You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
For general practitioners, socket preservation can be an excellent initial step to building an implant practice. Most dentists extract teeth, though not all dentists want to place implants. However, if socket preservation is performed, the area is more likely to be suitable for an implant without grafting. As Dr. Carl E. Misch has noted, taking something out should be followed by putting something back in. Socket preservation, however, is not just for patients who may have dental implants placed.1 For some patients who are not candidates for dental implants, there is value in maintaining bone volume for other prostheses and for maintenance of bone around adjacent teeth.2
When performing a socket preservation on a patient, the clinician should be prepared to place an implant in the area in 4 to 6 months. Providing this service for patients will help grow the practice and expand the clinician’s abilities. Offering these services in the dental office must be done in a manner that is organized and properly executed. The patient’s well-being is the most important factor. Expanding the practice into the arena of implant placement should be done methodically and carefully. Implant education along with receiving mentoring is vital,3 as it enables an exchange of information specific to a patient prior to the procedure.
There are a number of reasons for performing socket preservation. A study done by Iasella, Greenwell, et al4 found that grafting of extraction sites with freeze-dried bone increased the height and width of the alveolar ridge compared to sockets that were not grafted. This maintenance of the ridge can be the difference between implant success and failure. There are instances in which grafting distal to second molars after third molar removal may be indicated. These are patients aged 26 or older who have a risk of having a distal defect on the second molar after removal of their wisdom teeth.5
Case Selection
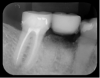
For clinicians who are inexperienced in socket preservation, case selection is crucial in building experience. In some cases grafting may only exacerbate the situation. For example, if the tissue is severly inflamed and fragile (Figure 1), the healing will be less than desireable and grafting may aggravate the area. In such instances, after removal of the tooth, wound management techniques (eg, antibiotics, chlorhexidine, pain management) should be used. Conversely, a good candidate for socket preservation is one that is free from serious infection (Figure 2).
For the inexperienced grafting clinician it is best to start with a five-walled defect.6 There are different treatment techniques used for the different bony defects, as follows:
• Five-walled defect (extraction site with all its walls intact): resorbable grafting material and primary closure (or coverage with membrane)
• Four-walled defect: resorbable grafting material and a membrane
• Three-walled defect: resorbable grafting material, membrane, and growth factors or autogenous bone
• Two-walled defect: resorbable grafting material, membrane, growth factors, autogenous bone, and possibly titanium mesh for support
• One-walled defect: block graft
Starting with the least complex type of graft allows the clinician to build experience and follow routine healing protocols. As clinicians build confidence they can gradually move into more complicated procedures for their patients. Multiple tooth extractions, for example, increase the complexity.
Extraction Site
Proper socket preservation starts with proper tooth removal. The cells on the inner surface of the periosteum are responsible for bone remodeling. If these cells are damaged they have to regenerate before the bone can remodel. Cortical bone receives 80% of its arterial and 100% of venous blood flow from the periostium.7 Therefore, careful handling of the soft tissue is crucial in succesful socket preservation and grafting, in general. Flap reflection should only be performed when necessary and kept to a minimum. For multi-rooted teeth careful sectioning will ensure the soft tissues are protected. Periotomes can also be used to sever the ligaments retaining the tooth to aid in atraumatic removal.
Mandibular molars can be sectioned bucco-lingually and each root removed individually. Maxillary molars are sectioned mesio-distally first, then the palatal root is removed bucco-lingually, and the buccal roots removed individually (Figure 3 through Figure 5). If clinicians are using an air-driven high-speed handpiece, they should not lay a flap as this may give the patient an air embolism.8 If a flap has been reflected, an electric handpiece must be used.
Extraction site healing occurs in four stages9: (1) initial angiogenesis–1 to 4 days; (2) new bone formation–3 to 4 weeks; (3) bone growth–4 to 6 weeks; (4) bone reorganization–6 weeks to 4 months. Healing of an extraction site without grafting occurs by the epithelium growing into the extraction site until it reaches the apical fibrous tissue. The epithelium grows across the fibrous tissue until it meets in the middle.10 Socket preservation raises the level of the area that the epithelium crosses. The graft also helps maintain the width of the ridge by minimizing the remodeling of the buccal and lingual plates.11
Grafting Technique
The patient’s own tissue, whether bone or soft tissue, is considered the ideal grafting material. Each of the four different types of bone grafting material has its own “pros” and “cons”12:
• Autogenous: patient’s own bone. This is the optimal graft for healing and integration; however, its use requires another surgical site and there could be limitations regarding available amount.
• Allograft: harvested from the same species. With allograft, there is no limit to available amount. It has some osteoinductive properties, but patients may object to its use.
• Zenograft: harvested from a different species (eg, bovine). It has no limit to its availability, however patients may object to using it. There are some issues with resorption in that the material may not fully resorb, and also it has no inductive properties.
• Alloplast: synthetic material. While there is no limit to availability and it resorbs nicely, is very consistent, and has good handling properties, alloplast offers no inductive properties.
A mixture of different materials can be used to try to utilize the best characteristics of each. For example, the oseoinductive properties of demineralized human bone may be desired along with the handling properties of a synthetic. (Oseoinduction is defined as new bone formation from osteoprogenitor cells derived from primitive mesenchymal cells.13 Oseoconduction creates a scaffolding for the surrounding bone to form new bone.14)
Other techniques for improving the healing of grafting sites can also be used. The patient’s blood can be centrofuged to separate the different components of it. These components have growth factors that help in the healing process. Platelet-rich plasma (PRP)15 and platelet-rich fibrinogen (PRF) are collectively referred to as platelet-derived growth factors,16 and when mixed with grafting material they improve the acceptance of the grafting materials.17 Many dental offices are not interested in dealing with this level of blood product handling; however, if more advanced grafting is to be done, use of these techniques will improve outcomes.17
Membrane Placement
It is difficult to achieve primary closure of an extraction site without tension on the tissue. Therefore, a membrane frequently must be used to keep the grafting material stable so the healing process can occur. There are two categories of membranes: resorbable and nonresorbable. This is also true for sutures. The author prefers polytetrafluoroethylene membranes and sutures because of their non-inflammatory nature. The healing around this material is excellent. Resorbable membranes should only be used if primary closure can be achieved. The nature of the oral environment will cause resorbable membranes to disolve too quickly to allow proper healing.
The membrane should be placed under the periosteum and over the bone so as to create a 2-mm overlap.18 A horizontal matress suture can be used to secure the tissue over the membrane. Medications after the procedure include amoxicillin 500 mg four times a day for 5 days (if penicillin allergy, Cleocin 300 mg twice daily for 5 days), Toradol 30 mg IM then 10 mg TQ6h (ensuring patient has no aspirin allergies and is not taking blood thinners),19 and chlorhexidine gluconate rinse three times per day.
The case presented in Figure 6 through Figure 15 demonstrates membrane use in what would be considered a four-wall defect. In such a case, the patient would come to the office weekly for evaluation of healing. The sutures would be removed after 3 weeks and the membrane after 4 weeks. The longer the membrane is left in, the better the result. Any exudate that may be coming from under the membrane should be removed immediately. There is no need for anesthetic before membrane removal. The initial angiogenic stage lasts for approximately 3 weeks, therefore it is important to keep the area stable for that amount of time.20
As demonstrated in Figure 16 through Figure 18, after removal of the membrane the area should be free from inflammation and infection. As shown, the area has ample attached gingiva and adequate ridge width for implant placement.
Procedure Implementation
Patients can be informed that this procedure is in the best interest of their long-term dental health and that newer information has brought to light the value in preserving the bone in the extraction site and the surrounding teeth. While some offices may be concerned about how to add this procedure to their treatment planning, the value of it can be seen once these patients begin returning for follow-up treatment. While not every patient will choose to have the procedure done, consistent recommendations are likely to improve the acceptance rate. The continued follow-up will keep the office connected to the patient and increase the probability that the patient will follow through with the remainder of the treatment plan. A cost analysis should be done to help the practice set a fair fee for the procedure. Material costs and the cost of added time and more follow-up appointments must be determined. The procedure is billed as an extraction, bone graft, and separate membrane.
There may be many reasons dental offices do not offer socket preservation procedures. Whether it is lack of knowledge about the procedure or assumptions that patients won’t accept the treatment, it is important that the staff is educated about the benefits of socket preservation. The staff should understand the “vision” of the office in order to support the clinician in his or her quest to provide quality care while enhancing the capabilities of the practice and increasing revenue. If all members of the staff are in unison, patients are more likely to respond positively.21
Whether clinicians are trying to build their practice by placing implants or provide their specialists with the optimum starting point, learning socket preservation can be beneficial. Patients’ expectations for complete dental care are increasing; this includes minimizing their time at the dental office. Offering socket preservation will save patients time and money in the long run.
DISCLOSURE
The author has no disclosures to report.
ABOUT THE AUTHOR
Terry L. Work, DMD
Private Practice, Scottsdale, Arizona
REFERENCES
1. Irinakis T, Tabesh M. Preserving the socket dimensions with bone grafting in single sites: an esthetic surgical approach when planning delayed implant placement. J Oral Implantol. 2007;33(3):156-163.
2. Child PL Jr, Christensen GJ. Extract and graft or extract and dismiss? Dentaltown. September 2011:28-34.
3. Lopez N, Johnson S, Black N. Does peer mentoring work? Dental students assess its benefits as an adaptive coping strategy. J Dent Educ. 2010;74(11):1197-1205.
4. Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003;74(7):990-999.
5. Kugelberg CF. Periodontal healing two and four years after impacted lower third molar surgery. A comparative retrospective study. Int J Oral Maxillofac Surg. 1990;19(6):341-345.
6. Misch CE. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Elsevier; 2008:876-878.
7. Roberts WE, Turley PK, Brezniak N, Fielder PJ. Implants: Bone physiology and metabolism. CDA J. 1987;15(10):54-61.
8. Davies JM, Campbell LA. Fatal air embolism during dental implant surgery: a report of three cases. Can J Anaesth. 1990;37(1):112-121.
9. Ohta Y. Comparative changes in microvasculature and bone during healing of implant and extraction sites. J Oral Implantol. 1993;19(3):184-198.
10. Amler MH, Johnson PL, Salman I. Histological and histochemical investigation of human alveolar socket healing in undisturbed extraction wounds. J Am Dent Assoc. 1960;61(7):32-44.
11. Van der Weijden F, Dell’Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. J Clin Periodontol. 2009;36(12):1048-1058.
12. Misch CE. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Elsevier; 2008:857-861.
13. Urist MR, Strates BS. Bone morphogenetic protein. J Dent Res. 1971;50(6):1392-1406.
14. Misch CE. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Elsevier; 2008:860-863.
15. Sunitha Raja V, Munirathnam Naidu E. Platelet-rich fibrin: evolution of a second-generation platelet concentrate. Indian J Dent Res. 2008;19(1):42-46.
16. Dohan DM, Choukroun J, Diss A, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(3):e37-e44.
17. Sequeria1 JP, Johri S. Platelet rich plasma: clinical applications in dentistry. Sch J Dent Sci. 2015;2(6):355-362.
18. Dimitriou R, Jones E, McGonagle D, Giannoudis PV. Bone regeneration: current concepts and future directions. BMC Med. 2011;9:66.
19. Fricke J, Halladay SC, Bynum L, Francisco CA. Pain relief after dental impaction surgery using ketorolac, hydrocodone plus acetaminophen, or placebo. Clin Ther. 1993;15(3):500-509.
20. Ohta Y. Comparative changes in microvasculature and bone during healing of implant and extraction sites. J Oral Implantol. 1993;19(3):184-198.
21. Morreale SP, Osborn MM, Pearson JC. Why communication is important: A rationale for the centrality of the study of communication. Journal of the Association for Communication Administration. 2000;29:1-25.