You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
General anesthesia is a drug-induced state that is characterized by an absence of perception to all sensations. In 1920, Guedel described ether anesthesia according to four stages, each of which reflects greater depression of brain function: Stage I—analgesia; Stage II—delirium; Stage III—surgical anesthesia; and Stage IV—medullary paralysis and death. Today, these stages are merely of historical interest; they are not observed reliably when modern intravenous or inhalation agents and techniques are used. The so-called anesthetic stages are too unpredictable and inconsistent to be attributed to modern-day general anesthetics.
Performance of surgery usually requires an immobilized patient who is amnesic for the procedure and does not exhibit an excessive autonomic response to surgical stimulation (blood pressure and heart rate). Most anesthesiologists agree that the anesthetic state reflects a collection of component changes in behavior and perception. These components include immobilization, unconsciousness, and attenuation of autonomic responses to noxious stimulation.1,2 Many of the agents classified by convention as general anesthetics do not accomplish all of these components. The inhalation agents come closest but only at doses that depress the brain to such a degree that vital functions become jeopardized. The term anesthetic is used spuriously when potent sedative-hypnotics or opioids that produce only one component of complete general anesthesia are described. For example, thiopental provides hypnosis, but a surgical stimulus evokes autonomic and somatic reflexes that confirm absence of analgesia and immobilization. For these reasons, it is most common to use combination regimens in providing general anesthesia to induce unconsciousness with a potent sedative-hypnotic or inhalation agent, provide analgesia with an opioid, and produce muscle relaxation with the use of a neuromuscular blocking agent.
INHALATION ANESTHETICS
Properties
The inhalation agents are most deserving of the title, general anesthetics. These are excellent hypnotics, and, at higher concentrations, they provide varying degrees of analgesia and skeletal muscle relaxation. Although the mechanism for their anesthetic effect is unresolved, influences are directly related to their tension (partial pressure) in brain tissue. This follows an equilibration between tensions in the inspired gas, the alveoli, and arterial blood.
Uptake, Distribution, and Elimination
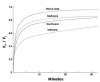
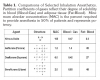
Unlike more common drug solutions, gases absorb and distribute as the result of pressure gradients and equilibrate when tensions of inspired gas equal those in alveoli, blood, and tissues. Gases that have low solubility in blood and adipose tissue will achieve tensions and equilibrate more rapidly. This tension in blood provides the driving force for inhalation agents to enter the brain, where their anesthetic action occurs. Values provided in Table 1 illustrate that nitrous oxide has very low solubility and, therefore, achieves equilibration most rapidly. For this reason, nitrous oxide has the fastest onset among inhalation agents (Figure 1).
This same principle applies to elimination of anesthetic gases, only in reverse. When administration of anesthetic gas is discontinued, alveolar tension is washed out, and equilibration proceeds from tissues to venous blood and to alveoli for expiration. Any elimination attributed to biotransformation is negligible for the most widely used agents. Therefore, inhalation anesthetics that have the lowest partition coefficients exhibit the most rapid onset and termination of effects, which renders them most suitable for cases that require intermittent alterations in anesthetic depth.1-3
Minimum Alveolar Concentration
The dose of an inhaled anesthetic gas is expressed as its percentage in the inspired mixture. In an effort to compare the relative potencies of anesthetic gases, anesthesiologists have accepted a measure known as MAC, or minimum alveolar concentration. This represents the percentage or concentration of the gas at 1 atmosphere that renders 50% of patients unresponsive to a surgical stimulus. It is analogous to the ED-50 (effective dose for 50% of patients) expressed in milligrams for other drugs. Nitrous oxide is clearly the least potent of the anesthetic gases, having a MAC of 104. This was extrapolated from studies conducted in a hyperbaric chamber because its MAC cannot be achieved at normal atmospheric pressure. The MAC determinations for various agents are listed in Table 1 and were determined in patients who were 21 to 65 years of age. It is significant that many variables can alter the MAC in a given patient. Some of these are listed in Table 2.
Because MAC reflects an adequate dose for only 50% of patients, successful clinical anesthesia may require 0.5 to 2.0 MAC for individual patients. More than 90% of all patients become anesthetized following the administration of 1.3 MAC1,3 and, presumably, 1.5 to 2.0 MAC is required to ensure anesthesia in all patients. Furthermore, the doses of anesthetic gases are generally additive; 0.5 MAC of a single agent added to 0.5 MAC of another provides 1 MAC. Based on this principle, and given the influence of other CNS depressants on MAC, anesthesia providers often administer anesthesia using single inhaled anesthetics or mixtures that equal 0.8 to 1.2 MAC, in combination with other central nervous system depressants such as intravenous sedatives and opioids. For example, administering a mixture of 52% nitrous oxide with 2% sevoflurane will provide 1.5 MAC, which could equal as much as 2 MAC if combined with opioids and sedatives.
Finally, it must be emphasized that MAC is a measure of the dose response for an inhalation agent in producing anesthesia. Incremental increases in MAC do not predict with any precision the influence on respiratory or cardiovascular function. For example, 0.5 MAC of an inhalation agent does not necessarily produce half the influence on blood pressure that is produced by 1.0 MAC.
Systemic Influences
At equipotent concentrations (MAC), anesthetic efficacy is identical regardless of the agent or mixture selected. The influence of these agents and mixtures on the lungs, heart, and circulation, as well as less apparent action on other organs, is similar qualitatively but differs in terms of intensity and specific parameters targeted.
Side effects always accompany use of general anesthesia, and accurate knowledge of these properties is required for safe management of the patient. Data comparing the influences of inhalation anesthetics were obtained from healthy volunteers and vary among patients who have preexisting medical conditions, especially of the respiratory, cardiac, hepatic, and renal systems, or who are taking medications that may interact with inhalation anesthetics.
Respiratory Effects
All inhalation agents are respiratory depressants, and their influence on ventilatory response to hypoxemia is greater than that for hypercapnia. Concentrations <0.5 MAC have minimal influence on hypercapnic drive, but the dose response becomes more significant at higher concentrations, leading to apnea at concentrations of 1.5 to 2.0 MAC. In contrast, however, as little as 0.1 MAC produces a 50% to 70% reduction in ventilatory response to hypoxemia.4,5
All inhalation agents share a tendency to increase respiratory rate but decrease tidal volume. Their net influence on minute ventilation is reflected as the degree of hypercapnia that occurs during administration. Nitrous oxide is distinguished from other agents in that it does not reduce net ventilation3,6 (Table 3).
In addition to their effects on central respiratory centers (hypercapnic drive) and carotid bodies (hypoxemic drive), inhalation anesthetics have varied effects on the respiratory tract. Most notable is their ability to relax bronchial smooth muscle; isoflurane and sevoflurane are most effective in this regard.3 They are not so effective as to replace beta2-agonists as emergency bronchodilators, but they are useful agents for providing general anesthesia to patients who have a history of asthma or reactive COPD. Nitrous oxide has no efficacy in this regard.3,6
Cardiovascular Effects
Inhalation anesthetics produce a dose-dependent reduction in mean arterial pressure (MAP). Again, nitrous oxide is the exception3,7,8 (see Table 3). Agents differ in terms of the specific physiologic parameter that they target, for example, heart rate, myocardial contractility, and systemic vascular resistance (SVR). Isoflurane, desflurane, and sevoflurane increase heart rate and decrease systemic vascular resistance but have little influence on cardiac output because their influences on myocardial contractility are minimal.
Skeletal Muscle Effects
Inhalation anesthetics have varying influences on relaxation of skeletal muscle tone—one of the requirements of successful anesthesia for many types of surgery. Isoflurane, desflurane, and sevoflurane provide considerable skeletal muscle relaxation, but nitrous oxide has no effect. Their influence on skeletal muscle can be detrimental. Malignant hyperthermia is a hypermetabolic disorder of skeletal muscle that can be triggered by succinylcholine and most inhalation anesthetics.3 Although susceptibility is largely heritable, variants of classic malignant hyperthermia have been reported in individuals without genetic predisposition. Neither nitrous oxide nor any of the amide local anesthetics has been associated with this disorder, and in fact, they have been listed as nontriggering.
NITROUS OXIDE
General principles of inhalation anesthetics have been reviewed here, and we now turn our attention to specifics regarding nitrous oxide. Nitrous oxide is an inorganic inhalation agent that is colorless, odorless to sweet-smelling, and nonirritating to the tissues. It is nonflammable but will support combustion.
The uptake and distribution of an anesthetic gas to brain tissue is largely dependent on its partition coefficients. For this reason, nitrous oxide has the most rapid onset of the inhalation agents (Table 1). It is transported in blood as free gas; it does not combine with hemoglobin, and it does not undergo biotransformation. Elimination occurs by expiration in a manner that is precisely the reverse of uptake and distribution, and its low solubility allows nitrous oxide to be removed rapidly.
Nitrous oxide has low potency (MAC = 104), but its impressive record of safety allows use of sub-MAC concentrations that are ideal in allaying apprehension and anxiety regarding injections of local anesthetics and treatment in general. In fact, many consider nitrous oxide an inert, benign gas that has little if any influence on vital physiologic functions. This observation is not entirely flawed, especially with doses typically provided by dental sedation units (0.1 to 0.5 MAC). Respiratory and cardiovascular functions are minimally influenced, especially when compared with changes produced by more potent agents. However, caution is advised because this analysis fails to address considerations when nitrous oxide is combined with other anesthetics, sedatives, or opioids. These agents not only lower the MAC for nitrous oxide but work synergistically in depressing respiratory and cardiovascular function.
Although 50% of patients require more than 1 MAC for surgical anesthesia, some patients are anesthetized at lower concentrations. Furthermore, the MAC of a particular anesthetic gas is often lower in small children, the elderly, and the medically compromised. Also, MAC is lowered by concomitant administration of other CNS depressants such as opioids and sedatives. For example, a 20 kg pediatric patient premedicated with a sedative and an opioid may require only 60% to 70% nitrous oxide to achieve MAC.
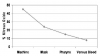
Concentration Delivered
It must be appreciated that the concentration of nitrous oxide that leaves the typical dental unit, and therefore its partial pressure, is not identical to that inspired or that reaching the alveoli. Equipment leakage such as through poorly fitted nasal masks, dead space, mouth breathing, and the ventilatory status of the patient are some of the factors that account for the discrepancy. Even though machine settings may indicate up to 70% nitrous oxide, the actual concentration delivered to alveoli is unlikely to exceed 30% to 50% (Figure 2).9 In other words, it is unlikely that one can deliver greater than 0.3 to 0.5 MAC with the use of typical dental nitrous oxide units. For this reason, one must use caution when extrapolating data derived from medical studies in which nitrous oxide was delivered by full mask or through an endotracheal tube.
Transfer to Gas-Filled Spaces
The blood:gas partition coefficient of nitrous oxide is 0.46, which is more than 30 times greater than that of nitrogen (0.014).When a patient’s inspired gas mixture is switched from air containing approximately 78% nitrogen to an anesthetic mixture containing 70% nitrous oxide, the nitrous oxide will enter gas-filled spaces more than 30 times faster than nitrogen can exit the space. As a result, the volume or pressure within such a space will increase.3 Although lower concentrations (30% to 50%) of nitrous oxide are used for sedation, it enters gas-filled spaces more rapidly than nitrogen can exit. Gas volume and pressure can become dangerously high within an obstructed bowel, pneumothorax, or the middle ear if patency of the eustachian tube is compromised by inflammation. Rupture of the tympanic membrane is possible during administration of nitrous oxide, and negative pressure may develop following discontinuation, leading to serous otitis possibly contributing to postoperative nausea and vomiting.3,10 Pain also may be experienced when nitrous oxide is administered to patients with a sinusitis. Expansion of gas bubbles in the eye following retinal surgery may lead to severe consequences. Other anesthetic gases are administered in such low concentrations that their partial pressures do not lead to the preferential transfer observed with nitrous oxide.
Diffusion Hypoxia
When inhalation of high concentrations of nitrous oxide is discontinued, high partial pressure in blood transfers nitrous oxide to the alveoli rapidly. This dilutes the partial pressure of oxygen in the alveoli and may lead to hypoxemia. For this reason, it is conventional practice to provide the patient with 100% oxygen during the first few minutes following discontinuation of nitrous oxide. This concern is more theoretical than clinical, however. Hypoxemia is significant for only a matter of minutes and has been documented only when high concentrations (>70%) have been delivered by full mask or by endotracheal tube.11 These conditions cannot be met with the use of conventional dental nitrous oxide machines with nasal masks, and any tendency for diffusion hypoxia is trivial.12 Nevertheless, providing 100% oxygen toward the end of a dental appointment has other benefits and is advocated. This allows discontinuation while providing a waning placebo influence, and it allows expired nitrous oxide to enter the scavenging apparatus of the machine, which is sound environmental practice.
Analgesic and Anesthetic Action
The mechanism by which anesthetic gases produce general anesthesia is unknown. The leading theory suggests that they bind to proteins within neuronal membranes and somehow modify ion fluxes and subsequent synaptic transmission.1,3
Unlike other anesthetics, nitrous oxide produces a mild analgesic effect at subanesthetic concentrations. The mechanism for this effect most likely involves an interaction with the endogenous opioid system because it is abolished by administration of the opioid antagonist, naloxone. The strongest evidence is that nitrous oxide stimulates release of enkephalins, which bind to opioid receptors that trigger descending noradrenergic pathways.13 The most common estimate of analgesic efficacy suggests that 30% nitrous oxide delivered by full mask is equivalent to 10 mg to 15 mg morphine.14 This interaction with the endogenous opioid system may account in part for abuse potential attributed to nitrous oxide.
Respiratory Effects
All anesthetic gases increase respiratory rate and diminish tidal volume. Unlike other agents, however, the increase in rate produced by nitrous oxide may actually provide a net increase in minute ventilation (see Table 3).6 Therefore, when used alone for mild to moderate sedation, nitrous oxide does not depress ventilation. However, when it is combined with sedatives or opioids that depress ventilation, a more pronounced and clinically important depression may result.
Similar to other inhalation agents, nitrous oxide produces a dose-dependent depression of ventilatory drive with greater influence on the ventilatory response to hypoxemia than to hypercapnia. As little as 0.1 MAC nitrous oxide can depress hypoxemic drive by 50%.4,5 This is to say that if respiratory depression occurs, nitrous oxide obtunds the body’s normal response to lowered oxygen tension rather than to elevated carbon dioxide tension. Because patients who have significant chronic obstructive pulmonary disease rely almost entirely on hypoxemic drive, some authorities suggest that nitrous oxide should be avoided in these patients. Reasons cited include not only its depression of hypoxemic drive, but also, because high oxygen concentrations are delivered with nitrous oxide, its use may remove the stimulus for hypoxemic drive. However, if the principles of moderate sedation are followed, the patient can always be instructed to breathe more deeply.
Cardiovascular Effects
Nitrous oxide mildly depresses myocardial contractility, but this is offset by its ability to activate sympathetic activity. In both normal patients and those with coronary artery disease, subanesthetic concentrations of nitrous oxide (0.1 to 0.5 MAC) have little influence on cardiac output, stroke volume, and heart rate. At higher concentrations, nitrous oxide actually increases these variables, while volatile agents have the opposite influence.15 Any depressant influences of nitrous oxide are overshadowed by its augmentation of sympathetic tone, but this introduces the need for one word of caution. Opioids depress sympathetic outflow, and when combined with nitrous oxide, depressant influences of nitrous oxide on myocardium could be unmasked.14,16 This may be significant for patients who are compromised by significant degrees of heart failure.
Arterial blood pressure remains stable in patients who receive subanesthetic concentrations of nitrous oxide. Nitrous oxide increases venous tone, leading to increased venous return to the heart,15 and this likely contributes to the stable cardiovascular function observed with nitrous oxide. It is notable that this influence of nitrous oxide on venous tone is exploited at times to facilitate venous access during difficult venipuncture.
Chronic Toxicity
Nitrous oxide has been implicated in the adverse effects on health seen in those individuals who are chronically exposed to trace amounts of the drug. These adversities include infertility, spontaneous abortion, blood dyscrasias, and neurologic deficits. These concerns pertain only to chronic exposure; it is presumed that healthy surgical patients could receive nitrous oxide without harm.
Nitrous oxide irreversibly oxidizes the cobalt atom of vitamin B12 and thereby reduces the activity of B12-dependent enzymes such as methionine and thymidylate synthetases. This appears to be the likely mechanism for toxicity because these enzymes are vital in the synthesis of myelin and nucleic acids. The minimum concentration and duration of exposure at which this influence becomes significant are unsettled, however. Megaloblastic changes in bone marrow are observed following exposure to anesthetic concentrations for 24 hours, and agranulocytosis is apparent after 4 days of exposure.17 Animal studies that used intermittent exposure to trace amounts of various anesthetic gases have failed to reveal any harmful reproductive effects.18 It is generally accepted that proper use of scavenging devices while nitrous oxide is provided to patients in the dental setting eliminates any significant risk. One must be cognizant, however, that proper use of scavenging equipment is only one of several methods used to reduce environmental nitrous oxide concentrations. Other considerations include, but are not limited to, the following: (1) set maximum vacuum settings per manufacturer instructions; (2) check all fittings for leaks (soapy water is an effective and inexpensive diagnostic agent); (3) ensure that there is adequate operatory ventilation and air circulation (air exchange rates above 10/hr recommended); (4) the exhaust system for vacuum suction should vent to outside of the building; (5) always use appropriate gas flow and ensure proper mask fit; (6) minimize patient conversation; and (7) as the procedure nears completion, terminate nitrous oxide flow and administer 100% oxygen for 3 to 5 minutes before removing the nasal hood from the patient.
Contraindications
With its long history of safety in medicine and dentistry, nitrous oxide sedation can be used safely for almost all patients routinely treated in the ambulatory dental setting. In fact, it could be argued that nitrous oxide is the safest of all the modalities available for sedation in dentistry. However, similar to any other pharmacologic agent, nitrous oxide may not be suitable for all patients. It is very important to carefully review the medical history of a patient and to consider the small number of situations in which nitrous oxide sedation may be contraindicated or may at least pose a relative contraindication.
Clearly, inability to use a nasal mask is an absolute contraindication to the use of nitrous oxide. Generally, such patients fall into one of two categories: those who cannot inhale adequately through the nose because of anatomic and/or disease-induced nasopharyngeal obstructions, and those who cannot tolerate and sustain placement of the nasal mask because of psychological and/or cognitive disturbances. Examples include severely phobic, cognitively impaired, or uncooperative pediatric patients, as well as those who present with deviated septum, nasal polyps, upper respiratory infection, allergic rhinitis, and severe sinusitis. In this latter regard, any compromise in patency of the eustachian tube may lead to pressure increases within the middle ear, as was explained previously in this article. In fact, it has been suggested that any recent surgery of the ear presents a contraindication for nitrous oxide.10
Although nitrous oxide has been used successfully in patients with diagnosed personality and psychiatric disorders, it should be used cautiously when those diagnosed with schizophrenia or bipolar disorder are treated. These patients are treated with many psychotropic agents, and the use of nitrous oxide may further alter disposition, leading to results that are highly unpredictable. Medical consultation is strongly encouraged for these patients.
The question of nitrous oxide use in pregnant patients is complicated by opinions based on concerns related to adverse effects associated with chronic exposure. These issues were addressed previously and warrant the use of scavenging devices to protect the healthcare provider. The issue under consideration, however, is the use of nitrous oxide sedation during a single appointment. Clearly, all elective dental treatment should be avoided during pregnancy, especially during the first trimester. However, urgent dental care frequently is required for patients who are pregnant. Under these circumstances, it is not unusual for the patient to be anxious and fearful, often extremely so. For these patients, apprehension should be allayed by using the safest agents available, and nitrous oxide fulfills this requirement.19,20 For ethical reasons, prospective studies cannot address this issue, but retrospective studies of nearly 6,000 general anesthetics in pregnant patients failed to reveal any adverse outcomes for patient or fetus.21-23 Virtually all these anesthetics included nitrous oxide. For the pregnant patient who is apprehensive and requires urgent dental care, nitrous oxide should be regarded as the sedation agent of choice. Any evidence of complication during pregnancy certainly warrants consultation with the patient’s obstetrician.
About the Authors
Dr. Becker is a Professor of Allied Health Sciences at Sinclair Community College and Associate Director of Education, General Dental Practice Residency, at Miami Valley Hospital in Dayton, Ohio.
Dr. Rosenberg is a Professor of Oral and Maxillofacial Surgery and Head of the Division of Anesthesia and Pain Control at Tufts University School of Dental Medicine, and an Associate Professor of Anesthesia at Tufts University School of Medicine, Boston, Massachusetts.
REFERENCES
1. Evers AS, Crowde CM, Balser JR. General anesthetics. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 11th ed. New York, NY: McGraw-Hill; 2006.
2. Chung DC, Lam AM. Essentials of Anesthesiology. 3rd ed. Philadelphia, PA: WB Saunders; 1997.
3. Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: Lange Medical Books/McGraw Hill; 2006.
4. Dahan A, van den Elsen MJ, Berkenbosch A, et al. Effects of subanesthetic halothane on the ventilatory responses to hypercapnia and acute hypoxia in healthy volunteers. Anesthesiology. 1994;80:727-738.
5. Yacoub O, Doell D, Kryger MH, Anthonisen NR. Depression of hypoxic ventilatory response by nitrous oxide. Anesthesiology. 1976;45:385-389.
6. Eger EI. Respiratory effects of nitrous oxide. In: Eger EI, ed. Nitrous Oxide. New York, NY: Elsevier; 1985.
7. Weiskopf RB, Cahalan MK, Eger EI II, et al. Cardiovascular actions of desflurane in normocarbic volunteers. Anesth Analg. 1991;73:143-156.
8. Eisele JH. Cardiovascular effects of nitrous oxide. In: Eger EI, ed. Nitrous Oxide. New York, NY: Elsevier; 1985.
9. Sher AM, Braude BM, Cleaton-Jones PE, et al. Nitrous oxide sedation in dentistry: a comparison between Rotameter settings, pharyngeal concentrations and blood levels of nitrous oxide. Anaesthesia. 1984;39:236-239.
10. Munson ES. Complications of nitrous oxide anesthesia for ear surgery. Anesth Clin North Am. 1993;11:559-572.
11. Eger EI. Pharmacokinetics. In: Eger EI, ed. Nitrous Oxide. New York: Elsevier; 1985.
12. Quarnstrom FC, Milgrom P, Bishop MJ, DeRouen TA. Clinical study of diffusion hypoxia after nitrous oxide analgesia. Anesth Prog. 1991;38:21-23.
13. Zhang C, Davies MF, Guo TZ, Maze M. The analgesic action of nitrous oxide is dependent on the release of norepinephrine in the dorsal horn of the spinal cord. Anesthesiology. 1999;91:1401-1407.
14. Jastak JT, Donaldson D. Nitrous oxide. Anesth Prog. 1991;38:142-153.
15. Eisele JH. Cardiovascular effects of nitrous oxide. In: Eger EI, ed. Nitrous Oxide. New York: Elsevier; 1985.
16. Stanley TH, Liu WS. Cardiovascular effects of meperidine-N2O anesthesia before and after pancuronium. Anesth Analg. 1977;56:669-673.
17. Nunn JF. Clinical aspects of the interaction between nitrous oxide and vitamin B12. Br J Anaesth. 1987;59:3-13.
18. Mazze RI, Fujinaga M, Rice SA, et al. Reproductive and teratogenic effects of nitrous oxide, halothane, isoflurane, and enflurane in Sprague-Dawley rats. Anesthesiology. 1986;64:339-344.
19. Santos AC, Braveman FR, Finster M. Obstetric anesthesia. In: Barash PG, Cullen BF, Stoelting RK, eds. Clinical Anesthesia. 5th ed. Philadelphia, PA: Lippincott-Raven; 2006.
20. Rosen MA. Management of anesthesia for the pregnant surgical patient. Anesthesiology. 1999;91:1159-1163.
21. Mazze RI, Kallen B. Reproductive outcome after anesthesia and operation during pregnancy: a registry study of 5405 cases. Am J Obstet Gynecol. 1989;161:1178-1185.
22. Aldridge LM, Tunstall ME. Nitrous oxide and the fetus: a review and the results of a retrospective study of 175 cases of anaesthesia for insertion of Shirodkar suture. Br J Anaesth. 1986;58:1348-1356.
23. Crawford JS, Lewis M. Nitrous oxide in early human pregnancy. Anaesthesia. 1986;41:900-905.