bacteria more difficult69,70 (Figure 4 and Figure 5). However, due to biofilm’s quick redevelopment capabilities, peroxide application needs to be part of the daily homecare routine in order to be effective.
Thus, a daily method is needed that is easy to use to enhance patient compliance, able to reach the depths of the pockets, and effective in breaking down biofilm while preventing it from rebuilding. The difficulty is in delivering the hydrogen peroxide to the depth of the pocket and keeping it there so it can assert its action on the biofilm for the requisite time to be effective. Fluid is produced in the sulcus/pocket as a natural process to flush bacteria and other items from this space. Unfortunately, this also flushes any materials used to try to irrigate the pockets. Normal crevicular fluid is replaced 40 times per hour, making spontaneous inflow in a pocket virtually impossible. In inflamed tissue, this flow may increase up to 30 times normal flow.71 This constant outflow of crevicular fluid leads to an extremely fast clearance of any topically applied product into the pocket.72 Since the peroxide gel requires sufficient contact time, placing it into the pocket with an irrigation syringe is ineffective due to the crevicular flow; it would also be time-consuming for the patient, which would add to compliance being an issue. Customized trays designed to deliver a solution such as hydrogen peroxide deep into periodontal pockets against the force of crevicular fluid flow have been successfully utilized. If the tray with the peroxide is worn for 15 minutes, the peroxide is shown to reach the bottom of deep pockets >7 mm.69,73
Besides natural teeth, biofilms can be associated with titanium dental implants. Because the attachment between the gingiva and titanium is weaker than that found around healthy natural teeth due to connective tissue fiber orientation, inflammation related to biofilms can progress more rapidly. Removal of the biofilm around these implants and any exposed threads must be done on a daily basis. Peroxide in concentrations of 1.7% has not been shown to affect the implant surface.74 Additionally, it has demonstrated to be an effective bacteriocidal agent against any bacteria adhered to the titanium surface.75
Conclusion
Today, plaque—now called biofilm—is recognized as a much more complex material functioning through coordination of bacteria within a protective slime matrix. Extensive data and research has demonstrated that the oral biofilm causing periodontal disease has distant systemic effects and has been connected to numerous medical conditions. The health conditions examined here are not the only ones associated with periodontal disease, and a full review of all conditions was beyond the scope of this article. Periodontal treatment is evolving to be a major component of full-body medical care, and controlling the associated biofilm yields better overall systemic health. Yet, homecare is critical to biofilm management due to the rapid rebuilding of the biofilm following scaling and root planing. As discussed, brushing, flossing, and oral irrigation are ineffective because of patient noncompliance and patients’ inability to effectively reach the bottom of the pockets. Therefore, careful consideration must be given to what clinicians recommend to patients, which must both be effective and require minimal patient effort.
ABOUT THE AUTHOR
Gregori M. Kurtzman, DDS, MAGD
Private Practice Silver Spring, Maryland
REFERENCES
1. Loos BG. Systemic effects of periodontitis. Int J Dent Hyg.2006;4(suppl 1):34-38.
2. Marsh PD. Dental plaque as a microbial biofilm. Caries Res. 2004;38(3):204-211.
3. Socransky SS, Haffajee AD. Dental biofilms: difficult therapeutic targets. Periodontol 2000. 2002;28:12-55.
4. van Steenbergen TJ, van Winkelhoff AJ, de Graaff J. Pathogenic synergy: mixed infections in the oral cavity. Antonie Van Leeuwenhoek. 1984;50(5-6):789-798.
5. Kanwar IL, Sah AK, Suresh PK. Biofilm-mediated antibiotic-resistant oral bacterial infections: mechanism and combat strategies. Curr Pharm Des. 2016 Nov 24. [Epub ahead of print]
6. Gilbert P, Maira-Litran T, McBain AJ, et al. The physiology and collective recalcitrance of microbial biofilm communities. Adv Microb Physiol. 2002;46:202-256.
7. Hojo K, Nagaoka S, Ohshima T, Maeda N. Bacterial interactions in dental biofilm development. J Dent Res. 2009;88(11):982-990.
8. Wade W, Thompson H, Rybalka A, Vartoukian S. Uncultured members of the oral microbiome. J Calif Dent Assoc. 2016;44(7):447-456.
9. Suntharalingam P, Cvitkovitch DG. Quorum sensing in streptococcal biofilm formation. Trends Microbiol. 2005;13(1):3-6.
10. Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol. 2013(13):159-175.
11. White blood cell enzyme contributes to inflammation and obesity. Medical Xpress website. April 2, 2013. http://medicalxpress.com/news/2013-04-white-blood-cell-enzyme-contributes.html. Accessed April 4, 2017.12. Marsh PD, Featherstone A, McKee AS, et al. A microbiological study of early caries of approximal surfaces in schoolchildren. J Dent Res. 1989;68(7):1151-1154.
13. Marsh PD. Dental plaque as a biofilm and a microbial community - implications for health and disease. BMC Oral Health. 2006;6(suppl 1):S14.
14. Sbordone L, Bortolaia C. Oral microbial biofilms and plaque-related diseases: microbial communities and their role in the shift from oral health to disease. Clin Oral Investig. 2003;7(4):181-188.
15. Xie H, Cook GS, Costerton JW, et al. Intergeneric communication in dental plaque biofilms. J Bacteriol. 2000;182(24):7067-7069.
16. Herzberg MC, Weyer MW. Dental plaque, platelets, and cardiovascular diseases. Ann Periodontol. 1998;3(1):151-160.
17. Scannapieco FA. Position paper of The American Academy of Periodontology: periodontal disease as a potential risk factor for systemic diseases. J Periodontol. 1998;69(7):841-850.
18. Valtonen VV. Infection as a risk factor for infarction and atherosclerosis. Ann Med. 1991;23(5):539-543.
19. Syrjänen J. Vascular diseases and oral infections. J Clin Periodontol. 1990;17(7 pt 2):497-500.
20. Nomura R, Otsugu M, Naka S, et al. Contribution of the interaction of Streptococcus mutans serotype k strains with fibrinogen to the pathogenicity of infective endocarditis. Infect Immun. 2014;82(12):5223-5234.
21. Haraszthy VI, Zambon JJ, Trevisan M, et al. Identification of pathogens in atheromatous plaques [abstract 273]. J Dent Res. 1998;77(spec iss B):666.
22. Deshpande RG, Khan MB, Genco CA. Invasion of aortic and heart endothelial cells by Porphyromonas gingivalis. Infect Immun. 1998;66(11):5337-5343.
23. Dhadse P, Gattani D, Mishra R. The link between periodontal disease and cardiovascular disease: How far we have come in last two decades? J Indian Soc Periodontol. 2010;14(3):148-154.
24. Persson GR, Imfeld T. Periodontitis and cardiovascular disease. Ther Umsch. 2008;65(2):121-126.
25. Desvarieux M, Demmer RT, Rundek T, et al. Periodontal microbiota and carotid intima-media thickness: the Oral Infections and Vascular Disease Epidemiology Study (INVEST). Circulation. 2005;111(5):576-582.
26. Loesche WJ, Schork A, Terpenning MS, et al. The relationship between dental disease and cerebral vascular accident in elderly United States veterans. Ann Periodontol. 1998;3(1):161-174.
27. Wu T, Trevisan M, Genco RJ, et al. Examination of the relation between periodontal health status and cardiovascular risk factors: serum total and high density lipoprotein cholesterol, C-reactive protein, and plasma fibrinogen. Am J Epidemiol. 2000;151(3):273-282.
28. Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366(9499):1809-1820.
29. Bascones-Martínez A, Muñoz-Corcuera M, Noronha S, et al. Host defense mechanisms against bacterial aggression in periodontal disease: Basic mechanisms. Med Oral Patol Oral Cir Bucal. 2009;14(12):e680-e685.
30. Palmer BF. Management of hypertension in patients with chronic kidney disease and diabetes mellitus. Am J Med. 2008;121(8 suppl):S16-S22.
31. DePaola DP, ed. Periodontitis and renal disease. Colgate Oral Care Report. 2007;17(4).
32. Buhlin K, Bárány P, Heimbürger O, et al. Oral health and pro-inflammatory status in end-stage renal disease patients. Oral Health Prev Dent. 2007;5(3):235-244.
33. National Diabetes Statistics Report, 2014. Centers for Disease Control and Prevention website. www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed April 5, 2017.
34. Stanko P, Izakovicova Holla L. Bidirectional association between diabetes mellitus and inflammatory periodontal disease. A review. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158(1):35-38.
35. Kim EK, Lee SG, Choi YH, et al. Association between diabetes-related factors and clinical periodontal parameters in type-2 diabetes mellitus. BMC Oral Health. 2013;13:64.
36. Taylor GW, Burt BA, Becker MP, et al. Severe periodontitis and risk for poor glycemic control in patients with non-insulin-dependent diabetes mellitus. J Periodontol. 1996;67(10 suppl):1085-1093.
37. Rosenblum R Jr. Oral hygiene can reduce the incidence of and death resulting from pneumonia and respiratory tract infection. J Am Dent Assoc. 2010;141(9):1117-1118.
38. Scannapieco FA, Bush RB, Paju S. Associations between periodontal disease and risk for nosocomial bacterial pneumonia and chronic obstructive pulmonary disease. A systematic review. Ann Periodontol. 2003;8(1):54-69.
39. Sjögren P, Nilsson E, Forsell M, et al. A systemic review of the preventive effect of oral hygiene on pneumonia and respiratory tract infection in elderly people in hospitals and nursing homes: effect estimates and methodological quality of randomized controlled trials. J Am Geriatr Soc. 2008;56(11):2124-2130.
40. Nishi Y, Seto K, Kamashita Y, et al. Survival of microorganisms on complete dentures following ultrasonic cleaning combined with immersion in peroxide-based cleanser solution. Gerodontology. 2014;31(3):202-209.
41. Pires CW, Fraga S, Beck AC, et al. Chemical Methods for Cleaning Conventional Dentures: What is the Best Antimicrobial Option? An In Vitro Study. OralHealth Prev Dent. 2017;15(1):73-77.
42. Paranhos HF, Silva-Lovato CH, Souza RF, et al. Effects of mechanical and chemical methods on denture biofilm accumulation. J Oral Rehabil. 2007;34(8):606-612.
43. Men’s sexual health may be linked to periodontal health. American Academy of Periodontology website. https://www.perio.org/consumer/erectile_dysfunction. Accessed April 5, 2017.
44. Joshi N, Bissada NF, Bodner D, et al. Association between periodontal disease and prostate-specific antigen levels in chronic prostatitis patients. J Periodontol. 2010;81(6):864-869.
45. Seymour RA. Is oral health a risk for malignant disease? Dent Update. 2010;37(5):279-283.
46. Han YW. Fusobacterium nucleatum: a commensal-turned pathogen. Curr Opin Microbiol. 2015;23:141-147.
47. Han YW, Wang X. Mobile microbiome: oral bacteria in extra-oral infections and inflammation. J Dent Res. 2013;92(6):485-491.
48. Leung A, Tsoi H, Yu J. Fusobacterium and Escherichia: models of colorectal cancer driven by microbiota and the utility of microbiota incolorectal cancer screening. Expert Rev Gastroenterol Hepatol. 2015;9(5):651-657.
49. Colucci F. An oral commensal associates with disease: chicken, egg, or red herring? Immunity. 2015;42(2):208-210.
50. Periodontal disease and pancreatic cancer linked. Medical News Today website. January 19, 2007. http://www.medicalnewstoday.com/releases/60977.php. Accessed April 5, 2017.
51. Michaud DS. Role of bacterial infections in pancreatic cancer. Carcinogenesis. 2013;34(10):2193-2197.
52. Silva de Araujo Figueiredo C, Gonçalves Carvalho Rosalem C, Costa Cantanhede AL, et al. Systemic alterations and their oral manifestations in pregnant women. J Obstet Gynaecol Res. 2017;43(1):16-22.
53. Lux J, Lavigne S. Your mouth – portal to your body. Probe. 2004;38(4):154-171.
54. Palmer RJ, Caldwell DE. A flowcell for the study of plaque removal and regrowth. J Micro Methods. 1995;24(2):171-182.
55. Teles FR, Teles RP, Sachdeo A. Comparison of microbial changes in early redeveloping biofilms on natural teeth and dentures. J Periodontol. 2012;83(9):1139-1148.
56. Teles FR, Teles RP, Uzel NG, et al. Early microbial succession in redeveloping dental biofilms in periodontal health and disease. J Periodontal Res. 2012;47(1):95-104.
57. Sauer K, Thatcher E, Northey R, Gutierrez AA. Neutral super-oxidised solutions are effective in killing P. aeruginosa biofilms. Biofouling. 2009;25(1):45-54.
58. Kouidhi B, Al Qurashi YM, Chaieb K. Drug resistance of bacterial dental biofilm and the potential use of natural compounds as alternative for prevention and treatment. Microb Pathog. 2015;80:39-49.
59. Rams TE, Degener JE, van Winkelhoff AJ. Antibiotic resistance in human chronic periodontitis microbiota. J Periodontol. 2014;85(1):160-169.
60. Rams TE, Degener JE, van Winkelhoff AJ. Antibiotic resistance in human peri-implantitis microbiota. Clin Oral Implants Res. 2014;25(1):82-90.
61. Shen Y, Stojicic S, Haapasalo M. Antimicrobial efficacy of chlorhexidine against bacteria in biofilms at different stages of development. J Endod. 2011;37(5):657-661.
62. Guggenheim B, Meier A. In vitro effect of chlorhexidine mouth rinses on polyspecies biofilms. Schweiz Monatsschr Zahnmed. 2011;121(5):432-441.
63. Marshall MV, Cancro LP, Fischman SL. Hydrogen peroxide: a review of its use in dentistry. J Periodontol. 1995;66(9):786-796.
64. Lekstrom-Himes JA, Kuhns DB, Alvord WG, Gallin JI. Inhibition of human neutrophil IL-8 production by hydrogen peroxide and dysregulation in chronic granulomatous disease. J Immunol. 2005;174(1):411-417.
65. Schreml S, Szeimies RM, Pranti L, et al. Oxygen in acute and chronic wound healing. Br J Dermatol. 2010;163(2):257-268.
66. Phillips J. The Wound Care Institute, Inc. for the Advancement of Wound Healing & Diabetic Footcare. Wound Care Institute Newsletter. Fall 1996.
67. Tomono S, Miyoshi N, Sato K, et al. Formation of cholesterol ozonolysis products through an ozone-free mechanism mediated by the myeloperoxidase-H2O2-chloride system. Biochem Biophys Res Commun. 2009;383(2):222-227.
68. Gupta G, Mansi B. Ozone therapy in periodontics. J Med Life. 2012;5(1):59-67.
69. Dunlap T, Keller DC, Marshall MV, et al. Subgingival delivery of oral debriding agents: a proof of concept. J Clin Dent. 2011;22(5):149-158.
70. Schaudinn C, et al. Manipulation of the microbial ecology of the periodontal pocket. World Dental. 2010;2(1):14-18.
71. Goodson JM. Gingival crevice fluid flow. Periodontol 2000. 2003;31:43-54.
72. Goodson JM, Offenbacher S, Farr DH, Hogan PE. Periodontal disease treatment by local drug delivery. J Periodontol. 1985;56(5):265-272.
73. Putt MS, Proskin HM. Custom tray application of peroxide gel as an adjunct to scaling and root planing in the treatment of periodontitis: a randomized, controlled three-month clinical trial. J Clin Dent. 2012;23(2):48-56.
74. Ntrouka V, Hoogenkamp M, Zaura E, van der Weijden F. The effect of chemotherapeutic agents on titanium-adherent biofilms. Clin Oral Implants Res. 2011;22(11):1227-1234.
75. Gosau M, Hahnel S, Schwarz F, et al. Effect of six different peri-implantitis disinfection methods on in vivo human oral biofilm. Clin Oral Implants Res. 2010;21(8):866-872.