You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Anterior single-tooth implants are an integral part of any contemporary dental practice. Each opportunity to replace a tooth with an implant requires meeting the interdependent challenges of the biologic, functional, and esthetic demands of anterior tooth replacement. The principles of osseointegration, the fundamentals of esthetics, and concerns for occlusion and function are elements for implant-supported crown success. Clinical decision-making, particularly implant placement decisions, affect each of these elements. The importance of esthetics is underscored by the interwoven relationship between soft-tissue architecture and underlying osseous form.
Osseointegration represents the formation of a bone-to-implant interface, one that is sufficient to meet the function of the implant and whose formation is strategically located to support the overlying mucosa, providing both health and esthetics for the implant-supported restoration (Table 1). Any decision to place an implant for anterior tooth replacement demands sufficient bone to reproducibly provide osseointegration. While there is no specific minimal dimension to achieve reproducible osseointegration success, implant dimensions approximately 3.2 mm to 3.5 mm in diameter and 8 mm to 11 mm in length are commonly used successfully. The minimal volume of bone needed to house the implant is also not well defined; however, providing 1 mm of bone surrounding the implant and 1.5 mm between the implant and adjacent teeth have been suggested as minimal dimensions. The assurance of primary stability, the key determinant of osseointegration success, is dependent on many factors including the volume and density of targeted bone. Reproducible osseointegration success likely requires a minimal bone volume represented by a cylinder of 6 mm in diameter and at least 6 mm in length.
Esthetics is a crucial concern for anterior dental restorations. In addition to the aforementioned volumetric osseous support of osseointegration, the location of the implant in the alveolus must be further considered in terms of esthetics. The relationship of the implant, the implant/abutment interface, and the enveloping bone are considered to be critical determinants of the soft-tissue form surrounding the dental implant crown. One approach to assuring the esthetic integration of the implant with existing teeth is to attempt to recapitulate the peri-coronal tissue architecture by the peri-implant mucosa that is formed at the implant (Figure 1). This approach demands that bone is present in the crestal region of the alveolus to support the soft-tissue form at the buccal aspect of the implant. Achieving reproducibly esthetic implant crowns requires management of these important relationships.
Dental implant placement in the anterior maxilla may involve placement within the healed alveolar ridge without grafting to permit alteration of implant orientation. In such cases, the implant is aligned with the original tooth root and often requires a cement-retained crown to avoid esthetic complications of the retaining screw. The intentional placement of implants in the maxillary anterior alveolus to provide for a screw-retained crown requires careful planning. Because implant components (abutments, abutment screws) have defined dimensions, the location of the implant must be calculated in relationship to these component dimensions. When considering phonetics, it is also clear that anterior tooth position is critical to success. Contemporary investigations suggest that the non-axial loading incurred by implants does not represent added risk to osseointegration. Placement for intended screw retention must carefully account for abutment dimensions and impingement upon occlusion, speech, and comfort.
The Rules of Six
In order to manage the different clinical goals described above, a rigorous approach to treatment planning and implant placement is required. A reproducible and simple approach is advantageous. The “Rules of Six” represents five diagnostic targets and a single therapeutic guideline useful in directing clinical success and preventing common complications.
For a simple, successful single-tooth dental implant, the clinician must identify or create bone volume with the following characteristics:
1. 6 mm of inter-radicular space.
2. 6 mm bucco-lingual osseous dimension.
3. 6 mm in “length” at minimum.
4. There must be 6 mm of inter-occlusal distance to permit inclusion of ideal components and prostheses without functional or esthetic interference.
There can be no more than a distance of 6 mm from the interproximal contact point to the bone crest.
Implants must be placed in specific orientation to the soft-tissue reference of the gingival zenith. Specifically, the implant/abutment interface should be located 3 mm apical and displaced 2 mm palatal to the gingival zenith of the planned crown.
These six guidelines can provide clinically reproducible single-implant success, esthetics, and stability.
Architecture of Anterior Single-Tooth Implant Site and the Rules of Six
The typical minimal mesiodistal dimension that may be considered for simple single-tooth replacement of an anterior tooth is 6 mm. This may not seem to be an impediment to implant placement; however, several common anatomic situations are often encountered. While the typical dimension of a lateral incisor is greater than 6 mm in the mesiodistal dimension, teeth are often lost without immediate placement, and the bound edentulous space may be reduced. Natural tooth crowding with rotation may result in less than 6 mm of mesiodistal dimension. Another concern is proximal root convergence leading to less than 6 mm of space for implant placement despite the dimension available for the crown. Finally, lateral incisor agenesis that is treated by orthodontics may not always provide 6 mm of space for implant placement or may result in proximal root convergence. There must exist 6 mm of mesiodistal bone dimension between adjacent teeth to permit an implant (> 3.5 mm in diameter) to be placed with greater than 1 mm of bone at mesial and distal interproximal locations (Figure 2 and Figure 3). The advent of narrow implants (eg, 3 mm) provides a new opportunity to address smaller (approximately 5 mm) mesiodistal dimensions.
The minimal buccolingual dimension that should be considered acceptable for simple single-tooth replacement of an anterior tooth is 6 mm. This is challenging for clinicians because estimation of this dimension by bone sounding is technically difficult, and not all communities have broad access to volumetric imaging (such as cone beam computed tomography [CBCT]) to assess this dimension. The buccolingual dimension is further challenging because residual alveolar ridges generally experience resorption. A recent systematic review revealed there was a loss of width of approximately 2.5 mm to 4.5 mm when no intervention was performed and resorption was not prevented.2 It is known that a majority of tissue loss occurs at the buccal aspect of the alveolus, further impacting esthetics.3,4 The assurance that 6 mm of alveolar bone is present permits the placement of a dental implant with approximately 1 mm of bone enveloping the buccal and lingual aspects of the endosseous implant without the need to explore bone augmentation.
The retention of an implant crown requires an abutment with a prescribed dimension. For a cement-retained crown, the abutment should possess a transmucosal dimension that permits biologic width formation (minimally 2 mm)5 and supracrestal axial walls, which ideally retain the crown (4 mm; total 6 mm). If the crown is to be screw-retained, the abutment and abutment screws available should typically possess minimal dimensions of approximately 4 mm. For such screw-retained crowns, the orientation of the implant may require augmentation of the buccal alveolar bone. In making such plans, it is important to establish that there is 6 mm of space from the crest of bone to the opposing dentition for an acceptable crown to be constructed in this manner. Although it is possible to gain additional vertical space by increasing the depth of implant placement, the related buccal bone and mucosal resorption associated with deep implant placement virtually eliminates this option for anterior dental implants.6
Additional attention must be paid to the osseous architecture related to the adjacent teeth, as this controls interproximal tissue form.7 The crest of healthy bone is 4.5 mm to 5 mm from the contact point between anterior teeth8; a similar 5-mm distance from the contact point to the bone crest has been measured between an implant and natural tooth. An important and additional rule to guide esthetic implant outcomes is that the adjacent tooth should possess interproximal bone levels no further than 6 mm from the natural tooth contact point (Figure 4 through Figure 6). While the ideal distance is justifiably indicated to be 5 mm, this 6-mm rule establishes a point at which marked interproximal tissue deficiencies and asymmetry will not be overcome.
Implants of 6 mm in length are available for use in clinical dentistry. While there must be at least 6 mm of length available for the implant, the use of short implants may not adequately provide sufficient stability in sockets or for immediate provisionalization procedures. Given the anatomy of the human anterior maxillary teeth and the alveolus, bone dimensions typically enable implants of at least 11 mm in length in this region of the mouth. It is typical for the anterior maxilla that bone accepting 8-mm to 11-mm long implants will be available.
To summarize the anatomical requirements for the successful placement of a dental implant, the dentoalveolar anatomy of the edentulous site should provide at least 6 mm of bone in three dimensions, and there should be 6 mm of space from the ridge crest to the opposing dentition. The adjacent tooth interproximal contact point should not be more than 6 mm from the bone crest. These anatomical guidelines provide opportunities for reproducible clinical success (Figure 7 through Figure 9).
Diagnostic Procedures Needed to Deploy the Rules of Six
Any dental therapy requires a comprehensive assessment of the patient that includes review of the health history and current medical status, exploration of the dental health history, and assessment of oral diseases. Tooth replacement by any means including implant therapy should not be performed without risk assessment and control of oral infectious and oncologic diseases. In particular, periodontal diseases and dental caries must be demonstrably controlled. Factors and conditions representing risk to existing teeth and eventual implant restorations—including diet, habits, bruxism, and xerostomia—must be identified.
Clinical Examination
Dental implant treatment planning must focus on the architecture of the bound edentulous space. This may be divided into two separate areas of concern. As mentioned above, one is the condition of the adjacent teeth and, in particular, the level of connective tissue attachment that determines the ultimate location of papilla at the single-implant crown (Figure 10 and Figure 11). The other is the condition of the alveolus within the bound edentulous space. The extent of resorption in the vertical and horizontal direction must be considered (Figure 12). There exist several classification systems for this (eg, Seibert, Allen) that identify the presence or extent of alveolar and horizontal alveolar bone deficiency. Pragmatically, clinical resolution requires that the position of the planned implant crown be identified in the context of the alveolar bone (discussed below).
Mounted Study Casts
The exploration of this architecture is only fully achieved by evaluation of study casts that clearly reveal the detailed anatomy of the alveolus and the peri-coronal tissues. Study casts should be mounted in maximum intercuspal position for the complete treatment planning of single-tooth dental implants. Mounted casts enable estimation of the required 6 mm of space between the ridge crest (approximately 2 mm submucosal) and the opposing tooth and measurement of the mesiodistal interdental distance. The orientation of the implant in the alveolus should neither interfere with the required occlusion nor should it obviate the placement of an esthetic crown (eg, excessively buccal orientation). This can be revealed through the diagnostic waxing process. Encroachment of opposing teeth into the bound edentulous space may suggest the need for possible adjustment or orthodontic movement of the antagonist. When excellent study casts are mounted, it is possible to: estimate bone volume; measure bound edentulous space inter-tooth dimensions; measure inter-arch dimensions; and evaluate alveolar ridge/tooth relationships (superseding resorbed ridge classification) (Figure 13 through Figure 16).
Radiographs
The intent of making radiographs for dental implant planning is to provide sufficient information concerning the osseous region of interest to permit safe and successful dental implant placement. The choice of radiographic imaging for a single-tooth implant in the anterior maxilla should be made on an individual basis that weighs the radiation risk and the benefits of information gained.9
In the context of the Rules of Six, the single periapical radiograph offers several advantages. Within a periapical radiograph, the essential features of a single-tooth-bound edentulous space can be observed. In addition to noting any contraindicating potential pathology, the periapical radiograph can indicate bone quality and bone quantity. A periapical radiograph can demonstrate the inter-radicular dimension. It also demonstrates the level of osseous attachment at adjacent teeth, suggesting the presence of clinical loss of attachment or therapeutic recession. This radiographic representation is ideal for measuring the distance from the interproximal contact to the bone crest (Figure 4). It will further suggest adjacent tooth health and status (eg, periapical lesions, fractures, existing endodontic therapy, quality of post-and-core restorations, recurrent caries). Unfortunately, periapical radiographs do not demonstrate these structures in the saggital (or coronal) planes.
Panoramic radiographic imaging is common in dental practice. This technique is extremely valuable in evaluating the patient. However, in the case of the single anterior dental implant, the artifacts presented by many panoramic radiographic images—as well as the quality or resolution of the image with regard to evaluating adjacent tooth bone levels—may be limited.
Volumetric imaging offers several advantages, including the 3-dimensional (3-D) assessment of the residual alveolar ridge, as well as sufficient resolution of the adjacent teeth to assess bone levels and periapical lesions. CBCT imaging offers access to volumetric imaging with the advantage over medical CT imaging of reduced radiation dose.10 A CBCT image permits the careful measurement of mesiodistal osseous dimension, buccolingual osseous dimension, and occlusogingival dimension of the alveolus, as well as the edentulous space (Figure 17 through Figure 19). The Rules of Six are readily interpreted from CBCT images. Using the Rules of Six, however, does not require that a CBCT image be produced.
The 3/2 Rule: Implant Planning, Decision Making, and Implant Placement
The last of the Rules of Six is the 3/2 rule, which describes the spatial relationship of the implant/abutment interface to the soft-tissue reference point, the gingival zenith.11 The implant/abutment interface exists at the bone crest. The implant/abutment interface should be 3 mm apically displaced from the zenith. It should be displaced 2 mm palatally from the zenith (Figure 20). The apical displacement reflects knowledge of the biologic width, which is formed along a dental implant abutment (approximately 3 mm including the sulcus). The palatal displacement reflects understanding of peri-implant mucosal stability and its relationship to buccal peri-implant tissue thickness. Peri-implant tissues of approximately 2-mm thickness (bone and soft tissue) facial to the implant abutment display stability when compared to thin peri-implant tissues.12
Deploying the 3/2 rule requires that the location of the gingival zenith be determined as a prerequisite step in treatment planning (Table 2). Zenith-directed planning is achieved using the study casts and the process of diagnostic waxing. The location of the residual alveolar ridge may or may not conform with the desired location of the cervical contour of the crown and suggests that subtractive or regenerative procedures are necessary for optimal dental esthetics. Bone must also be located at a point 3-mm apical and 2-mm palatal to the planned gingival zenith. The completed diagnostic waxing must be oriented to available bone. This can be done preoperatively or inter-operatively by bone sounding. However, a powerful and simple technique is to include the proposed crown contour within the CBCT image by use of a radiographic template.
Imaging of the proposed crown contour in the volumetric image permits the linear measurement of the located zenith to the bone crest in three dimensions (Figure 18). Thus, the desired 3-mm apical displacement and 2-mm palatal displacement of the implant/abutment interface can be evaluated. This rule serves as both a therapeutic guide—determining where the implant should be placed—as well as a diagnostic guide—determining whether there is enough bone to permit ideal implant placement. When viewing the linear relationship of the existing bone crest to the gingival zenith, the presence or absence of bone at this location offers direction in clinical decision-making. If ideal esthetics is desired and insufficient bone volume is observed, then the decision to perform bone augmentation can be made. If there is excess bone, the decision to place the implant in a subcrestal position can and should be made.
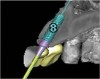
Implant placement according to the 3/2 rule involves using a surgical guide that reveals the location of the gingival zenith. Gingival zenith-oriented planning begins with a diagnostic waxing that identifies the planned tooth contour and related soft-tissue form. This information is transferred to the radiographic assessment and surgical placement using a thermoplastic index that is carefully trimmed to the zenith. In this way, the surgical placement can be monitored and directed from the location of the gingival zenith (Figure 21 through Figure 25). The intended result is placement of the implant/abutment margin 3-mm apical and 2-mm palatal to the clinical landmark. Careful fabrication of the provisional crown guides tissue formation and results in properly developed soft-tissue form surrounding the final implant crown (Figure 25).
It is further possible to manage zenith-directed planning using surgical guidance through CAD/CAM guides constructed from volumetric imaging of the site. Whether or not the implant is placed in a healed ridge or in an extraction socket and by flapped or flapless surgical procedures, the gingival zenith can be localized, and the position of the implant in the socket or within the healed ridge can be correctly located in relationship to this restorative landmark.
Summary
A set of rules for treatment planning of single-tooth implants has been proposed. A common 6-mm distance makes the rules easily recalled. The minimal mesiodistal and buccolingual dimension of the residual alveolar ridge, the minimal interocclusal distance, and the maximal interproximal contact point to bone distance each approximate 6 mm for an acceptable clinical result. Major deviations from these acceptable reference dimensions may lead to clinical complications, implant dehiscence, and esthetic difficulties. The final rule, the 3/2 rule, assures the placement of an implant within bone at a location that supports lasting esthetics.
References
1. Martin WC, Morton D. Implant Therapy in the Esthetic Zone – Single Tooth Replacements. In: Buser D, Belser U, Wismeijer D, eds. ITI Treatment Guide. Vol 1. Quintessenz Verlag; 2007.
2. Morjaria KR, Wilson R, Palmer RM. Bone healing after tooth extraction with or without an intervention: a systematic review of randomized controlled trials. Clin Implant Dent Relat Res. 2012 Mar 8. doi:10.1111/j.1708-8208.2012.00450.x. [Epub ahead of print]
3. Van der Weijden F, Dell’Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. J Clin Periodontol. 2009;36(12):1048-1058.
4. Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005;32(2):212-218.
5. Hermann JS, Buser D, Schenk RK, et al. Biologic width around titanium implants. A physiologically formed and stable dimension over time. Clin Oral Implants Res. 2000;11(1):1-11.
6. Zetu L, Wang HL. Management of inter-dental/inter-implant papilla. J Clin Periodontol. 2005;32(7):831-839.
7. Choquet V, Hermans M, Adriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72(10):1364-1371.
8. Kois JC, Kan JY. Predictable peri-implant gingival aesthetics: surgical and prosthodontic rationales. Pract Proced Aesthet Dent. 2001:13(9):691-698.
9. Angelopoulos C, Aghaloo T. Imaging technology in implant diagnosis. Dent Clin North Am. 2011;55(1):141-158.
10. Ganz SD. Cone beam computed tomography-assisted treatment planning concepts. Dent Clin North Am. 2011;55(3):515-536.
11. Cooper LF. Objective criteria: guiding and evaluating dental implant esthetics. J Esthet Restor Dent. 2008;20(3):195-205.
12. Evans CD, Chen ST. Esthetic outcomes of immediate implant placements. Clin Oral Implants Res. 2008;19(1):73-80.
About the Authors
Lyndon F. Cooper, DDS, PhD
Stallings Distinguished Professor
Department of Prosthodontics
University of North Carolina School of Dentistry
Chapel Hill, North Carolina
Oliver C. Pin-Harry, DDS, MS
Adjunct Assistant Professor
Department of Prosthodontics
University of North Carolina School of Dentistry
Chapel Hill, North Carolina
Private Practice,
Burlington, Ontario, Canada