You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The World Health Organization considers obesity to be a global epidemic.1 Data from the National Health and Nutrition Examination Survey (NHNES) from 2003-2004 indicate that in the United States 17% of children and adolescents are overweight, and 32% of adults are obese.2 These data also show that the overweight and obese populations are on the increase when compared to previous NHNES data from 1999-2000.2 There is a serious problem even among the very young, with 5% of 6-to-11-year-olds estimated to be severely obese.3
Obesity is a growing public health concern; obesity increases the risk of diabetes, heart disease, stroke, arthritis, and some types of cancer.4 Over the past 10 years in the United States the prevalence of obesity has increased, and weight discrimination also increased by 66%.5 Physicians and medical students have expressed less desire to help obese patients, and have labeled these patients as lazy, undisciplined, and unmotivated.5-7 Obese patients seeking healthcare who encounter negative attitudes and poor treatment from the healthcare providers have been shown to subsequently avoid preventive care,5 which in turn may adversely affect their health status.
Magliocca and colleagues employed a modified version of a questionnaire, used to measure medical student bias,8 to study both dental and dental hygiene students’ attitudes toward obesity.9 They found that both dental and dental hygiene students indicated negative attitudes toward obese patients.9 Approximately 30% of student respondents reported that obese patients were lazy, and 26% reported perceiving obese people as unmotivated and lacking will power. Also, 14% of the students reported feeling uncomfortable examining obese patients, and 17% lacked empathy toward obese patients.9
Additional data indicate that obesity bias is also present among those who study obesity and/or work with obese patients.10 Schwartz and colleagues surveyed attendees at an international obesity conference and found there to be a significant obesity bias, particularly among the women participating, regardless of the assumption that this population would be well-informed on the topic of obesity. This finding underscores the importance of evaluating for, and addressing bias within, the health professions including dental hygiene.
Biases are known to influence patient care in the medical setting,5-7 but it is unknown whether dental hygienists harbor or display biases toward obese patients. The research questions guiding this study are as follows: Do dental hygienists have biases toward obese patients? Are there differences in attitudes toward obesity among those with different self-reported body images? The purpose of this study is to explore dental hygienists’ attitudes toward the obese population and to determine whether there are differences in attitudes among those with different self-reported body images.
Methods
The study population was dental hygienists whose email addresses were in the database of the California Dental Hygienists’ Association (CDHA). Inclusion criteria included both members and nonmembers of CDHA. Potential participants received an email invitation to participate containing basic information on the purpose of the study, informed consent declaration, and a link to the online survey. Two follow-up emails were distributed after the initial invitation to participate was distributed; the first follow-up message was sent on the third week, and the second follow-up was sent on week eight.
The online survey consisted of two previously validated instruments adapted for use with dental hygienists. The first instrument was the Fat Phobia Scale, which consisted of 14 pairs of adjectives sometimes used to describe obese people.11 For each of the 14 pairs of adjectives, respondents selected a number (1 through 5) closest to the adjective that they felt best described their feelings and beliefs. The total score was added and divided by 14 to obtain a scoring range from 1 to 5. Scores below 2.5 indicate a neutral attitude about obese patients, scores between 2.5 and 4.3 indicate a mild bias, and scores of 4.4 or higher indicate a high level of obesity bias.
The second instrument that was used was the Anti-fat Attitudes Questionnaire (AFAQ), which evaluated respondents’ attitudes and behaviors related to obesity.12 Respondents selected one of nine Likert-like responses, ranging from very strongly agree to very strongly disagree. When frequencies (percentages) were calculated, four responses were merged for convenience in reporting, resulting in six categories of responses: very strongly and strongly agree, moderately and somewhat agree, moderately and somewhat disagree, and very strongly and strongly disagree.
The survey also included three items on demographic information and one item on body image, which asked respondents to self-identify as underweight, normal or average weight or overweight.
Qualtrics (Qualtrics, www.qualtrics.com) survey and research suite was used to calculate frequencies (percentages) of responses to each survey item and to conduct cross tabulations among variables. The percentages of responses for each level of agreement with statements from the AFAQ were analyzed, using a variation of the chi-square test, for significant differences among self-reported body images. A P-value equal to or less than P < .05 was considered statistically significant.
Results
The Institutional Review Board at the University of California, San Francisco approved this cross-sectional study. Of the 6,248 email addresses in the CDHA database, 518 dental hygienists opened the online survey, yielding a response rate of 8%. However, 90 of these respondents neglected to answer any questions, and the number of respondents per question varied greatly. Table 1 indicates that the majority of respondents were female, non-Hispanic White, and between 40 to 59 years of age.
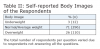
Respondents self-reported their body image in terms of three categories: underweight, normal or average weight, and overweight (Table 2). Most of the respondents reported normal or average weight.
The respondents’ assessments of their attitudes toward the obese population, based on responses to word pairs, are shown in Table 3. More than half (57%) of the Fat Phobia Scale word pair scores were higher than 2.50, which indicated a slight fat phobia. The mean of all word pair scores for the Fat Phobia Scale was 2.61. The “Likes food: Dislikes food” word pair had the lowest score or the least “fat Phobia” and the “Weak: Strong” word pair had the higher score or mild “fat phobia.”
Table 4 indicates the respondents’ levels of agreement with various statements from the AFAQ. The highest percentage (84%) of respondents’ agreement, which includes those responding “strongly to very strongly agree,” “somewhat to moderately agree,” and “agree,” was to the statement “People who weigh too much could lose at least some part of their weight through a little exercise.”
Three statements had significantly (P ≤ .05) different levels of agreement based on self-reported body image. Two of the statements were concerned with the respondent’s personal belief of one’s own body image, “I feel disgusted with myself when I gain weight” and “I worry about becoming fat.” Significantly more respondents of the overweight population agreed to these statements than those who reported themselves as underweight. The third statement demonstrating significance was regarding a respondent’s relationship with obese persons, “Fat people make me somewhat uncomfortable.” This statement displayed a strong disagreement from the respondents of the self-identified overweight population compared to those identifying as underweight.
Most of the respondents (93%) reported that they had not completed a continuing education course related to obesity. The few that had taken courses indicated that the course was offered at dental scientific sessions or through scientific journals.
Discussion
In our study we assessed the attitudes of dental hygienists toward the obese population using two established survey instruments: The Fat Phobia Scale11 and the Anti-fat Attitude Questionnaire.12 Participating dental hygienists were shown to report mildly negative attitudes or bias toward the obese population when the two implemented measures were considered in total. More than half of the scores on the Fat Phobia Scale were higher than 2.5, indicating a slight fat phobia. However, compared to the Fat Phobia Scale score of 3.413 reported for the study involving registered dieticians, registered dental hygienists were found to report more positive attitudes toward the obese population.
The results of the Anti-fat Attitude Questionnaire suggest that the majority of the respondents presented a positive attitude toward the obese population. However, the levels of agreement with three of the statements on the Fat Phobia Scale, “I feel disgusted with myself when I gain weight,” “I worry about becoming fat,” and “Fat people make me somewhat uncomfortable,” demonstrated statistically significant differences of reported attitudes between those who self-reported as overweight, normal/average weight, or underweight.
When the respondents were asked to indicate their levels of agreement with various statements designed to detect the “presence of bias and negative attitude” on the Anti-fat Attitude Questionnaire, the majority of the respondents did not present a negative attitude toward the obese population. In a study by Magliocca et al, when the dental and dental hygiene students were asked to respond to the statement, “Overweight people tend to be lazier than normal weight people,” 30% of both dental and dental hygiene students agreed with the statement, and 40% disagreed and 30% were neutral.9 Compared to the respondents in the current study, in which 24% agreed that overweight people are lazy, 16% disagreed, and 60% felt neutral. It was further reported that 14% of the dental and dental hygiene students felt uncomfortable when examining an obese patient9; however, only 2.3% of the respondents in our study reported feeling uncomfortable with the obese population.
In a study by Walter and colleagues, the Anti-fat Attitudes questionnaire12 was used to survey undergraduate and graduate students enrolled in a religiously affiliated university.14 The participants indicated that 10% felt uncomfortable interacting with an obese person.14 Over 50% of the participants’ responses to statements, self-reflective of one’s own weight gain or weight concern, ranked between 7-9 on the Anti-fat Attitudes scale indicating a negative attitude.14 Participants were generally more critical about their own personal weight gain, and less critical about others who gain weight.14
There is a similarity in findings from the Walter et al study and the current study. In both studies, participants who ranked highest for the statement, “People who weigh too much could lose at least some part of their weight through a little exercise,” were found to have the highest indication of negative bias towards the obese population.14 The bias reported may indicate either adherence to a stereotype or lack of knowledge about the obese population. Many people may make the assumption that what an overweight person might need to do to lose weight is to exercise rather than investigating further into the etiology of a patient’s weight gain through their health history, cultural background, nutrition or other variables.
Obesity bias in dental hygienists should be explored in future studies. Raising awareness of negative attitudes toward obesity population for both dental hygiene students and dental hygienists in practice is needed so that all patients receive the best comprehensive care available. It is necessary to address the unconscious bias that one can hold in addition to meeting educational needs in order to prepare dental hygienists to meet the needs of obese patients. One suggestion is to encourage dental hygienists to investigate their own unconscious biases through resources such as Project Implicit, a research and education project on implicit bias ongoing in collaboration with several US universities. In addition to examining personal bias dental hygienists can also participate in general diversity training, particularly those that include persons of size as a diversity marker.
More extensive education relating to the additional health concerns that present with obesity and the role of the dental hygienists in addressing these concerns is recommended. Research done by Kading and colleagues supports this recommendation15; North Carolina dental hygienists reported that they lacked the training on how to address specific topics, which may improve the overall health of their obese patients. Integrating obesity health concerns into current curricula is one means of addressing this need. There are content areas already taught that should be evaluated for possible refinement and inclusion of obesity content; for example, when addressing diabetes and other metabolic disorders. Professional training must follow population changes. It is clear that the trend toward obesity is still rising and will necessitate greater expertise among dental hygienists in managing the oral health and supporting the total health of obese patients. On the other hand, dental hygienists need to be aware of their limited education in addressing the complications of obesity that require the expertise of a nutritionist. Determining dental hygienists’ needs and practices of referrals to a nutritionist would be an interesting study.
Being obese increases the likelihood of a patient having associated medical and oral health problems. Recent studies have suggested obesity as a risk factor for periodontal disease.16 One study found that body mass index was positively and significantly associated with severity of periodontal attachment loss.17 This relationship may result from the fat cells in the abdominal adipose tissue secreting inflammatory factors, such as the cytokine tumor necrosis factor-alpha (TNF-α), into the plasma. The circulating inflammatory factors would increase systemic inflammation and, thus, promote the risk for periodontal inflammation. To maintain the obese individual’s periodontal health, the dental hygienist has an important role in emphasizing preventive oral care.
Another health message for the patient-centered interaction would be a discussion of the patient’s consumption of high sugar foods and drinks that increase the risk of dental caries, as well as contribute to obesity. Discussion of dietary versus nutritional counseling may be an important change to consider within the profession. Dental hygienists are commonly educated in dietary counseling as related to oral health and caries prevention. Enriching and expanding that curricular content may be a means of addressing the needs of obese patients. For example, providing greater content of evidence-based nutrition information related to obesity and introducing a clinical requirement of counseling obese patients may enhance the student’s confidence and ability to be proactive at addressing the obese patient’s oral health.
Offering obesity content in both dental hygiene clinical programs and in continuing education courses that meet the current need for information is necessary to ensure that both entering dental hygiene clinicians as well as currently practicing dental hygienists are reached with this information. Respondents in our study overwhelming reported that they have not taken any continuing education courses on obesity. Creating continuing education courses on obesity is strongly recommended. This will ensure that all dental hygienists will receive new and useful information on the topic of obesity that they can incorporate into their dental hygiene care. Core curriculum in entry-level dental hygiene programs and continuing education courses specific to obesity education ought to address the currently identified need. Courses should include topics such as etiology, risk factors, nutrition, psychology, patient management, and specific dental hygiene interventions focused on helping the obese patient.
A limitation of this study was response bias. The response rate was only 8%, based on the number of email addresses in the CDHA database. However, the relationship between email addresses and individuals is uncertain. Another limitation may have been that the body image category was self-reported. The Body Mass Index would have provided a more accurate system to categorize the individuals into underweight, normal or average weight, and overweight categories. However, in this study, we were interested in the influence of respondents’ perception of their body image, rather than their actual weight. The third potential limitation may be due to the sensitivity of the study; respondents may have answered in a way that they think was the correct choice instead of choosing what they truly felt.
Conclusion
Dental hygienists in this study exhibited mildly negative attitudes toward the obese population. Most attitudes were similar among self-reported body images. It is recommended that dental hygienists be made aware of any negative attitudes toward the obese population and that content specifically addressing obesity and the role of the dental hygienist in addressing the health effects of obesity be incorporated into current curricula and continuing education courses. With these recommendations, dental hygienists could offer care that would enhance the oral and systemic health of their obese patients.
ACKNOWLEDGMENT
The authors appreciate the support of the California Dental Hygienists’ Association for assisting with the distribution of the survey.
ABOUT THE AUTHORS
Gwen Essex, RDH, MS, EdD, is HS Clinical Professor in the Department of Preventive and Restorative Dental Sciences at the University of California, San Francisco, and Co-Director of the Virtual Dental Home Clinics at the University of the Pacific Arthur A. Dugoni School of Dentistry. Keiko Miyahara, RDH, BA, MS, is a graduate of the Master of Science Program in Dental Hygiene, and Dorothy J. Rowe, RDH, MS, PhD, is Associate Professor Emeritus in the Department of Preventive and Restorative Dental Sciences at the University of California, San Francisco.
REFERENCES
1. World Health Organization. Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:i–xii, 1253. Geneva: World Health Organization. 2000.
2. Flegal KM, Carroll MD, Ogden CL, Johnson, CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288(14):1723-1727.
3. Skinner A, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr. 2014;168(6):561-566.
4. Centers for Disease Control and Prevention. Health consequences. [Internet]. 2012 Apr [cited 2015 May 31]. http://www.cdc.gov/obesity/causes.health.html.
5. Sabin JA, Marini M, Nosek BA. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PloS One. 2012;7(11):e48448.
6. Phelan SM, Dovidio JF, Puhl RM, et al. Implicit and explicit weight bias in a national sample of 4,732 medical students: The medical student changes study. Obesity. 2014;22(4):1201-1208.
7. Persky S, Eccleston CP. Medical student bias and care recommendations for an obese versus non-obese virtual patient. Int J Obes. 2011;35(5):728-735.
8. Foster GD, Wadden TA, Makris AP, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11:1168-1177.
9. Magliocca KR, Jabero MF, Alto DL, Magliocca JF. Knowledge, beliefs, and attitudes of dental and dental hygiene students toward obesity. J Dent Educ. 2005;69(12):1332-1339.
10. Schwartz MB, Chambliss HO, Brownell KD, et al. Weight bias among health professionals specializing in obesity. Obesity Res. 2003;11(9):1033-1039.
11. Bacon JG, Scheltema KE, Robinson BE. Fat phobia scale revisited: the short form. Int J Obes. 2001;25:252-257.
12. Crandall CS. Prejudice against fat people: ideology and self-interest. J Pers Soc Psychol. 1994;66(5):882-894.
13. Wellborn SE. Comparison of obesity bias, attitudes, and beliefs among undergraduate dietetic students, dietetic interns, and practicing registered dietitians (unpublished dissertation). East Tennessee State University, Johnson City, Tennessee. 2013.
14. Walter ME, Ragan K, Sulak TN, Bagby JH. Implicit and explicit biases toward obesity: perspectives of school of education students. J Community Med Health Educ. 2013;3(3):1-6.
15. Kading CL, Wilder RS, Vann WF Jr, Curran AE. Factors affecting North Carolina dental hygienists’ confidence in providing obesity education and counseling. J Dent Hyg. 2010;84(2):94-102.
16. Suvan J, D’Aiuto F, Moles DR, et al. Association between overweight/obesity and periodontitis in adults. A systematic review. Obesity Reviews. 2011;12:e381-e404.
17. Genco RJ, Grossi SG, Ho A, et al. A proposed model linking inflammation to obesity, diabetes, and periodontal infections. J Periodontol. 2005;76:2075-2084.