You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The placement of posterior composites has increased as practitioners and patients have opted for tooth-colored restorations instead of amalgam restorations. In the days of amalgam restorations, a clinician would spend a significant amount of time creating the proper posterior preparation; however, the actual placement of amalgam took a relatively short amount of time and was placed with relative ease. Unfortunately, these esthetic and conservation benefits of composite restorations come at a cost of time and technique sensitivity. When placing composite restorations the clinician must take into account factors such as proper dentin bonding, cuspal deflection, and the kinetics of light-polymerization in order for patients to have successful, long-lasting restorations. If any one of these components is not achieved, a patient can experience sensitivity or a restoration can fail fairly quickly.
Adhesion
Modern adhesive dentistry started in 1955, when Buonocore discovered that phosphoric acid could be used on enamel to increase bond strength.1 The idea of using phosphoric acid on tooth structure came from an industrial process where metal was treated with phosphoric acid before paint was applied. This concept led him down a path of many research experiments until he came to the conclusion that enamel could be etched with an 85% concentration of phosphoric acid for 30 seconds.1 Over the years, this concept of enamel etching with phosphoric acid has been modified, and present-day enamel etching generally occurs with a 35% to 40% concentration in contact with enamel for 15 to 30 seconds.
While Buonocore’s concept of enamel etching led to more predictable enamel bonds, it was not until Fusayama’s work on dentin etching and bonding in 1979 when the world began to see long-term bonds being formed that were not easily susceptible to degradation. Fusayama believed that low dentin bond strengths existed because very minimal bonds were forming to the dentin smear layers after the dentin was mechanically prepared, and in order to form higher-strength bonds the smear layer must be removed to ex- pose collagen. To this end Fusayama advocated that dentin also should be etched with phosphoric acid, and the total-etch technique was born.2
Fourth Generation: Etch, Prime, and Adhesive
Fusayama’s concept of total-etching led to predictable dentin and enamel bonds, and it was this concept that ultimately led to the development of adhesives that required etching, priming, and bonding. This three-step system is commonly referred to as a fourth-generation bonding agent (Table 1). In this generation, the techniques generally involve etching enamel and dentin with phosphoric acid. Once the enamel and dentin are rinsed with water and dried to remove the etchant, a primer is applied to the treated surfaces. On enamel, the primer will have little to no effect; however, on dentin, the primer will fluff up any collagen that may have collapsed after the dentin was etched and dried. The hydrophilic nature of primer allows it to drive into dentin and return collagen to a similar height as pre-etched dentin. This primed collagen can now be infiltrated by adhesive resin and form what is known as the hybrid layer.3
The hybrid layer is an intermingling of collagen and resin, allowing for a micromechanical lock to occur between the two.4 After the hybrid layer forms, the adhesive resin is polymerized, and it is this polymerized surface that forms a barrier between the hydrophilic primer and the hydro- phobic resin that will be placed. Furthermore, the hydrophobic monomers within the adhesive resin allow a bond to form with the resin that will be placed onto it. One key advantage of fourth- generation systems is that by separating acidic hydrophilic primers and hydrophobic adhesive monomers, this generation tends to have compatibility with both self-cured and light-cured resins. This separation allows for a neutral pH of the cured surface, thus allowing for compatibility.
This generation of adhesives has been available to clinicians for more than 20 years and it has shown very good results. In fact, this generation is still considered the gold standard; when adhesives are tested today, they are still compared to this generation of adhesives. In a 13-year randomized clinical study, one fourth- generation adhesive demonstrated 94% retention of Class 5 resin restorations.5
Fifth Generation: Etch and Adhesive (Adhesive and Primer Combined)
To simplify the adhesive process, researchers created a two-step adhesive resin (Table 1). In this generation, primer and adhesive were combined into a single bottle and placed onto enamel and dentin after they were etched with phosphoric acid and rinsed. The combined primer and adhesive is responsible for creating a hybrid layer by using its hydrophilic properties to penetrate into collagen. Once cured, the surface becomes hydrophobic and can then bond to hydrophobic resin materials.
In theory, this generation of adhesives was to offer simplicity for the clinician; however, this generation actually increased technique sensitivity in many ways. By combining the primer and adhesive resin into a single bottle, the concept of moist bonding became very important. In fourth-generation adhesives, if the dentin was accidently over-dried after etching, the primer had the ability to remoisten the collagen with its hydrophilic properties before the adhesive resin was introduced. This ability to rehydrate the collagen offered some technique forgiveness.
In fifth-generation adhesives, one must pay close attention to the directions prescribed by the manufacturer because each system is different in terms of maximizing adhesive bonds. In some systems it is recommended that two coats of the combined primer and adhesive are placed, while in others only one coat is needed. In essence, the first coat moistens the dentin and the second coat allows penetration and formation of a hybrid layer.
In other systems that tend to be more filled, only a single coat needs to be placed. Once cured, this generation of adhesives is compatible with all light- cured resins; however, this generation has shown some incompatibility with self-cure and dual-cure resins.6 The reason for incompatibility is that the oxygen-inhibited layer that is formed after curing tends to be too acidic and neutralizes the tertiary amines in self- and dual-cure composites. To com- bat this issue, many manufacturers have created dual-cure activators to be used in conjunction with the adhesive. The dual-cure activators essentially raise the pH of the oxygen-inhibited layer to al- low for compatibility. This generation has shown comparable results to fourth-generation adhesives in terms of microleakage and marginal staining, and is a viable alternative for light-cured restorations.7,8 Clinicians must be aware that postoperative sensitivity can occur when etching is involved and when proper techniques are not followed. These issues can be magnified in preparations where deeper dentin is involved.9
Sixth Generation: Acidic Primer and Adhesive
To combat the technique sensitivity issues associated with the etching of dentin researchers searched for a solution that would remove traditional phosphoric-acid etching and rinsing. To this end, two-component self-etching adhesives were introduced into the market (Table 1). The first component is a hydrophilic acidic monomer that is used to prime the dentin and roughen the enamel surface. The second component is a hydrophobic bonding resin similar to those used in fourth-generation adhesives. The big benefit of a system like this is that the clinician is not guessing whether the dentin is too wet or too dry. If the dentin is never etched with phosphoric acid, the smear layer is never completely removed; therefore, the collagen does not collapse. In addition, the dentinal tubules stay at least partially plugged with the smear layer. This mechanism of action, in theory, should lead to higher dentin bonds and help mitigate sensitivity. Anecdotally, practitioners have reported less sensitivity with self-etch adhesives; however, a multitude of factors can lead to sensitivity and these anecdotal findings are not consistent with the literature.10 On the other hand, very high and stable dentin bond strengths have been noted in the literature using sixth-generation adhesives.11
One concern of this generation has been centered on the ability of the acidic primer to properly etch enamel. If enamel is not etched properly, marginal seal breakdown can occur and staining can become visible.12 To this extent the primer in sixth-generation adhesives has been developed with various levels of acidity. Primers are generally classified into categories of strong (pH < 1), intermediately strong (pH ≈ 1.5), mild (pH ≈ 2), and ultra-mild (pH ≥ 2.5).13 The proper balance of acidity is one that allows a sufficient etching of enamel to occur without causing deleterious effects on dentin. When an acid is too strong, more calcium and phosphate ions are dissolved. These dissolved ions are not rinsed away by water in a self-etching protocol and they can impact the collagen layer, which may explain lower dentin bonds in the literature when strong acidic primers are used.14
An ideal material would offer high dentin bond strengths as well as high enamel bond strengths. Unground enamel has been notoriously difficult to bond to, and chemical etching with phosphoric acid is recommended in the vast majority of studies. On the other hand, if a primer can at least be effective on ground enamel, a significant upside is possible. To accomplish this, some adhesives have capitalized on creating a primer that is acidic enough to etch enamel similarly to phosphoric acid, yet not be so aggressive as to impact dentin negatively.
One additional benefit of this generation is that these adhesives tend to be compatible with both dual-cure and self-cure resins. This is especially important if a dual-cure resin cement or core buildup is being used.
Seventh Generation: Acidic Primer and Adhesive in a Single Bottle
In this generation of adhesives, manufacturers attempted to create simplicity in the technique by combining everything into a single bottle (Table 1). In this protocol, phosphoric acid is not needed because these adhesives allow bonds to be formed to both dentin and enamel. Similar to sixth-generation adhesives, this generation is also classified as self-etch. However, it is accomplished in one bottle. Combining both functions in a single bottle is quite difficult, as hydrophilic and hydrophobic monomers must be mixed together without diluting the effectiveness of one another. At the same time, the solution must also be at least mildly acidic to form a bond to enamel. One concern with this generation of adhesives has been that they tend to be too hydrophilic, and water is actually drawn out of the dentinal tubules and pulled back into the adhesive layer after initial evaporation.15 This phenomenon can be deleterious to maintaining long-term bond strengths. Additionally, because all components are in one bottle, it has been reported that a high residual level of acidity may exist after placement and that this acidity does not allow proper bonds to be formed with self- and dual-cure materials materials.16 This generation had the proper intent of creating simplicity for the clinician; however, this multifunctional chemistry is difficult to accomplish and further research is needed.
Universal Adhesives
This generation of adhesives (Table 1) has moved away from the traditional numerical nomenclature and a significant amount of confusion exists with respect to defining universal adhesives. To date there has been no consensus statement reached on what the definition should be and each manufacturer has essentially created their own classification system. Some manufacturers claim that a universal adhesive is any adhesive that is in a single bottle and can be used in a total-etch, self-etch, or selective-etch technique. Other manufacturers claim that it is any adhesive that is in single bottle or packet and can be used with light- and dual-cure resins without the need for a separate dual-cure activator. Finally, some manufacturers do not restrict their universal definition to single-bottle systems; rather, they state that universal means any adhesive that can be used across a multitude of substrates ranging from enamel to ceramic, in addition to being compatible with all forms of resins, as well as potential etching techniques.
Regardless of how adhesives are defined, it is important for clinicians to understand that each adhesive has a specific set of instructions to optimize its chemistry. One must pay close attention to these facts and understand that techniques amongst various adhesives are not necessarily interchangeable.
Composite
Achieving a proper bonding interface is a critical step in achieving a successful posterior composite restoration. The next critical component is the actual placement of the composite restoration. It is this step that has historically required a tedious process of placing incremental layers of composite until the entire restoration is built to form. This concept has been advocated throughout the world to decrease the chance of cuspal deflection caused by resin shrinkage, as well as to predictably polymerize each small increment of resin that has been placed. This process of placing composite has generally been successful; however, issues still exist with this technique. One concern historically has been the time required to incrementally place posterior composites;17 however, concerns such as voids between layers are also evident in the literature.18 In the ideal world, a material could be placed in bulk and have no negative effects.
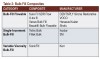
Over the last 10 years, bulk-filling techniques have come more in vogue as new materials have been developed with improved properties (Table 2).19 If these materials can work as claimed, a significant paradigm change in posterior composite dentistry may be possible. During this time, bulk-fill composites have essentially been separated into two categories. The first category offered bulk-fill resins that were to be used like a base, with a capping composite placed on top. In the second category, a single material was to be used throughout the entire restoration.
Bulk-Fill Flowable
In this category of materials, essentially a 4-mm layer of a low-viscosity resin is placed into the cavity preparation. The low-viscosity properties of the resin allow it to coat the preparation and minimize any voids. Once this layer is put in place, it is polymerized before a capping composite is placed on top. These bulk-fill flowable composites tend be more translucent and do not have the physical properties of traditional composites. They are not meant to withstand occlusal load; therefore, a traditional composite is placed on top to enhance esthetics and with- stand the opposing occlusion. Traditionally, flowable composites exhibited high shrinkage parameters; however, this category of bulk-fill materials has been shown to reduce shrinkage stress. In fact, the literature today shows that bulk-fill flowable composites may actually reduce cuspal deflection compared to incremental filling techniques.20
Single-Increment Bulk Fill
Bulk-fill flowable composites have shown great promise and have substantially decreased placement time; however, the ideal material would be one where a single increment of composite can be placed with all the physical properties to withstand occlusal load. To address this point, manufacturers have released high-viscosity materials that can be placed in a single increment and, after polymerization, have very good physical properties. The only issue with this category is that adaptation of a higher-viscosity material to the preparation can be difficult to accomplish compared to materials that have greater flow characteristics. Adaptation can be further complicated compared to traditional incremental filling as a light, condensing pressure must be transmitted across a greater mass of material. In a recent study comparing traditional incremental layering, a bulk-fill flowable with a capping layer, a single-increment higher-viscosity bulk fill, and a bulk fill with variable viscosity, the single-increment higher-viscosity bulk fill had the highest proportion of marginal gaps.21 To combat this issue, many clinicians will place a traditional flowable composite first and, after polymerization of this layer, a higher-viscosity bulk fill is placed.
Variable-Viscosity Bulk Fill
A third option within the bulk-fill arena is to use a variable-viscosity material. A truly ideal material has the ability to flow nicely across the depths of the cavity preparations, yet gains body back, so that the restoration can be sculpted appropriately. This type of material is available to clinicians today. The variable viscosity is achieved by using sonic energy, and combines the best aspects of a flowable material with a medium- to high-viscosity material. The system uses a unique, proprietary, highly filled composite and pairs it with a handpiece that delivers sonic energy. As the energy is applied, the viscosity of the material drops by 84%, which allows it to adapt intimately to the prepared cavity form. As the energy is removed from the material, the composite gains viscosity back over a roughly 20-second span and returns to a consistency similar to traditional nanohybrid composites. During this time, the practitioner can easily sculpt the restoration to achieve proper form and harmony with the adjacent tooth structure. This technique allows practitioners to restore teeth in a fraction of the time compared to traditional layering techniques. The material can be placed in increments up to 5 mm, so that the vast majority of preparations can be restored in a true single increment versus worrying about capping layers or initial flowable composite layers. Over the last 2 to 3 years, researchers have found that this variable-viscosity material is at least as good as the traditional incremental technique,22 but can be placed in a fraction of the time.
Light Polymerization
Numerous resin restorations are being placed every year, and this trend will continue to grow as more patients seek esthetic restorations. Practitioners must be cognizant of the fact that polymerizing restorations properly is incredibly important, being that inadequate polymerization adversely affects the resin’s physical properties, reduces bond strength, increases wear and breakdown at the margins, decreases biocompatibility of the resin restoration, and increases bacterial colonization of the resin in the restoration.23 The fact that blue light may be coming out of the curing light by no means indicates that a restoration will be polymerized properly; rather the light coming out must have the correct irradiance and spectral emission.
Irradiance is the radiant power striking a specific area,24 and spectral emission is the wave- length of light coming out of the curing unit. With respect to resins that are used in dentistry, camphorquinone (CQ) is the primary photoinitiator,25 and curing lights must emit light that can activate CQ. In addition, a minimum of 400 mW/cm2 of irradiance must be delivered to light-activated composite in order for polymerization to occur.26
The facts mentioned here are even more critical for bulk-fill restorations that are cured in mass. The most critical part of a restoration is not the top surface that is close to the light tip; rather it is the area that is going to be cured at the farthest distance from the tip. To accomplish this task, it is best to have a light that is very well collimated. Such lights will maintain proper energy at their periphery and will not expand greatly in diameter as they move further away from their source. On the other hand, poorly collimated lights will expand in diameter the further they move away from their source, and the energy on the periphery may not reach the critical threshold of 400 mW/cm2.
Many manufacturers tout power as the primary means by which a curing light should be selected. Unfortunately, power alone does not translate into effective curing. The statistic that is more relevant is effective irradiance. Effective irradiance is the power per unit area that is effectively able to inter- act with CQ. If a light has a high power, but does not activate CQ, the extra power is irrelevant. The power that matters is the power that will actually lead to polymerization.
Overall Success
The success of posterior composites is truly multifactorial. However, today materials and technologies exist that allow efficient and predictable restorations to be placed. Clinicians have choices in their techniques, but they can be very comfortable in the fact that simplicity in material application is not compromising their clinical results. In fact, today’s simplified adhesive materials are performing similarly to materials that have historically been the gold standard, and bulk-fill materials are performing equally to time-consuming incremental layering techniques. A new paradigm in dentistry is upon us where simplicity can be in parallel with success.
ABOUT THE AUTHOR
Parag R. Kachalia, DDS, is the vice chair of Preclinical Education, Technology & Research in the Department of Integrated Reconstructive Dental Sciences at the University of the Pacific Arthur A. Dugoni School of Dentistry. He also has a private practice in San Ramon, California.
REFERENCES
1. Buonocore M. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34(6):849-853.
2. Fusayama T, Nakamura M, Kurosaki N, Iwaku M. Nonpressure adhesion of a new adhesive restorative resin. J Dent Res. 1979;58:1364-1370.
3. Van Meerbeek B, Inokoshi S, Braem M, Morphological aspects of the resin-dentin interdiffusion zone with different dentin adhesive systems. J Dent Res. 1992;71:1530-1540.
4. Nakabayashi N, Kojima K, Masuhara E. The promotion of adhesion by the infiltration of monomers into tooth substrates. J Biomed Mater Res. 1982;16:265-273.
5. Peumans M, De Munck J, Van Landuyt KL, et al. A 13- year clinical evaluation of two three-step etch-and-rinse adhesives in non-carious class-V lesions. Clin Oral Invest. 2012;16:129-137.
6. O’Keefe KL, Powers JM. Adhesion of resin composite core materials to dentin. Int J Prosthodont. 2001;14(5):451-456.
7. Schmitt DC, Lee J. Microleakage of adhesive resin systems in the primary and permanent dentitions. Pediatr Dent. 2002;24(6):587-593.
8. Castelnuovo J, Tjan AH, Liu P. Microleakage of multi-step and simplified-step bonding systems. Am J Dent. 1996;9:245-248.
9. Opdam NJ, Feilzer AJ, Roeters JJ, Smale I. Class I occlusal composite restorations: In vivo post-operative sensitivity, wall adaptation, and microleakage. Am J Dent. 1998;11(5):229-234.
10. Perdigão J, Swift EJ. Critical appraisal: post-op sensitivity with direct composite restorations. J Esthet Restor Dent. 2013;25:284-288. J Esthet Restor Dent. 2013;25:284-288.
11. Peumans M, De Munck J, Van Landuyt KL, et al. Eight-year clinical evaluation of a 2-step self-etch adhesive with and without selective enamel etching. Dent Mater. 2010;26:1176-1184.
12. Pashley DH, Tay FR. Aggressiveness of contemporary self-etching adhesives. Part II: etching effects on un-ground enamel. Dent Mater. 2001;17(5):430-444.
13. Van Meerbeek B, Peumans M, Poitevin A, et al. Relationship between bond-strength tests and clinical out- comes. Dent Mater. 2010;26:e100-e121.
14. Van Landuyt K, Kanumilli P, De Munck J, et al. Bond strength of a mild self-etch adhesive with and without prior acid-etching. J Dent. 2006;34:77-85.
15. Van Landuyt KL, De Munck J, Snauwaert J, et al. Monomer-solvent phase separation in one-stepself-etch ad- hesives. J Dent Res. 2005;84(2):183-188.
16. Sanares AME, Itthagarun A, King NM, Tay FR, Pashley DH. Adverse surface interactions between one-bottle light- cured adhesives and chemical-cured composites. Dent Mater. 2001;17:542-546.
17. Abbas G, Fleming GJ, Harrington E, et al. Cuspal movement and microleakage in premolar teeth restored with a packable composite cured in bulk or in increments. J Dent. 2003;31:437-444.
18. Campos EA, Ardu S, Lefever D, et al. Marginal adaptation of class II cavities restored with bulk-fill composites. J Dent. 2014;42:575-581.
19. Leprince JG, Palin WM, Hadis MA. Progress in dimethacrylate-based dental composite technology and curing efficiency. Dent Mater. 2013;29:139-156.
20. Moorthy A, Hogg CH, Dowling AH, et al. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent. 2012;40:500-505.
21. Agarwal RS, Hiremath H, Agarwal J, Garg A. Evaluation of cervical marginal and internal adaptation using newer bulk fill composites: An in vitro study. J Conserv Dent. 2015;18:56-61.
22. Bayraktar Y, Ercan E, Hamidi MM, Çolak H. (2016), One-year clinical evaluation of different types of bulk-fill composites. J Investig Clin Dent. doi: 10.1111/jicd.12210.
23. Seth S, Lee CJ, Ayer CD. Effect of instruction on dental students’ ability to light cure a simulated restoration. J Can Dent Assoc. 2012;78:c123.
24. Kirkpatrick, SJ. A primer on radiometry. Dent Mater. 2005;21:21-26.
25. Yu Q, Nauman S, Santerre JP, and Zhu S. UV photopolymerization behavior of dimethacrylate oligomers with camphorquinone/amine initiator system. J Poly SC.
2001;82:1107-1117.
26. Rueggeberg, FA, Caughman WF, Curtis JW. Effect of light intensity and exposure duration on cure of resin composite. Oper Dent. 1994;19:26-32.