You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
Multidisciplinary efforts from both paid emergency responders and unpaid volunteers are needed to improve the capacity of community responses to mass fatality incidents (MFIs).1-3 Failure to identify and organize disaster response teams leads to errors, slows the victim identification process, increases confusion and frustration, and could compromise the safety of responders.4 Due to the demand for better organization of trained responders, the US Department of Homeland Security has recommended all allied healthcare professionals obtain specialized training to prepare for, manage, and recover from MFIs.5 The American Board of Forensic Odontology (ABFO) recognizes dental hygienists as allied health professionals who have the education and licensures applicable to disaster preparedness and response training, particularly in terms of disaster victim identification (DVI).6 DVI is a scientific and formal process utilized when a disaster results in a large number of human fatalities, where victim identification needs to be confirmed. This is often accomplished by comparing accurate antemortem (AM) dental records to a victim’s postmortem (PM) dental evidence.6
There are multiple examples of MFIs, which have been negatively affected by the challenges of organizing disaster preparedness and response trained personnel. DVI errors made during the 1983 Beirut, Lebanon, terrorist disaster and 1985 Arrow Airlines accident were attributed to unorganized and untrained DVI team members.7 These errors were thought to be a result of inappropriate use of forms, charting errors, use of nonsecure areas for AM record management, and poor transcribing skills.7 More recently, during the September 11, 2001, New York terrorist attacks, an estimated 350 dental health professionals responded as DVI volunteers. Excluding 78 compensated Disaster Mortuary Operational Response Team (DMORT) personnel, most responders did not have specialty training.8 For the purpose of avoiding significant delays in the victim identification process, responders were not turned away despite difficulties collecting documentation showing each volunteer’s specific qualifications; therefore, a significant burden was created for incident managers regarding chain of command and accountability.1,8,9
In a 2007 survey by the American Dental Hygienists’ Association (ADHA), dental hygienists listed forensic dentistry as a topic of interest10; however, existing research does not provide data on recent disaster preparedness and response involvement by dental hygienists during MFIs. Of the minimal information that could be found, dental hygienists’ involvement with disaster preparedness and response appears to be limited to few individuals when considering the estimated 150,000 dental hygienists across the United States.10,11
Role of the Disaster Preparedness and Response Trained Dental Hygienist
Dental hygienists have knowledge and skills that are helpful to disaster preparedness and response and DVI efforts.12 Competencies of licensed dental hygienists that make these professionals assets include knowledge of dental root morphology, the intricacies of the oral cavity, dental nomenclature, and exposing diagnostic quality dental radiographs, as well as communication skills and manual dexterity accessing the oral cavity.11-14 To ensure successful outcomes of assigned roles and responsibilities, all volunteers should seek disaster preparedness and response training prior to becoming involved, regardless of their professional specialty or background.15
Dental hygienists’ roles during disaster preparedness and response can vary. Roles recommended for dental hygienists include managing dental personnel, obtaining and standardizing AM dental records, assisting authorities, transcribing data into databases, assisting surgical procedures, exposing radiographs, aiding multiple verifications during PM exams, monitoring team members for fatigue, assisting with PM dental charting and evidence collection, triaging dental records, assisting the search for matches, and sorting charts.11-14,16 Disaster response roles can be emotionally and psychologically challenging due to activities involving exposure to commingled and scattered human remains. Therefore, some responders may prefer a role serving the team by managing records, equipment, or personnel rather than performing duties that require physical contact with victim remains.13,17
Antemortem (AM) Data Management for the Dental Hygienist
The accuracy of AM dental records is a legal responsibility of the dental team, but records are known to occasionally contain errors. During the 2004 Asian tsunami, DVI team members reported that of the 106 AM dental records received, 54% of accompanying radiographs were of poor quality, several charts contained no AM radiographs, and half of the AM records had to be returned due to insufficient information.2 One of the most basic ways clinical dental hygienists can assist DVI efforts is by advocating for and providing accurate and comprehensive AM dental record-keeping techniques.
According to Brannon and Connick, dental hygienists are capable of working with legal authorities for the purpose of obtaining relevant AM dental record information from healthcare providers.11 It has also been suggested that dental hygienists with psychological first-aid training could communicate with the victim’s family to obtain items showing visual identification information (photographs) or household items containing the victim’s DNA (such as a toothbrush).8 Once all AM materials have been collected, administrative control of the AM record and chain-of-evidence can be managed by the dental hygienist to ensure proper security.11 The interpretation and organization of official AM records is considered one of the most time-consuming and difficult tasks facing forensic odontologists due to the variations of each dental professional’s own subjective style.18 Since dental hygienists are familiar with common notations, abbreviations, and dentition numbering systems often used in dental charting, they can provide interpretation verification attempts and transcribe for official odontogram forms.11,12 Efficiency would be gained by the DVI team utilizing trained dental hygienists for all AM-related tasks.12
Postmortem (PM) Data Management for the Dental Hygienist
Dental hygienists can have a role during PM dental evidence collection through exposing dental radiographs, taking photographs, surgical assisting, cleaning victim remains of debris, charting examination observations, and cross-checking for quality assurance.11-14 Cross-checking involves one odontologist completing the exam and verbalizing the details documented by a dental hygienist; a second odontologist will then verify the final documentation.13 This multiple-verification system helps to avoid errors. Proper storage and labeling of surgically removed remains, as well as the chain of custody for other collected evidence such as hard-copy images and hard-copy odontogram forms, can be assigned to dental hygienists after physical examinations are completed.13
Once the AM and PM data collection portions of the identification process are complete, comparison work can begin by using victim identification software.11 Trained dental hygienists who choose to work in the capacity of data entry could relieve odontologists of this time-consuming task. Assigning forensically trained dental hygienists to these duties can increase the efficiency and accuracy of the DVI process.
Disaster Preparedness and Response Formal Education for the Dental Hygienist
All healthcare disaster responders should have the opportunity for learning about their roles through formal education. According to Hsu et al, disaster preparedness and response competencies need to be identified, and instruction should be tailored to all healthcare workers.19 Many healthcare disciplines, with encouragement from the federal government,5 are slowly incorporating disaster preparedness and response curriculum into formal education and continuing education; yet, coursework for DVI and disaster preparedness and response is lacking within the dental hygiene formal curriculum.12,13 Cognitive concepts and skill competencies for dental hygienists responding to MFIs or serving DVI teams are not fully understood or available for reference. Although disaster preparedness and response competencies have not been established for dental hygienists, general cross-discipline competencies have been suggested.19 These healthcare worker competencies include recognizing disaster events and implementing appropriate response actions, applying principles of disaster management, demonstrating safety in disaster situations, understanding emergency operation plans, demonstrating effective communication, understanding the chain of command, and having the knowledge and skills needed to fulfill the personal role.19 Details for each of these competencies as they relate to dental hygienists are unknown but could assist curriculum developers interested in building disaster preparedness and response educational opportunities for dental hygienists.
Reasons for this deficiency in the dental hygiene curriculum are not fully understood; however, Hermsen et al examined similar deficiencies in the dental curriculum and cited possible contributing factors such as a lack of qualified instructors, lack of time or interest for course development among faculty, lack of implementation interest among administrators, and a lack of time for inclusion in an already rigorous curriculum.20 Hermsen et al also offered possible solutions to these challenges: schools could consult a local medical examiner or coroner to locate forensic odontologists willing to offer support in the development and delivery of forensic classes; students could participate as volunteers in community disaster drills; forensic courses could be taught using distance educational technology, and interested faculty members could be trained through American Society of Forensic Odontology (ASFO)–accredited courses and travel to school programs to facilitate hands-on learning activities.20 These solutions may assist dental hygiene curriculum developers who wish to incorporate forensics coursework.
Topics of disaster preparedness and response training that dental hygienists may need in addition to their educational background and work experiences include: infection control protocol for DVI, recommended personal protective equipment (PPE), dental radiology techniques, equipment utilization, and working knowledge of identification software such as WinID.14,20,21 Organizations devoted to identifying, recruiting, training, and organizing medical health professionals prior to MFIs maintain registrations so that volunteers can be quickly and efficiently activated when needed.
Disaster preparedness and response organizations have become the authority on disaster management, and serve as resources for healthcare professionals interested in community service during MFIs. A list of organizations offering training and their website can be found in Table 1.9,13,22-26 Dental hygienists can contact these organizations as a route for becoming trained and becoming more involved with disaster preparedness and response.
The scientific literature does not offer sufficient data about dental hygiene professionals regarding disaster preparedness and response. The purpose of this study was to fill a gap in the literature by investigating information on US dental hygienists’ interests, current involvement, formal education, views, comfort levels, and intentions for involvement with disaster preparedness and response. The survey investigated four research questions:
1. Does interest in disaster preparedness and response among US dental hygienists reflect their current involvement?
2. Have dental hygienists been formally educated on disaster preparedness and response roles, and what are their views?
3. What level of perceived comfort do dental hygienists feel regarding DVI tasks?
4. Do dental hygienists have intentions for becoming involved with disaster preparedness and response?
Methods and Materials
A 21-item online, electronically delivered survey was utilized for the study. There was no previously existing survey of this kind in the dental hygiene literature; therefore, the survey was researcher-designed by dental hygiene faculty with MFI disaster preparedness and response training.
Approval from the College of Health Sciences of Old Dominion University (ODU) Institutional Review Board (IRB) was obtained prior to administrating the survey. Ten full-time dental hygiene faculty members from the ODU School of Dental Hygiene pilot-tested the online, electronic survey. Survey questions were clarified based on comments and responses resulting from the pilot test prior to deployment. Two groups of respondents participated in the deployed survey: (1) US dental hygienists who attended the February 2014 ODU Dental Hygiene Winter Weekend Continuing Education Conference in Virginia Beach, Virginia; and (2) US dental hygienists who belonged to randomized dental hygiene groups on the social media website Facebook. Attendees for the Winter Weekend continuing education conference were provided computers to take the online survey, and those belonging to the randomly selected four Facebook groups were provided a website link to open the survey. Prospective participants consisted of a random sample who were willing to respond to the online link posted. A cover letter explained the purpose of the study and informed consent requirements. Survey instructions explained inclusion/exclusion criteria and asked that only US dental hygienists participate.
Statistical analysis was performed using SPSS software. Data were analyzed using descriptive statistics, chi-square goodness-of-fit tests, and a paired-samples t-test; the significance level was set at α = 0.05. Qualitative responses were identified and grouped into common themes from open-ended questions.
Results
Demographics
The survey was completed by 334 US dental hygienists. Respondents were primarily female (99.4%) clinical practitioners (89%) with a bachelor’s degree (45.2%); 31 to 35+ years of work experience was indicated most frequently (23%). Respondents in the study represented 41 of the 50 United States, with the Commonwealth of Virginia having the highest percentage of participation (39%, n = 129). Of the respondents, 67% indicated residing in a community susceptible to at least one potential hazard (natural, accidental, or terrorist in nature) that could result in an MFI. Table 2 summarizes the sample’s demographics.
Disaster Preparedness and Response Interest Among Dental Hygienists
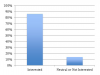
When survey respondents were asked to indicate their level of professional interest in disaster preparedness and response, 86% of the dental hygienists indicated interest, while 14% were neutral or not interested (Figure 1). A chi-square goodness-of-fit test was performed, revealing the interest in this specialty area to be statistically significant among the respondents (P = .000).
Current Involvement With Disaster Preparedness and Response
The majority of respondents in the current study indicated not being a member of disaster preparedness and response organizations (95%) and not having ever participated in an MFI (97%). Eight respondents indicated membership with the following disaster preparedness and response teams: American Board of Forensic Odontology (ABFO) (n = 1), American Red Cross (n = 1), Disaster Mortuary Operational Response Team (DMORT) (n = 1), Emergency System for Advance Registration of Volunteer Health Professionals (ESAR-VHP) (n = 1), Medical Reserve Corps (MRC) (n = 3), and Community Emergency Response Team (CERT) (n = 1). Regarding types of MFI scenarios the dental hygienists would consider being involved in as a responder if called in the future, 93% indicated willingness to serve for a small-scale disaster, 68% chose large-scale disasters, 58% said they would be willing to travel to any US state, and 34% said they would consider international travel.
Concerns among the dental hygienists related to responding to an MFI included: too gruesome (34%), too depressing/sad (40%), difficulty with post-event emotions (38%), risk of exposure to radiation during a nuclear incident (36%), safety regarding increased risk of exposure to infectious diseases in a mortuary setting (31%), cost of training (34%), and inability to leave family in order to serve (31%). Only 42 respondents (13%) indicated that they had no concerns about responding to an MFI.
Formal Education and Views Among Dental Hygienists for Disaster Preparedness and Response
Analysis of survey data found that respondents typically did not receive formal education about disaster preparedness and response roles for dental hygienists (Figure 2). A chi-square goodness-of-fit test with expected equal proportions indicated a statistically significant difference in the number of people who affirmed (7%) and the number of people who denied (93%) receipt of such formal instruction (P = .000). Additionally, over half of the respondents agreed that there were not enough continuing education opportunities available for this specialty area. When respondents were asked if the disaster preparedness and response role of dental hygienists should be covered in the formal dental hygiene curriculum, 86% agreed.
Comments were offered by 117 of the respondents to explain their view on whether or not hygienists could have a vital role in disaster preparedness and response. Most of these responses made reference to the traditional formal education and experience common to all dental hygienists prior to obtainment of any specialized training. Twenty comments were selected and organized into themes: education and experience, need more information on the topic, or miscellaneous (see Table 3 for select comments).
Perceived Comfort Regarding DVI Activities
Respondents were asked to rate their perceived comfort for nine activities related to DVI work; four of those activities involved contact with human remains while five activities did not involve direct contact with human remains (Table 4). A paired-samples t-test revealed a statistically significant mean difference between the perceived comfort felt when respondents were asked about contact activities compared to no contact activities. Respondents indicated more comfort with no contact activities (M = 84%, SD 15%) when compared to contact activities (M = 74%, SD 18%), a statistically significant mean difference of 9%, (95% CI [.08, .11], t(324) = 13.2, P < .05). Out of the five no-contact activities, respondents were most comfortable with digitizing information collected from dental records into identification software (89%) and working collaboratively with members of other professions (97%). Out of the four contact activities, respondents were most comfortable with taking photographs of victim remains (76%) and exposing dental radiographs on victim remains (83%).
Intentions for Involvement With Disaster Preparedness and Response
Respondents were given a list of scenarios for becoming involved with disaster preparedness and response and were asked to indicate their intentions for each (Table 5). Two scenarios with the most agreement were: “I will serve by maintaining accurate antemortem dental records” (n = 210, 64%) and “I will seek more information and decide once I am better informed” (n = 220, 67%). Agreement for a negatively worded scenario and considered as a negative response for becoming involved was: “I will stay informed about dental hygiene’s involvement, but I will not pursue this type of work.” (n = 147, 47%).
Discussion
A search of the literature gave minimal information about the dental hygiene profession as it relates to disaster preparedness and response; therefore, the intent of this study was to serve as a basis for building the dental hygiene literature on the topic. The broad findings of this study provide information about dental hygienists’ interest and formal education in disaster preparedness and response, perceived level of comfort regarding DVI tasks, and intentions of dental hygienists to become involved with disaster preparedness and response. Considering recommendations from the federal government and ABFO for dental hygienists to become involved, along with interest among dental hygienists revealed by the current study, justification exists for making disaster preparedness and response educational opportunities more accessible for these professionals. Results of this study could aid dental hygiene professionals and program administrators in realizing the need for establishment of more opportunities for disaster preparedness and response education to initiate involvement.
The response for this study included dental hygienists from much of the United States with a wide range of educational backgrounds and years of work experience, as well as a range of dental hygiene professional capacities. Results suggest that interest in disaster preparedness and response among dental hygienists is overwhelmingly positive, yet the majority of respondents indicated not being a member of disaster preparedness and response organizations and not having ever participated in an MFI. Therefore, it is proposed that reported low participation is not due to a lack of interest. A possible explanation for low participation could be a lack of dental hygiene educational opportunities. Dental hygienists who are not educated about this topic may be unaware of this service opportunity or unsure of possible routes for being involved. As indicated by respondents, over half felt that there are not enough continuing education opportunities, and almost all said this specialty topic was not a part of their formal education. When respondents were asked if the disaster preparedness and response role of dental hygienists should be covered in the formal dental hygiene curriculum, 86% agreed. The findings of this study that a lack of educational opportunities for this topic exists in dental hygiene are supported by the paucity of information available on how dental hygienists are prepared in this specialty, as well as suggestions from Nuzzolese et al and Ferguson et al about the lack of disaster preparedness and response in dental hygiene curriculum.12,13
According to survey results, the respondents were mostly comfortable with DVI activities regardless of whether or not the activity required physical contact with human remains. The literature suggests that disaster preparedness and response participants should be screened for their levels of comfort, and task assignments should take reported comfort levels into consideration.3 Therefore, this finding is important when considering the need to identify participants who are able and willing to perform activities associated with the sensitive nature of DVI work.17 Table 6 provides an up-to-date list of roles for trained dental hygienists suggested by the literature from 1982-2015.
The literature suggests that specialty-trained dental hygienists have a vital role in disaster preparedness and response and are able to serve as needed personnel11-13; respondents of the current study overwhelmingly agreed, which is encouraging. Comments offered by respondents explaining their views on why dental hygienists have a vital role primarily made reference to the traditional formal education and experiences common to all dental hygienists prior to obtainment of any specialized training. Also, a majority of respondents reported they would consider responding to participate in MFIs; yet, less than half of the responders agreed to seek disaster preparedness and response courses for obtainment of specialized training and certification. However, dental hygienists who intend to become involved without proper training have a misconception about their abilities to adequately perform disaster response and DVI activities. As pointed out in the literature, while disaster responders are needed, those who lack training are cause for concern as it relates to the effectiveness of disaster response work and the participants’ safety.4,15
The current research provides new information, which should serve as a basis for designing numerous future studies of this topic. Research is needed to develop disaster preparedness and response competency-based skills specifically for dental hygienists, determine the amount of specialized training needed prior to involvement, further define the role of dental hygienist disaster responders, and assess misconceptions about disaster preparedness and response held by dental hygienists. Specifically, research could be conducted to determine the aptitude of forensically trained dental hygienists as compared to untrained dental hygienists in the following areas: taking documentation photographs and dental radiographs on human remains, assisting with the collection and verification of dental evidence, the ability to utilize special equipment, and PM surgical assistance. Ideal learning approaches for dental hygienists based on specific roles they would have when participating with disaster preparedness and response need to be identified through studies conducted within learning institutions. It would also be beneficial for investigators to gather information on safety protocols dental hygienists would need to follow when performing disaster preparedness and response roles. Such research published in dental hygiene journals would help build the literature, strengthen the dental hygiene community service response for MFIs, and assist with recruiting disaster preparedness and response organization members from the dental hygiene profession.
There are several limitations to this study. The survey tool was researcher-designed; therefore, the reliability and validity of the survey may not have been fully established. This study included dental hygienists from a random sample of the US dental hygienists population and targeted those who chose to be professionally active through social media groups and a continuing education conference; the population may not represent viewpoints of dental hygienists who choose to be professionally active in other ways. A large portion of the surveyed population was from Virginia as a result of the continuing education conference, and two of the four Facebook groups included in the study (Tidewater Dental Hygienists’ Association and Virginia Dental Hygienists’ Association) were based in Virginia. It is possible that dental hygienists of Virginia, where disaster types and frequencies can vary from that of other US regions, may have affected the outcomes of the research due to knowledge or feelings generated by past experiences with disasters in their residential proximity. While over half of the respondents did indicate residential proximity to hazards that could result in MFIs, the research design did not look for correlations of how such factors could have impacted responses.
Conclusion
Dental hygienists are interested in becoming more involved with disaster preparedness and response. They view themselves as professionals who could have a vital role in disaster preparedness and response and are comfortable with DVI-related tasks. Competency and curriculum on this topic should be developed and made readily available to create educational opportunities for dental hygienists who choose to serve their communities in this capacity.
ABOUT THE AUTHORS
Brenda T. Bradshaw, RDH, MSDH, is Dental Hygiene Clinical Adjunct Faculty for the Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University, Norfolk, Virginia. Ann P. Bruhn, RDH, MSDH, is Assistant Professor, Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University. Tara L. Newcomb, RDH, MSDH, is Assistant Professor, Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University. Bridget D. Giles, PhD, is Research Assistant Professor, The Virginia Modeling, Analysis and Simulation Center, Old Dominion University. Kathy Simms, PhD, is Data Analyst and Assistant Professor, Student Engagement and Enrollment Services, Old Dominion University.
REFERENCES
1. Donahue AK, Tuohy RV. Lessons we don’t learn: a study of the lessons of disasters, why we report them, and how we can learn from them. Homeland Secur Affairs. 2006;2(2):1-28.
2. Kieser JA, Laing W, Herbison P. Lessons learned from large-scale comparative dental analysis following the south Asian tsunami of 2004. J Forensic Sci. 2006;51(1):109-112.
3. Rogers B, Lawhorn E. Disaster preparedness: occupational and environmental health professionals’ response to Hurricanes Katrina and Rita. AAOHN J. 2007;55(5):197-207.
4. Hinchliffe J. Forensic odontology, part 2: major disasters. Br Dent J. 2011;210(6):269-274.
5. US Dept of Homeland Security. Washington, DC; Target capabilities list: a companion to the national preparedness guidelines [Internet]. [2007; cited 2014 Jan 9]. http://www.fema.gov/pdf/government/training/tcl.pdf.
6. American Board of Forensic Odontology (ABFO). c2008-2013. ABFO diplomats reference manual [Internet]. [updated 2013 Jan; cited 2013 Aug 28]. http://www.abfo.org/wpcontent/uploads/2012/08/ABFO-Reference-Manual-1-22-2013-revision.pdf.
7. Brannon RB, Kessler HP. Problems in mass-disaster dental identification: a retrospective review. J Forensic Sci. 1999;44(1):123-127.
8. Zohn HK, Dashkow S, Aschheim KW, et al. Odontology victim identification skill assessment system. J Forensic Sci. 2010;55(3):788-791.
9. US Dept of Health & Human Services (HHS). Washington, DC; HHS, Department of Public Health Emergency; The emergency system for advance registration of volunteer health professionals (ESAR-VHP). [Internet]. [cited 2013 Nov 7]. http://www.phe.gov/esarvhp/Pages/home.aspx.
10. American Dental Hygienists’ Association (ADHA). Survey of dental hygienists in the United States: executive summary [Internet]. 2007 [cited 2013 Nov 3]. http://204.232.157.152/downloads/DH_pratitioner_survey_Exec_Summary.pdf.
11. Brannon LM, Connick CM. The role of the dental hygienist in mass disasters. J Forensic Sci. 2000;45(2):381-383.
12. Nuzzolese E, Lepore MM, Cukovic-Bagic I, et al. Forensic sciences and forensic odontology: issues for dental hygienists and therapists. Int Dent J. 2008;58(6):342-348.
13. Ferguson DA, Sweet DJ, Craig BJ. Forensic dentistry and dental hygiene: How can the dental hygienist contribute? Probe. 2008;42(4):203-211.
14. Newcomb T, Bruhn A, Giles B. Mass fatality incidents and the role of the dental hygienist: Are we prepared? J Dent Hyg. 2015;89(3):143-151.
15. Trengrove HG, Gray A. The role of military dental capabilities in mass fatality situations. Mil Med. 2013;178(5):523-528.
16. Rawson RD, Nelson BA, Koot AC. Mass disaster and the dental hygienist: the MGM fire. Dent Hyg (Chic). 1983;57(4):12,17-18.
17. Ocak T, Duran A, Ozdes T, et al. Problems encountered by volunteers assisting the relief efforts in Van, Turkey and the surrounding earthquake area. Acad Emerg Med. 2013;12:66-70.
18. Martinez-Chicon J, Valenzuela A. Usefulness of Forensic Dental Symbols© and Dental Encoder© database in forensic odontology. J Forensic Sci. 2012;57(1):206-211.
19. Hsu EB, Thomas TL, Bass EB, et al. Healthcare worker competencies for disaster training. BMC Med Educ. 2006;6(19):1-9.
20. Hermsen KP, Johnson JD. A model for forensic dental education in the predoctoral dental school curriculum. J Dent Educ. 2012;76(5):553-561.
21. Sharma BR, Reader MD. Autopsy room: A potential source of infection at workplace in developing countries. Am J Infect Dis. 2005;1(1):25-33.
22. US Dept of Health & Human Services (HHS). Washington, DC; HHS, Department of Public Health Emergency; Disaster mortuary operational response teams (DMORTs) [Internet]. [cited 2013 Nov 7]. http://www.phe.gov/preparedness/responders/ndms/teams/pages/dmort.aspx.
23. Medical Reserve Corps [Internet]. Rockville, MD; Homepage; [updated 2013 Mar 21; cited 2014 Feb 06]. https://www.medicalreservecorps.gov/HomePage.
24. American Red Cross. Washington, DC; Disaster training [Internet]. [updated 2014; cited 2014 Nov 22]. http://www.redcross.org/take-aclass/disaster-training.
25. Community Emergency Response Teams (CERT). Washington, DC; Home page [Internet]. [updated 2014 Jul 24; cited 2014 Nov 22]. https://www.fema.gov/community-emergency-response-teams.
26. American Society of Forensic Odontology (ASFO). Lubbock, TX; Home page [Internet]. [updated 2013; cited 2014 Feb 06]. http://asfo.org.