You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Like the peripheral system, the performance of neurons within the central nervous system is predicated on the activity of neurotransmitters. In addition to acetylcholine and norepinephrine, however, many additional transmitters have been identified. Their precise functions are not fully understood, but some usefulness can be derived from the simple fact that neuron-to-neuron synapses are either excitatory or inhibitory. Normal function of the central nervous system (CNS) requires a delicate balance between these influences. It must be understood that a particular neurotransmitter can inhibit neurons in one brain area while exciting those in another. This is because neurotransmitters bind and activate a specific class of receptor, but receptors exist as many subtypes. For example, there are at least 14 subtypes of serotonin (5-HT) receptors distributed throughout the various brain regions. Despite being activated by the same neurotransmitter, one subtype may produce excitation while another produces inhibition. A simplified synopsis of the principal neurotransmitters and their most common responses mediated is presented in Table 1.
The “limbic system” is a functional label for all tracts and nuclei that contribute to emotional behavior and motivational drive. The hypothalamus is credited as the source of most vegetative functions (eg, hunger, thirst, anger) and is considered a central component of this system. Other components include portions of the cortex, thalamus, and basal ganglia that function to integrate emotional state with motor and visceral activities.
Psychiatric illnesses are believed to result in part from biochemical derangements within the limbic structures. Much of this reasoning is based on known pharmacological actions of several psychotropic drug classes. For example, the efficacy of antipsychotic medications is attributed to inhibiting the actions of dopamine, and the psychoses are therefore believed to be attributable in some manner to excess dopamine transmission. This reasoning is hardly scientific and merely reflects our current futility in comprehending psychiatric illnesses.
Typically, psychotropic drugs are agents used to treat psychiatric disorders. They include sedative-anxiolytics, antipsychotics, antidepressants, and the antimanic agents. While these drugs all act in some manner to alter the activity of neurotransmitters, psychiatric illness cannot be explained entirely on biochemical defects. Indeed, one cannot overlook the importance of psychological and social factors in both the pathophysiology of mental illness, and its response to specific pharmacotherapeutic agents.2
Sedative-Anxiolytics
Drugs in this particular class have the ability to calm (anxiolytic), induce drowsiness (sedative), or promote sleep (hypnotic). These effects generally follow a classic dose-response pattern. For example, a drug marketed as an anxiolytic is formulated as a lower dosage than if it were to be promoted as a sedative or hypnotic for insomnia. Several of these agents are prescribed as skeletal muscle relaxants, but this effect is likely an extension of their anxiolytic properties. Distinct central mechanisms for anxiolysis, sedation, and skeletal muscle relaxation have been postulated but have not been confirmed.
In addition to their useful effects, sedative-anxiolytics also have in common several side effects. As might be expected, high doses of any CNS depressant can depress respiration and cardiovascular tone. Chronic use leads to tolerance and dependence and, following abrupt discontinuation, a withdrawal syndrome occurs. Furthermore, some patients experience paradoxical responses, ie, excitation rather than sedation. The precise mechanism for this peculiar response cannot be explained but is known to occur with greater frequency among pediatric and geriatric patients.
The benzodiazepines are by far the most widely prescribed agents of this class. Virtually all of their effects can be explained by an ability to activate specific benzodiazepine receptors leading to a potentiation of gamma-aminobutyric acid (GABA)–mediated influx of chloride ions. They are unique compared with other sedatives in their ability to produce anterograde amnesia. This is an advantage for the dentist prescribing them for treatment anxiety but introduces concern when prescribed chronically for anxiety disorders or insomnia. This issue, added to those regarding abuse and dependence, has diminished their medical use for chronic disorders in favor of antidepressant medications that lack these influences.
In recent years, novel agents have been introduced for insomnia that are not benzodiazepine-derived, but nevertheless act as agonists at benzodiazepine receptors. Marketing strategies advertise them as nonbenzodiazepines in an effort to separate them from negative impressions regarding traditional benzodiazepines. However, their potential for anterograde amnesia and dependence is no different than that for the more traditional benzodiazepines. These newer agents include zolpidem (Ambien) and Zaleplon (Sonata), having relatively fast onset and short durations, and eszopiclone (Lunesta) having a slower onset and longer duration.
Dental Implications for Patients Medicated With Sedative-Anxiolytics
Drug tolerance and dependence are the principal concerns for the dentist when managing patients taking sedatives chronically. Common sense dictates caution when administering sedation or general anesthesia due to the potential for enhanced CNS depression. However, tolerance develops following chronic use of these agents, and patients may actually require greater doses to provide adequate sedation for dental treatment. Further complicating matters is the fact that degrees of tolerance or dependence can be estimated based on the patient’s frequency and duration of use only. Although intravenous sedation allows for accuracy of titrated doses, any decision regarding an oral dosage is empiric at best. Furthermore, if the patient has developed benzodiazepine dependence, oversedation cannot be countered using the reversal agent, flumazenil, for fear of inducing withdrawal.
The only drug interaction with benzodiazepines of concern to the dentist is the use of macrolide antibiotics, eg, erythromycin. These antibiotics compete for CYP3A4 enzymes, which catalyze oxidative reactions that inactivate most benzodiazepines and thereby elevate serum levels and prolong their half-lives. Lorazepam (Ativan) is a notable exception because it is metabolized via conjugation rather than oxidation.
Antidepressants
Major depression is one of the most common psychiatric illnesses, afflicting more than 12% of men and 20% of women at some point in life.3 The suicide rate in such patients is roughly 30 times that of the general population and emphasizes the importance of effective treatment. Psychotherapy alone is effective in some forms of mild depression and is a useful adjunct in others, but drug therapy is clearly the treatment of choice for severely depressed patients.2
Precise neurochemical mechanisms for depression have not been defined. Historically, depressed patients were thought to suffer deficiencies in central biogenic amines, eg, norepinephrine and serotonin. This belief spawned continued development of drugs that elevate the concentrations of these neurotransmitters within the central nervous system. Although these drugs are the foundation of treatment for depression, elevation of norepinephrine and serotonin levels per se cannot entirely explain their effectiveness. Neurotransmitter concentrations are elevated within hours of administering an antidepressant, but clinical improvement is not appreciated for several weeks and may require several months for maximum benefit. Current speculation is that benefit arises from sustained elevations in these neurotransmitters that lead to alterations in the number or sensitivity of specific receptor subtypes.2,3 Additional biochemical derangements that have been implicated in depression include dopamine deficiencies and elevations in stress hormone levels such as cortisol and corticotropin.3 The sum of all these considerations suggests that depression is a consequence of many derangements acting alone and in concert.
It is not uncommon for antidepressant medications to be described using the lay term “mood-elevator.” Unfortunately, use of such a term nurtures a misconception that antidepressants are CNS stimulants when, in fact, their most troubling side effects often include sedation and lethargy. Conventional CNS stimulants such as amphetamine and cocaine increase concentrations of these neurotransmitters and transiently elevate mood but produce agitation and lack benefit in improving chronic negative ideations. Unlike CNS stimulants, and conventional sedatives, antidepressants have no potential for recreational abuse.
Monoamine Oxidase Inhibitors
The monoamine oxidase inhibitors (MAOI) were the first class of drugs used to treat depression. As their name implies, they elevate norepinephrine and serotonin levels by limiting their oxidation by the enzyme monoamine oxidase (MAO). The major drawback of this drug class is its potential for serious food and drug interactions, many of which precipitate an acute hypertensive crisis. Compliance with medication instructions is critical, and the depressed patient may not be so inclined. Phenelzine (Nardil) is the only member of this class in current use.
Tricyclic Antidepressants
Tricyclic antidepressants (TCA) are so named because of their three-ringed molecular structure. They differ in their propensities to inhibit neuronal uptake of either norepinephrine or serotonin. Formerly, this was believed to provide a basis for prescribing specific agents for selected patients, and perhaps offered a biochemical basis for classifying various forms of depression. This belief is no longer tenable and, in fact, all agents and classes of antidepressants exhibit comparable efficacy. Any basis for selecting a particular agent is largely empiric and is correlated more with the patient’s medical status or the side effect profile of the particular agent.4
The tricyclic compounds also differ in their activity as antagonists at cholinergic, histamine, and alpha receptors. All of these actions contribute to their sedative side effect but individually explain their bothersome peripheral autonomic side effects. Anticholinergic side effects most often present as xerostomia, urinary retention, and constipation, while alpha receptor blockade accounts for orthostatic hypotension. Anticholinergic activity on cardiac tissues introduces a risk for cardiac arrhythmias that is particularly troubling following drug overdoses. Although a precise mechanism has not been established, tricyclic agents may also produce seizure activity, especially if patients have a preexisting disorder.
Amitriptyline (Elavil) is generally regarded as the prototype of this group of antidepressants, but today it is more commonly used in the management of insomnia and chronic pain. Neurotransmission of pain (nociception) is inhibited by descending neural pathways that release norepinephrine as a neurotransmitter. Tricyclic antidepressants elevate norepinephrine concentrations within these synapses and are effective adjuncts for pain management at dosages well below those required for the treatment of depression. Their sedative influences make them particularly useful at night.
Selective Serotonin Reuptake Inhibitors
The selective serotonin reuptake inhibitors (SSRI) inhibit the neuronal uptake of serotonin and lack most of the annoying autonomic side effects associated with tricyclic antidepressants. Fluoxetine (Prozac) was the first of this class to be introduced. The most common adverse effects of SSRIs include nausea, diarrhea, headache, jitteriness, insomnia, fatigue, and sexual dysfunction. Sexual dysfunction (including decreased libido, impaired arousal, and anorgasmia) is a common adverse effect and affects a significant number of patients treated. Abrupt discontinuation of an SSRI results in dizziness, anxiety, and dysphoria. This withdrawal can be minimized by gradual tapering and is least likely to occur with fluoxetine, which has the longest half-life.4
It is difficult to assess negative publicity regarding a possible association between SSRI antidepressants and suicidal or homicidal ideation. Current scientific evidence does not support these concerns and most likely reflects the extensive use of SSRIs in psychiatric patients already predisposed to suicidal tendency. There is particular controversy regarding the influence of antidepressants on suicidal tendency among children and adolescents, but scientific data are sparse. Depression is a major risk factor for suicide, which ranks third as the most common cause of death among teens. During the past decade, the increased use of antidepressants in teens has actually paralleled a significant decline in suicide rate.5 This represents an “association,” but does not prove cause-effect. Nevertheless, it appears the overall benefit of antidepressant therapy in this age group may outweigh any potential for negative outcome. Clinical studies are underway to better define these issues. Meanwhile, antidepressant therapy in this age group must be closely monitored. SSRI antidepressants are known to produce agitation and manic behavior as side effects, and these could contribute to suicidal tendency.
Atypical Antidepressants
Newer “atypical” antidepressants are structurally unrelated to the other classes, and their varied pharmacological actions preclude a more precise classification. For example, venlafaxine (Effexor) and duloxetine (Cymbalta) inhibit reuptake of both norepinephrine and serotonin. Many texts refer to these as serotonin-norepinephrine reuptake inhibitors. Although this action resembles the tricyclic antidepressants, they have a different molecular structure and do not produce the autonomic side effects typical of the TCAs. Aggressive marketing by the manufacturer has persuaded some to believe these serotonin-norepinephrine reuptake inhibitors have the greatest efficacy, but analysis of clinical studies is not convincing.
Clinical Considerations
Antidepressants that elevate serotonin levels are a concern if taken along with other medications that enhance serotonin levels. This can lead to a so-called serotonin syndrome characterized by hyperpyrexia, confusion, agitation, and neuromuscular irritability. This has been observed with St John’s wart, an over-the-counter herbal antidepressant, and the various “triptan” drugs used for migraine headaches, eg, sumatriptan (Imitrex).
The SSRI antidepressants and many of the atypical agents are gaining widespread use for conditions other than depression. They have virtually replaced the benzodiazepines for chronic management of most anxiety disorders. Other uses include chronic pain, eating disorders, and as adjuncts in managing alcohol abuse. The biochemical defect in premenstrual dysphoric syndrome (PMS) is related to interplay of elevated sex hormone and diminished serotonin. Although fluoxetine is the only SSRI that has FDA approval for this indication, all of these antidepressants are effective. Dosages must be individualized, but are generally administered for 7 to 10 days preceding each menses.
It should be emphasized that no category of antidepressant or specific agent has proven more effective than others for managing depressive illness.6 However, an unsatisfactory response to one agent does not preclude therapeutic success with another. This is frequently the case following failure with the agent initially selected. Selected antidepressants are summarized in Table 2.
Dental Implications for Patients Medicated With Antidepressants
When prescribing or administering sedatives, use caution for patients taking antidepressants that have significant sedative properties. Otherwise, the principal dental considerations for patients taking antidepressant medications are their potential drug interactions. The most important of these are summarized in Table 3, but a few of these will receive more detailed explanation.
The most storied interaction of relevance to dentists was the putative interaction between epinephrine and the monoamine oxidase inhibitors. It was believed that inhibition of MAO could potentiate the activity of epinephrine by delaying its oxidation. While this is a valid consideration for many sympathomimetic drugs, it is not the case for epinephrine or levonordefrin (NeoCobefrin), which are catecholamines in structure and rely most heavily on methylation by catechol-O-methyl-transferase for their termination, not monoamine oxidase.
Epinephrine and levonordefrin are not without some concern, however. Cardiac tissues may be excited by antidepressants that elevate norepinephrine levels, and this could become accentuated with concurrent administration of any sympathomimetic drug. This concern is for most classes of antidepressants, other than the selective serotonin reuptake inhibitors. Tricyclic antidepressants present greatest concern because they also produce anticholinergic actions on the heart. Epinephrine and levonordefrin are not contraindicated in these patients, but they should be used cautiously. For example, heart rate and blood pressure should be reassessed following each 20-mg to 40-mg dose of epinephrine administered (1 to 2 cartridges containing a 1:100,000 concentration).
The SSRI antidepressants inhibit several families of hepatic enzymes (CYP-450), which may delay the biotransformation and clearance of numerous other drugs. Of particular importance for dentistry is the CYP2D6 family of enzymes, which is responsible for demethylating codeine, hydrocodone, and oxycodone to their active metabolites; morphine, hydromorphone, and oxymorphone, respectively. The SSRI antidepressants vary in their intensity for inhibiting these enzymes, with fluoxetine (Prozac) and paroxetine (Paxil) having the greatest influence. Patients medicated with these antidepressants may not experience adequate pain relief from codeine or its derivatives.7,8
Antipsychotic Drugs
The psychoses include schizophrenia and other delusional impairments in which patients have difficulty in comprehending reality. These disorders are managed using antipsychotic drugs. Although less descriptive, these agents may also be referred to as “neuroleptics,” a term less offensive to the patient. Despite our poor understanding of their precise mechanisms and their myriad side effects, it cannot be disputed that antipsychotic drugs are effective. Extensive clinical studies have found that the relapse rate is much greater for patients who discontinue antipsychotic medication, compared with those who continue therapy.
It is significant that antipsychotic drugs are not disease-specific; they can be used for conditions other than schizophrenia and other psychoses. These include acute agitation and delirium associated with Alzheimer dementia, fever, septicemia, amphetamine intoxication, or mechanical ventilation. They are frequently used in combination with lithium and anticonvulsants during acute phases of mania, and with antidepressants for complex cases of depression. Most agents are excellent antiemetics and can be used to manage nausea and vomiting. Finally, their sedative effects can be used to potentiate sedatives and opioids during anesthesia and pain management.
Most of the first-generation antipsychotic drugs are derivatives of the phenothiazine molecular structure, although haloperidol (Haldol) is a notable exception derived from a butyrophenone. For this reason, it is not uncommon for antipsychotics to be referred to as phenothiazine compounds. Chlorpromazine (Thorazine) was the first drug used specifically in the management of psychoses and retains its status as the prototype of the antipsychotics. The actual antipsychotic efficacy of the three dozen compounds available is attributed to their ability to act as antagonists at dopamine receptors within the limbic regions. Dopamine and its receptors perform many functions throughout the brain, and at least five dopamine receptors have been identified, labeled as D1 thru D5. Antagonism of D2 receptors within the limbic regions is credited as the antipsychotic mechanism for these drugs, but most agents lack specificity for this particular dopamine receptor and produce troubling side effects by virtue of their antagonizing D2 and other dopamine receptor subtypes in additional brain regions.
Useful and several adverse effects of antipsychotic agents are attributed to the blockade of dopamine receptors within specific brain regions. In addition to limbic sites, where their antipsychotic influence is produced, these agents produce useful antiemetic effects by blocking dopamine transmission in the chemoreceptor trigger zone. Within the hypothalamus, dopamine normally acts to inhibit prolactin release. By blocking this influence, antipsychotic agents may produce galactorrhea.
The most troubling side effect of antipsychotic drugs is attributed to the blockade of dopaminergic transmission within the basal ganglia. This results in so-called extrapyramidal syndromes that include akathisia, Parkinsonian symptoms, and tardive dyskinesia. In some cases, the physician may prescribe the concurrent use of centrally acting anticholinergics such as benztropine (Cogentin) to obtund these effects. This is designed to offset excitatory pathways that release acetylcholine as their neurotransmitter, a strategy also used in the management of Parkinson disease. These extrapyramidal influences are the most feared side effects of antipsychotic drugs and deserve further analysis.
Akathisia is a subjective feeling of restlessness leading to a compelling need to move. Patients feel that they must get up and walk or continuously move about, and this behavior may be mistaken for agitation. Their distinction is critical, because agitation is treated with an increase in dosage of the antipsychotic drug and will worsen akathisia. It is not uncommon for this syndrome to be undiagnosed and may interfere with the patient’s medication compliance. It should be noted that this extrapyramidal effect is produced by promethazine (Phenergan) and prochlorperazine (Compazine), which are antipsychotic derivatives used commonly for nausea and vomiting. Parkinson disease is a well-defined neurologic disorder associated with dopamine deficiency within the basal ganglia. It should not be surprising that dopamine blockade by antipsychotic drugs can produce a syndrome of side effects indistinguishable from this disease and is described as Parkinsonism. Clinically, there is a generalized slowing of movement (bradykinesia) with masked facial expression and a reduction in arm movements. The syndrome characteristically evolves gradually over days to weeks of drug use. The most noticeable signs are rigidity and tremor at rest, especially involving the upper extremity, and perioral tremors along with ‘‘pill-rolling’’ movements may be seen. Some of these parkinsonian side effects may be mistaken for depression, because the flat facial expression and retarded movements may resemble signs of depression.
Tardive dyskinesia is associated with chronic use of antipsychotic drugs and occurs in as many as 15% to 25% of psychotic patients. It is characterized by stereotyped, repetitive, tic-like movements of the face, eyelids (blinks or spasm), mouth (grimaces), tongue, extremities, or trunk. Like other extrapyramidal syndromes, these movements disappear during sleep and are dependent on the patient’s level of arousal or emotional distress. The most perplexing aspect of this syndrome is that it may persist indefinitely after discontinuation of the precipitating medication, but fortunately, in most cases, symptoms disappear or at least gradually decline over a period of months. Most antiparkinsonism drugs provide little relief, and Cogentin actually worsens the condition. There is simply no adequate treatment available.
The gamut of side effects produced by antipsychotics can be explained by their ability to act as antagonists at various receptors. In addition to the dopamine receptors described above, antipsychotic agents also block histaminic, cholinergic, and alpha receptors. Within the central nervous system, these actions contribute to the sedative effects of these agents because histamine, acetylcholine, and norepinephrine act here as excitatory neurotransmitters. Peripherally, they provide a series of bothersome autonomic effects including xerostomia, constipation, urinary retention, and orthostatic hypotension. With the exception of those attributed to dopamine blockade, side effects of the antipsychotics resemble those of the tricyclic antidepressants.
Although acutely psychotic patients may improve within a day or two of therapy, chronic conditions generally require 2 to 3 weeks of treatment to notice any benefit. Maximum improvement may require several months of therapy.9 With the exception of clozapine (discussed below), no single agent can be regarded as having superior efficacy overall or for any specific symptom. Individual patients may appear to do better with one agent than another, but this can be determined only by trial and error. In cases of noncompliance or with failure of oral treatment, the patient can be treated with injections of long-acting, depot preparations (generally every 2 weeks). These are particularly useful for delusional paranoid patients who frequently believe that “medicines are poison.” Exemplary antipsychotic agents are summarized in Table 4. Dosages for antipsychotic agents can be quite variable and must be titrated to the individual patient. Notice from the table that the more potent conventional agents, ie, those requiring <50 mg/day, produce the greatest incidence of extrapyramidal effects, while those having less potency are more likely to produce sedation and autonomic side effects. Potency per se is hardly the explanation for these differences; less potent agents appear to provide their own anticholinergic influences that counter extrapyramidal effects. Nevertheless, it is a useful clinical caveat for predicting the side-effect profile of a particular antipsychotic agent.
In recent years, researchers have formulated several novel antipsychotic agents that preferentially block dopaminergic receptor subtypes found within the limbic regions, specifically D2 receptors, or act as partial agonists. This reduces the likelihood of their producing extrapyramidal or other side effects mediated at dopaminergic receptors in other brain regions. Many of these so-called second-generation, or “atypical,” agents also block specific serotonin receptor subtypes, but the significance of this action is unknown. Clozapine was the first of these agents to receive FDA approval and is generally agreed to be the most effective drug to date. Its advantage is offset by its tendency to produce agranulocytosis in 1% to 2% of patients treated, which requires that patients have white blood cell (WBC) counts weekly for a month or two and then biweekly throughout therapy. Risperidone (Risperdal) and olanzapine (Zyprexa) do not produce agranulocytosis and are associated with a lower incidence of sedation and autonomic side effects. Both of these drugs are very expensive (5 to 10 times the cost for first-generation agents), and their routine use is frequently criticized. The use of these agents is generally reserved for severe cases, or those refractory to the more traditional agents.9,10
Dental Implications for Patients Medicated With Antipsychotic Drugs
There are no well-established drug interactions associated with antipsychotic medications and drugs conventionally used in dental practice. However, some consideration may be given to the use of vasopressors in local anesthetic solutions and the use of antihistamines and antiemetics used in sedation regimens. Most antipsychotic agents have modest alpha-blocking actions that may counter any increase in systemic vascular resistance following systemic absorption of vasopressors contained in local anesthetic formulations. Yagiela et al11 demonstrated that chlorpromazine ameliorated the pressor responses to levonordefrin and norepinephrine. Because epinephrine normally lowers systemic vascular resistance due to its beta-2 mediated vasodilation, any influence of this vasopressor in reducing arterial constriction was observed only with high-dose epinephrine, such as that employed during the management of cardiac arrest.
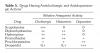
It may also be wise to avoid the use of drugs having significant anticholinergic or antidopaminergic action that could enhance the potential for side effects attributable to these mechanisms. Added anticholinergic influences may precipitate delirium,12 and dopamine blockade may increase the risk for extrapyramidal symptoms. Antihistamines and antiemetics have these properties and are frequently used in sedation and anesthesia regimens. These are summarized in Table 5.
Antimanic Agents
Mania is an affective disorder essentially opposite that of depression. Manic patients demonstrate a variety of hyperactive behaviors, including agitation, excessive talkativeness, elation, fleeting attention, increased psychomotor activity and perhaps, delusion, and frank psychosis. Often patients fluctuate between periods of depression and mania, in which case their affective disorder is described as bipolar rather than unipolar. The dated term for this disorder is “manic depression.” Potent sedatives and antipsychotic drugs may be used as adjuncts for the management of mania, especially acute episodes, but lithium is still regarded as the standard for chronic treatment.10 Unlike other drugs, having complex molecular structures, lithium is merely a monovalent cation, [Li+]. Its mechanism of action is unknown, but it is thought to somehow stabilize neuronal membranes, thereby reducing their rate of discharge and neurotransmitter turnover. Lithium is effective for the prevention and for treatment of manic episodes, and also for prevention of depressive mood swings in the patient with bipolar disorder.8
The typical daily dose for lithium is 300 mg three or four times a day and results in a therapeutic serum level of 0.4 mEq/L to 1.2 mEq/L. Provided that serum concentrations are sustained at this level, lithium is relatively free of side effects. Higher concentrations result in toxicity that is directly related to the serum concentration and may require hemodialysis in life-threatening cases. These are summarized in Table 6. To avoid toxicity, patients must be compliant with their dosage schedule and have their serum concentrations monitored periodically.
Anticonvulsants
Although lithium is regarded as the conventional agent for managing manic disorders, several anticonvulsant agents have been shown to be equally effective and safer for patients who are questionably compliant.
Seizures are clinical manifestations of synchronous discharges from cortical neurons and may be caused by drug toxicity, or a variety of injuries and diseases. If a cause cannot be ascertained, the seizure is regarded as primary or idiopathic. Seizures reflect the general function of the brain region involved and include altered consciousness (absence seizures), involuntary movements (convulsive seizures), and behavioral automatisms. Seizures are designated as “epileptic” only if they have a chronic pattern of recurrence. Indeed, it is common for patients to experience a single seizure, never experiencing another; in many cases it is found to be secondary to a syncopal episode.
Despite the fact that many seizures are neither convulsive nor epileptic, antiseizure medications are called anticonvulsants or antiepileptics by convention.
They depress excitability of neurons by hindering influx of sodium or calcium ions, or potentiating the actions of inhibitory neurotransmitters such as GABA. Regardless of their precise mechanisms, they suppress the spontaneous firing of actual seizure foci and/or the spread of impulses from these foci to neighboring neuron pathways.7,13 The stabilizing influence of these drugs on neuronal membranes has proven useful in managing several conditions in addition to seizure disorders. These include bipolar affective disorders (manic depression), anxiety disorders, and pain syndromes having neuropathic components such as trigeminal neuralgia.
The various anticonvulsants differ in their efficacy for managing different categories of seizures. The agents commonly used also for nonseizure disorders such as pain and bipolar disorders are listed in Table 7.
Dental Implications for Patients Medicated With Lithium and Anticonvulsants
All anticonvulsants have sedative properties, but patients develop tolerance to this influence within a few weeks of use. Nevertheless, this property should be considered when administering sedatives. Patients chronically medicated with clonazepam or clorazepate invariably develop tolerance and dependence to benzodiazepines. This is problematic when choosing dosages for oral sedation, but careful intravenous titration of benzodiazepines is generally without problem. The use of flumazenil for reversal should be avoided. Drug interactions to be considered are summarized in Table 8.
About the Author
Dr. Becker is an Associate Director of Education, General Dental Practice Residency, at Miami Valley Hospital in Dayton, Ohio.
References
1. Bloom FE. Neurotransmission and the central nervous system. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 11th ed. New York, NY: McGraw-Hill; 2006:328-336.
2. Baldessarini RJ. Drug therapy of depression and anxiety disorders. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 11th ed. New York, NY: McGraw-Hill; 2006:430.
3. Belmaker RH, Agam GA. Major depressive disorder. N Engl J Med. 2008;358(1):55-68.
4. Drugs for depression and anxiety. The Medical Letter on Drugs and Therapeutics. 2001;14:73-83.
5. Vitiello B, Swedo S. Antidepressant medications in children. N Engl J Med. 2004;350(15):1489-1491.
6. Which SSRI? The Medical Letter on Drugs and Therapeutics. 2003;45(1170):93-95.
7. Olin BR, Hebel SK, Dombek CE, eds. Drug Facts and Comparisons 2007. St Louis, MO: Facts and Comparisons Inc; 2007.
8. Drug interactions. The Medical Letter on Drugs and Therapeutics. 1999;41(1056):61-62.
9. Choice of an antipsychotic drug. The Medical Letter on Drugs and Therapeutics. 2003;45(1127):102-104.
10. Drugs for psychiatric disorders. Treatment Guidelines From the Medical Letter. 2006;4:35-45.
11. Yagiela JA, Duffin SR, Hunt LM. Drug interactions and vasoconstrictors used in local anesthetic solutions. Oral Surg Oral Med Oral Pathol. 1985;59:565-571.
12. Inouye SK. Delirium in older patients. N Engl J Med. 2006;354:1157-1165.
13. Drugs for epilepsy. Treatment Guidelines From the Medical Letter. 2003;1(9):57-64.