You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Access to dental care is a challenge across the United States, which has been attributed to a shortage of trained providers, a lack of funding for dental care, inadequate coverage by health plans, and an aging workforce of dentists.1 A key component of the Patient Protection and Affordable Care Act (PPACA) is to alleviate the shortage of dental services in the United States.2 As of November 2012, there were 195,941 professionally active dentists in the United States with a projected growth rate of 21% annually.3 In 2012, there were 195,903 professionally active dental hygienists in the United States, with a projected growth rate of 38% annually.4,5 The total number of dental graduates in 2012 was 5,199, whereas the total number of dental hygiene graduates in 2012 was 7,103.4 If these trends continue, the annual increase of dentists is projected to insufficiently meet the increase of population need for dental providers in the United States each year.6
The high cost of dental care, lack of dental insurance, and misdistribution of dental providers prevent many Americans from obtaining dental care.7 From 2010 to 2011, 13.2% of Americans who were interviewed stated that they did not obtain dental care during the previous 12 months due to the high cost.7 In addition, as of 2013, there were 4,595 dental care Health Professional Shortage Areas (HPSAs) in the United States where there were an insufficient number of providers to meet the needs of the population.6 Across these shortage areas, only 42% of the population need was met.6 The number of additional dentists and dental hygienists required to meet 100% of the population need is 6,531.6
Dental hygienists are licensed preventive dental professionals who could help reduce the current burden of need if they were permitted to work without dental supervision in all 50 states.6 Currently, licensure requirements call for all US dental hygienists to graduate from an accredited dental hygiene program and complete a written national examination in addition to a regional or state clinical examination.8 In eight states a dental hygienist is legally required to be directly supervised (on the premises) by a dentist while providing preventive dental services.9 In other states that have some level of general supervision, the dentist is legally required to authorize preventive services provided by a dental hygienist prior to implementation.9 Therefore, an individual must be examined by a dentist prior to being treated by a dental hygienist for preventive services in general supervision states.
As a comparison, The Report on the Future of Nursing recommends removing scope-of-practice barriers in healthcare to facilitate the ability of registered providers to work to the full extent of their education and training.10 This report has increased attention to scope-of-practice and state supervision regulations in nursing.10 Investigators have shown that using healthcare mid-level providers such as nurse practitioners to execute services that they are licensed to deliver is cost-effective and accepted by patients.11 It is estimated that the average cost of a physician assistant or nurse practitioner visit is 20% to 35% lower than a physician visit.12 In a study by Dierick-van Daele et al, patients seeing nurse practitioners were more satisfied and felt that the quality of care was equivalent to physician care.11
Professionals such as nurse practitioners are allowed greater autonomy to make decisions about the care of their patients. Autonomy is defined as self-governing; a social environment where others are considered as separate individuals capable of self-determination.13 Gender and class background have been a significant factor in the autonomy and self-regulation of professions.14 In the early periods of professions, women were excluded from entrance into professions, which established a male domination. Whittington found that gender still plays a statistically significant factor in science-based professions.15
It is unclear if dental hygienists, who are predominately female,16 feel capable of autonomy in the care of patients and if their education has prepared them to take on this role. The purpose of this study was to determine if dental hygienists from different states view their education and capabilities as adequate to provide preventive dental care independently to individuals in need and underserved areas.
Methods and Materials
The study used a cross-sectional, quantitative survey design. A stratified sample, based on state dental supervision levels for dental hygienists and gender, was drawn from state dental boards or dental hygiene boards that would allow access to the email or mailing addresses of dental hygienists. The sample was obtained from state boards with various dental hygiene supervision levels. The sample of registered dental hygienists was randomly selected from eight preselected sample states based on dental supervision levels of dental hygienists and ability to obtain email and traditional mailing addresses. The states that were utilized in the study included: Alabama, California, Colorado, Florida, North Carolina, Tennessee, Washington, and West Virginia. The states were divided into four categories of state regulated dental supervision: direct access with local anesthesia allowed, general supervision/direct access with local anesthesia allowed, general supervision with local anesthesia allowed, and direct supervision/general supervision with no local anesthesia allowed. In order to ensure an acceptable number of male dental hygienists in the study sample, all male dental hygienists within six of the states were solicited since there were fewer than 100 male dental hygienists within these states. Table 1 displays the number of available participants by each state used in the study.
The study used a confidence level of 90%, a 0.5 standard deviation, and a confidence interval of +/- 5% in order for the results to be considered statistically significant. Using a MANOVA sample analysis table, the sample size needed for this study was 130 participants for a medium effect and an alpha level of 0.05 for eight groups with six variables.17 Therefore, surveys were sent to 1,250 registered dental hygienists in order to obtain the 130 respondents for a precision level sample size of eight dental hygiene groups.18
Two tools were used to collect data for this study. The first was the Dempster Practice Behaviors Scale (DPBS) instrument utilizing scale rated questions.19 The survey questionnaire was designed by the principal investigator, Judith S. Dempster, in 1990 for her dissertation. The questionnaire was tested for reliability and validity prior to its use in other studies.19 The second instrument gathered demographic data, including a nominal scale of age, gender, educational background, highest dental hygiene degree level obtained, clinical employment status, teaching status, graduation year from a dental hygiene program, and state of current residence.
The study participants were recruited in June and July of 2014. Implied consent was used, that is, completing the questionnaire implied that participants were willing to participate in the study. Over a 1-month period, 650 surveys were mailed through the US Postal Service. In addition, 600 survey links were emailed to dental hygiene potential participants through Survey Monkey. Candidates in Alabama, California, Colorado, and North Carolina were mailed surveys through the postal service along with a self-addressed stamped return envelope. Candidates in Florida, Tennessee, Washington, and West Virginia were sent an email invitation to complete the survey online through Survey Monkey. In addition, 100 randomly selected female dental hygienists and 100 randomly selected male dental hygienists, all with an active license from each of the eight states, were sent surveys. Due to an insufficient number of male dental hygienists within six states, only 25 surveys were sent to Alabama male dental hygienists, 63 to Colorado male dental hygienists, 73 to North Carolina male dental hygienists, 23 to Tennessee male dental hygienists, 67 to Washington male dental hygienists, and nine to West Virginia male dental hygienists.
Results
Of the 1,250 surveys that were sent, a total of 405 surveys (32.4%) were returned. Of the 405 returned surveys, 198 (48.9%) were mailed surveys and 207 (51.1%) were online surveys. Forty-seven online surveys (7.8%) and 22 mailed surveys (3.4%) were returned as undeliverable. Twenty-one online recruits (3.5%) declined survey participation. Total usable surveys numbered 360 (88.9%).
Figure 1 through Figure 5 show the frequency distribution of the study participants based on age, employment status, years of clinical experience, education level, and state of residency. The average age of the participants was 45.41 years. Clinicians numbered 333 (92.5%) and 27 (7.5%) were educators. Twenty-six (7.2%) had a certificate in dental hygiene, 191 (53.1%) had an associate degree in dental hygiene, 113 (31.4%) had a bachelor’s degree in dental hygiene, 27 (7.6%) had a master’s degree in dental hygiene, and 3 (0.8%) had a doctorate degree.
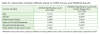
The ANOVA results in Table 2 show that there were no significant differences among the DPBS scores when comparing state dental supervision levels, age groups, education level, employment status, gender, or years of clinical experience among dental hygienists. However, the MANOVA results show that there were significant differences among DPBS scores when comparing state dental supervision levels with age, educational level, and gender. These results reiterate that ANOVA post hoc analyses ignore the fact that the MANOVA hypothesis includes sub-hypotheses about linear combinations of dependent or control variables.20
Follow-up pairwise comparisons were conducted for the dependent variable, independent variable, and five control variables. With the Bonferroni method, each comparison was tested at the alpha level for the ANOVA divided by the number of comparisons.20 In addition, the same five comparisons were performed using the Dunnett’s C method since the variances for gender and employment status were not homogenous. For age, educational level, and gender there was a significant difference in DPBS mean scores among the four dental supervision levels. There was a nonsignificant difference in the means between: employment status and years of clinical experience among the four dental supervision levels and also means of the four dental supervision levels alone.
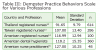
Total autonomy scores ranged from 57 to 148, with a mean of 118.20 (SD = 15.35). Based on the DPBS the higher the score, the higher level of autonomy with possible scores ranging from 30 to 150.19 The instrument scale does not classify a range for scoring. When compared to other DPBS instrument research results, these findings show that dental hygienists within this sample perceived high levels of autonomy. Table 3 displays the DPBS results for registered dental hygienists and other professions that have completed the DPBS survey.
The DBPS used a five-point Likert scale ranging from 1 (not at all true) to 5 (extremely true).19 Table 4 displays the mean results of the DPBS instrument for the four subscales based on state dental supervision level: readiness, empowerment, actualization, and valuation.19 The Readiness subscale had 11 item statements and measured elements of skills, competence, and mastery. The Empowerment subscale had seven items and measured the acceptability of performance in a practice setting. The Actualization subscale included nine items and measured accountability, decision making, determination, responsibility. The Valuation subscale included three items and measured elements of worth, value, merit, and usefulness related to autonomy in practice.
Discussion
Overall, the sample of dental hygienists had a DPBS mean score of 118.2 out of a range of 30 to 150 autonomy level score. This finding supports research from McCain, which found that Virginia dental hygienists had a strong belief in competency skills and desire to work in nontraditional settings, under general dentist supervision.21 For example, the current study found that American registered dental hygienists had a higher DPBS mean score than registered nurses from Thailand, Taiwan, and the United States. These findings also corroborate the findings of Turner et al, who found that European dental hygienists feel competent to complete some preventive dental care services unsupervised.22 The Turner et al study surveyed 150 dental hygienists, 183 hygiene-therapists, and 152 dental therapists from England, Scotland, Wales, and Northern Ireland and found that these providers felt competent to diagnose periodontal disease and provide preventive dental care without a supervising dentist on the premises. In addition, the findings of this current study agree with the findings of Robinson et al that found military nurses in highly ordered settings similar to direct supervision have less autonomy.23 General supervision dental hygienists have the ability to work independently in some settings, whereas the dental hygienists in the direct supervision states are unable to work independently in any settings and had the lowest autonomy DPBS mean score of the four supervisory categories in the current study.
This study revealed that one possible explanation of why direct access dental hygienists do not have a higher level of autonomy is because of bureaucratic restrictions where they are employed. For example, a 51- to 55-year-old female direct access clinician from California with 20 to 24 years of dental hygiene experience stated, “My office has made their own rules and in many ways my decisions are limited due to not being able to decide without a dentist giving the okay for treatment. Sometimes they agree and sometimes not.” Other DPBS survey comments argued that the requirement of completing different state clinical board examinations if moving from state to state restricts autonomy. Therefore, dental hygienists within the direct access states are experiencing different restrictions to providing unsupervised preventive dental treatment to underserved populations from the other dental supervision leveled states; however, they are still experiencing restrictions.
Educational level, gender, and age appear to affect the level of professional autonomy among the dental hygienists within the eight states of this study. Therefore, prospective research that explores a deeper understanding of these results may reveal currently unknown aspects of dental hygienists and state supervision levels.
There are limitations within this study. First, survey results gathered from the small random sample of 360 participants cannot be generalizable to a larger population of dental hygienists in the United States when they have unique levels of dentist supervision. The study sample may not be representative of the larger dental hygienist population thus hindering external validity. Second, the sample of male dental hygienists and educators that participated in the study was limited. Numbers of male dental hygienists vary as do numbers of dental hygiene educational programs between states limiting the ability to generalize the results. Third, the topic of dental hygiene independent practice and self-regulation is controversial. Participants may not have been willing to respond to the survey if they were not absolutely certain of anonymity or how the study results were to be used. Therefore, the participants could have failed to respond truthfully. Lastly, registered dental hygienists who are interested in independent practice and self-regulation for the profession may have been more likely to participate in the study compared to registered dental hygienists that have less interest in becoming autonomous. The study results that show a high level of autonomy among dental hygiene participants may be due to a more autonomous study sample.
Further studies on the attitudes of dental hygienists toward independent practice and professional autonomy are warranted. This study’s small random sample did not show a difference in autonomy levels among dental hygienists based on employment status or years of clinical experience when state dentist supervision levels were taken into consideration. A larger study sample size needs to be obtained in order to capture a broader range of participants. In addition, a qualitative study could further investigate why dental hygienists from this study feel “taken advantage of by dentists.”
Conclusion
The DPBS scores of the study sample suggest that dental hygienists feel prepared and competent to perform preventive dental hygiene services without dentist supervision. The attitudes of the dental hygienists from each of the four state dentist supervision levels support a move toward achieving professional jurisdiction of preventive dental care within the United States. For this shift in bureaucratic power to occur, a disruption in dental tasks and jurisdictions must transpire between the dental and dental hygiene professions.
ABOUT THE AUTHOR
April Catlett, MDH, PhD, is the Macon Campus Dental Hygiene Program Chair at Central Georgia Technical College.
ACKNOWLEDGMENTS
The author would like to acknowledge Cheryl Anderson, Dissertation Committee Chairperson; Jeanne Connors, Dissertation Committee Member; and Dorothy Browne, University Reviewer for their contribution to this research.
REFERENCES
1. Health Resources and Services Administration. The professional practice environment of dental hygienists in the fifty states and the District of Columbia, 2001. National Center for Health Workforce Analysis, Bureau of Health Professions [Internet]. 2004 [cited 2014 Jan 5]. http://bhpr.hrsa.gov/healthworkforce/reports/dentalhygiene50statesdc.pdf.
2. US Congress. Bill 3590. United States Government Printing Office [Internet]. 2010 [cited 2014 Jan 8]. http://www.gpo.gov/fdsys/pkg/BILLS-111hr3590enr/pdf/BILLS-111hr3590enr.pdf.
3. US Dept of Labor. Bureau of Labor Statistics: occupational outlook handbook for dentists. US Dept of Labor [Internet]. 2013 [cited 2014 Jan 7]. http://www.bls.gov/ooh/Healthcare/Dentists.htm.
4. American Dental Education Association. Dental and allied dental graduates: 2001-2012. American Dental Education Association [Internet] 2013 [cited 2014 Jan 6]. http://www.adea.org/uploadedFiles/ADEA/Content_Conversion_Final/publications/Trend sinDentalEducation2009/AlliedDentalHealth/DentalandAlliedDentalGraduates.pdf.
5. US Dept of Labor. Bureau of Labor Statistics: occupational outlook handbook for dental hygienists. US Dept of Labor [Internet] 2013 [cited 2014 Jan 7]. http://www.gpo.gov/fdsys/pkg/BILLS¬111hr3590enr/pdf/BILLS-111hr3590enr.pdf.
6. US Dept of Health and Human Services. HRSA data warehouse: designated health professional shortage areas statistics as of July 29, 2013. US Dept of Health and Human Services [Internet]. 2013 [cited 2014 Jan 9]. http://ersrs.hrsa.gov/reportserver/Pages/ReportViewer.aspx?/HGDW_Reports/BCD_HPS A/BCD_HPSA_SCR50_Smry_HTML&rs:Format=HTML4.0.
7. Centers for Disease Control and Prevention/National Center for Health Statistics. National health interview survey, family core, sample child, and sample adult questionnaires. Centers for Disease Control and Prevention/National Center for Health Statistics [Internet]. 2012 [cited 2014 Jan 7]. http://www.cdc.gov/nchs/data/hus/2012/075.pdf.
8. American Dental Association. Dental hygienist: job description. American Dental Association [Internet]. 2013 [cited 2014 Jan 8]. http://www.ada.org/357.aspx.
9. American Dental Hygienists’ Association. Scope of practice. American Dental Hygienists’ Association [Internet]. 2012 [cited 2014 Jan 6]. http://www.adha.org/scope-of-practice.
10. Institute of Medicine. The future of nursing: focus on scope of practice. Institute of Medicine [Internet]. 2010 [cited 2014 Jan 8]. http://www.iom.edu/~/media/Files/Report%20Files/2010/The-Future-of-Nursing/Nursing%20Scope%20of%20Practice%202010%20Brief.pdf.
11. Dierick-van Daele AT, Metsemakers JF, Derckx EW, et al. Nurse practitioners substituting for general practitioners: randomized controlled trial. J Adv Nurs. 2009;62(2):391-401.
12. Eibner C, Hussey P, Ridgely MS, McGlynn EA. Controlling health care spending in Massachusetts: an analysis of options. Division of Health Care Finance and Policy [Internet]. 2009 [cited 2014 Jan 6]. Santa Monica, CA. RAND Corporation. http://ct.gov/sustinet/lib/sustinet/board_of_directors_files/resources/control_health_care_s pending_rand_08-07-09_full.pdf.
13. Moreau E, Mageau GA. The importance of perceived autonomy support for the psychological health and work satisfaction of health professionals: not only supervisors count, colleagues too! Med Care Res Rev. 2012;67(1):3-26.
14. Barker K. Women physicians and the gendered system of professions: an analysis of the Sheppard-Towner Act of 1921. Work Occupation. 1998;25(2):229-235.
15. Whittington KB. Mothers of invention? Gender, motherhood, and new dimensions of productivity in the science profession. Work Occupation. 2011;38(3):417-456.
16. American Dental Education Association. Dental hygiene total enrollment by gender: 2000-2011. American Dental Education Association [Internet]. 2012 [cited 2014 Jan 6]. http://www.adea.org/publications/tde/Documents/Dental%20Hygiene%20Total%20Enroll ment%20by%20Gender%20Table.pdf.
17. Guilford JP, Fruchter B. Fundamental Statistics in Psychology and Education. New York, NY: McGraw-Hill; 1973.
18. Baruch Y. Response rate in academic studies: a comparative analysis. Hum Relat. 1999;52(1):421-438.
19. Dempster JS. Autonomy in practice: conceptualization, construction, and psychometric evaluation of an empirical instrument. [Doctoral dissertation]. 1990. Available from ProQuest Dissertations and Theses. Ann Arbor, MI: University Microfilms International.
20. Green SB, Salkind NJ. Using SPSS for Windows and Macintosh: Analyzing and Understanding Data. 7th ed. Upper Saddle River, NJ: Pearson; 2013.
21. McCain LH. Attitudes of Virginia dental hygienists towards issues relevant to the independent practice of dental hygiene. [Doctoral dissertation]. 1993. Available from ProQuest Dissertations and Theses. Ann Arbor, MI: University Microfilms International.
22. Turner S, Ross MK, Ibbetson RJ. Dental hygienists and therapists: how much professional autonomy do they have? How much do they want? Results from a UK survey. Brit Dent J. 2011;210(10):16-22.
23. Robinson SE, Rodriguez ER, Sammons MT, Keim J. Does being in the military affect nurses’ perceptions of work life? J Adv Nurs. 1993;18(7):1146-1151.