You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
Both the illicit production and the use of methamphetamine, a powerful stimulant that affects the central nervous system, have a tremendous impact on people’s lives and on national and state resources.1 Between 1996 and 2012, the percentage of adults admitted to treatment facilities for methamphetamine use increased from 2.6% to 8.5% for the nation and from 9.7% to 21.9% for Iowa.2 In addition to burdening the healthcare system, methamphetamine production and use have negatively impacted the criminal justice system. In 2012, 50.9% of people imprisoned on drug charges in Iowa had committed a crime related to the drug methamphetamine.3
Methamphetamine use has been purported to cause destructive dental caries. Some authors have suggested that it may be the chemical or physical qualities of methamphetamine or its components, such as their acidity or toxicity, directly attacking tooth structure.4,5 Other studies suggest that methamphetamine causes dry mouth, which reduces the protective aspects of saliva.6-8 Others do not attribute it to methamphetamine but to users’ poor oral hygiene, high consumption of refined carbohydrates, and lack of routine dental care.4,8,9 The relationship between methamphetamine use and poor oral health was first suggested for prescription use of methamphetamine and then illicit use.10,11 The relationship with illicit use has been reported in a number of articles,4,5,8,9,11-25 and has been investigated in research studies that measured oral health by self-report26-29 and by clinical examinations or screenings.7,30-33 Of the studies using clinical data, mixed results were found from bivariate analyses. Two studies concluded that methamphetamine use had a negative impact on oral health,7,32 and two studies reported that there was no impact.30,31 Multivariate analysis also resulted in mixed results. Controlling for demographic variables, professional care, oral hygiene, sugar consumption, and tobacco use, Cretzmeyer et al found that oral health (number of teeth present and total filled and carious surfaces) was not statistically different for methamphetamine abusers and those who abused other drugs.31 Conversely, Shetty et al, controlling for demographic and professional care variables, found that methamphetamine abusers had more missing teeth and poorer self-reported oral health than adult NHANES III respondents; however, they did not find a difference for dental caries.33 Based on a systematic review of methamphetamine use and health for adolescents, Marshall and Werb concluded that there is a research gap in that there is insufficient evidence of an association between methamphetamine use and dental outcomes and that future research should assess potential covariates and adjust for them using stratified or multivariate analyses.34
This study examined the relationship between methamphetamine use and oral health using data collected in 1998 from a population of recently admitted prisoners. This study is important because previous research has not resolved this question. Studies using clinical measures of oral health status are few in number and none of these studies adequately controlled for covariates. Additionally, the findings from these studies have been inconsistent. A better understanding of the relationship of methamphetamine use on oral health status should assist dental professionals in providing treatment to methamphetamine users, especially preventive services like those provided by dental hygienists, and could have implications for policy decisions related to dental care for methamphetamine users in prisons, drug treatment centers, and dental health clinics.
Methods and Materials
This cross-sectional study was conducted within the confines of the staff dental hygienist’s workday. Oral health evaluations and personal interviews were used to collect data from a sample of inmates newly admitted to the Iowa Medical Classification Center (IMCC) between June and December 1998.
All inmates entering Iowa’s prison system are evaluated at the IMCC for mental and physical health conditions. Oral health evaluations are conducted on the day after admission and new inmates are examined by the staff dentist or dental hygienist. Mouth mirrors, explorers, and panographic radiographs are standard equipment used at the IMCC to evaluate each tooth surface for each inmate and the oral health information is recorded on the IMCC anatomical odontogram, a chart depicting the crown and root for each of the 32 teeth possibly present in an adult mouth. Because the evaluations are conducted to determine treatment needs, adequate fillings are not differentiated from sound surfaces. When the data were collected, the dental hygienist had 16 years of clinical experience, 3 years at IMCC, 7 years at a maximum-security prison, and 6 years in private practice. The purpose of the study was discussed with the dental and medical directors and warden during the planning phase, and a design that restricted data collection to the dental hygienist’s patients was accepted. The medical director and warden approved the study protocol and consent form. The University of Iowa institutional review board (IRB) determined that, because this study was limited to analysis of de-identified data, it did not meet the regulatory definition of research involving human subjects and, therefore, was not subject to further IRB review.
As stated above, study participants were drawn from the inmates evaluated by the staff dental hygienist. On days when there were too many inmates for the dental hygienist to both provide an oral health evaluation and collect study data, a set format of offering study participation to every second, third, or fourth inmate, depending on the number of inmates to be examined, was used. Within this time constraint, inmates were invited to be a part of the study and there were no exclusions based on gender, race, age, or any other covariate. Inmates who elected to participate were read the consent form, which they signed prior to the oral health evaluation.
Photocopies of the odontograms were made and identifying information was removed. Each photocopy and corresponding questionnaire was given a unique identifier. Oral health was measured by three variables: total number of carious teeth, total number of carious surfaces, and total number of missing teeth. For the study, incipient lesions, those not into the dentin, were excluded, which is consistent with oral health epidemiological and survey research.
Data regarding demographic, oral hygiene, professional dental care, sugar consumption, and drug use were obtained from personal interviews administered by the dental hygienist after the oral evaluation. Demographic variables included sex, age, race/ethnicity, education, marital status, and employment. Oral hygiene was measured by usual toothbrushing frequency using a 6-point scale from three or more times/day to less than weekly, and toothbrushing frequency when on drugs. The latter was obtained with the open-ended question, “When you were using drugs, how frequently did you brush your teeth?” Of 92 subjects’ responses (measured on the 6-point scale previously described), 32 stated they brushed the same as usual, 23 stated they never brushed when on drugs and were coded at the lowest frequency, four stated they brushed more when on drugs and were raised one usual frequency level, 20 stated they did not use drugs or only cigarettes and were coded at their usual frequency, and three subjects’ answers could not be coded. For regression analysis, the three were included using their respective usual frequencies. Professional dental care included the number of years since the last dental visit and the reason for the last dental visit. Consumption of eight types of sweetened beverages and food was measured with the same 6-point scale as toothbrushing. Sugar consumption was analyzed using two variables: soda (the frequency of soda consumption) and non-soda sugars (a summed variable of the other seven sugar items). For multivariate analysis, both sugar variables were rendered closer to scale by converting them to the common denominator of times per week. Participants were asked if they had ever used tobacco, alcohol, marijuana, methamphetamine, other stimulants, cocaine, and heroin and were given the option to name up to two additional drugs. Respondents were divided into users and non-users for each of the drugs for data analysis.
Data were entered in the computer by student research assistants and one of the authors. All data were verified and then analyzed using IBM SPSS Statistics 19 and SAS.
Distributions and descriptive statistics were calculated. Bivariate analysis was conducted to test for differences between users and non-users of methamphetamine. Continuous, normally distributed variables were compared using two-sample t tests, while Mann-Whitney U Tests were used for non-normally distributed and ordinal variables. Pearson’s chi-square or the Fisher’s Exact Test was used for comparing categorical variables. Bivariate analysis was also conducted to examine the association of covariates with the three dependent variables using Spearman’s Rho, Mann-Whitney U Tests, and Kruskal-Wallis Tests.
Because the primary objective was to describe the effect of methamphetamine use on oral health controlling for the influence of covariates, multivariate linear regression analysis was used. Separate regression models were analyzed for each of the three oral health dependent variables. As none of the oral health variables was normally distributed, they were transformed for regression analysis: caries with the square root transformation and missing teeth with the natural log transformation.35,36
The covariates included in the regression models were demographics (sex, age, race/ethnicity, and marital status), sugar consumption (soda and non-soda sugars), personal oral hygiene (toothbrushing frequency when on drugs), professional dental care (number of years since last the dental visit and reason for the last dental visit) and drug use (tobacco, alcohol, methamphetamine, marijuana, and cocaine). Heroin use was not included due to the small number of heroin users (n = 6). None of the sample used other stimulants.
In addition to fitting a main-effects-only regression model, interaction effects involving methamphetamine and other covariates were also examined. This was done by fitting separate regression models with a single interaction effect added to the main effects model. Interaction effects with a P value ≤ .10 were considered for possible inclusion in the final model. The presence of a significant interaction effect of any of these variables with methamphetamine indicates that the effect of methamphetamine on caries or missing teeth is moderated by this variable. Among the interaction effects that were tested, there were three variables that met the inclusion criteria: race/ethnicity, age, and frequency of toothbrushing when on drugs. Regression models were then fitted that included various combinations of these interaction variables. The extent to which each model provided the best fit was assessed by the Akaike Information Criterion.37
From the final model that included interaction effects, the effect of methamphetamine was then examined using the test of mean contrast to test for differences in dental caries or missing teeth between methamphetamine users and non-users at each level of the moderating variable. Because multiple tests were performed to test for the effect of methamphetamine (ie, two tests by race/ethnicity), the P values for these tests were adjusted using Bonferroni’s method.38
Results
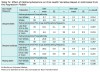
There were 174 individuals in the study, with only one individual declining to participate (99.4%). The average age was 30 years (SD = 8.3, 122 range 17 to 53), 85.6% were male, 81.6% were white, 50.6% had never been married, 49.5% had either graduated high school or obtained a GED, and 78.2% had been employed full-time prior to incarceration (Table I).
The main reasons for the last dental visit were a toothache (55.2%), checkup (28.2%), and other dental work (15.5%). More than half (n = 101, 57.9%) had not been to the dentist in the past year and the average number of years since the last dental visit was 4 (SD = 4.3).
Most subjects usually brushed their teeth once (39.7%) or twice a day (35.6%); however, when subjects were using drugs, 36.8% brushed once a day and only 27.5% brushed twice a day. While 2.3% of subjects usually brushed less than weekly, 14% brushed less than weekly when on drugs.
Almost half or more of the subjects reported that they ingested soda (83.3%), chips and/or snack crackers (59%), cake and/or cookies (54.3%), or candy (47.1%) at least once a day. Soda was consumed three or more times a day by 64.9% of the subjects for a mean consumption of 15.9 times per week. Non-soda sugars were consumed, on average, 34.7 times per week.
While the majority of subjects (82.8%) used multiple drugs, 12 subjects did not use any drugs, and 18 subjects used only one drug. Four drugs were used by more than half of the subjects: tobacco (86.8%), alcohol (58%), methamphetamine (54.6%), and marijuana (52.3%). Cocaine was used by 23.6% of the subjects and heroin by 3.4%. Fourteen subjects reported using other types of drugs.
Bivariate analysis determined significant associations between methamphetamine use and being white, being female, having visited the dentist in the previous year, having visited the dentist for a toothache, having consumed soda at the highest frequency, using multiple drugs, using tobacco, using marijuana, using cocaine, and using heroin (Table I).
Eighteen participants had no teeth with untreated dental caries and 32 had no missing teeth. Users had significantly higher numbers of carious teeth (P = .020), carious surfaces (P = .018) and missing teeth (P = .009) than those who had never used methamphetamine (Table II).
The significant bivariate associations between each covariate and the dependent variables of carious teeth and surfaces are as follows. Dental caries were significantly greater among those using methamphetamine (carious teeth: P = .020; surfaces: P = .018), being white (carious teeth: P = .016; surfaces: P = .014), consuming soda more frequently (carious teeth: P = .000; surfaces: P = .002), brushing once a day or less when on drugs (carious teeth: P = .031; surfaces: P = .050), and visiting the dentist for a toothache or other work (carious teeth: P = .030; surfaces: P = .005). The number of missing teeth was significantly greater among those using methamphetamine (P = .009), being older (P = .000), being male (P = .021), being married (P = .000), not visiting the dentist in the past year (P = .004), and visiting the dentist for a toothache or other work (P = .000).
Regression analyses to control for covariates in assessing the effect of methamphetamine use on dental caries showed a significant interaction between methamphetamine use and race/ethnicity (carious teeth: P = .039; surfaces: P = .023) and a significant interaction between methamphetamine use and toothbrushing frequency when on drugs (carious teeth: P = .044; surfaces: P = 0.035) (Table III). Among non-whites there were significantly more carious teeth and surfaces in methamphetamine users (n = 6) compared to non-users (n = 26) (Bonferroni adjusted P = .014 and P = .011, respectively). However, no significant effect of methamphetamine was seen among whites (carious teeth Bonferroni adjusted P = .367; carious surfaces Bonferroni adjusted P = .287) (Table IV). Likewise, among those who brushed their teeth less than once a day when on drugs, there were significantly more carious teeth and surfaces in methamphetamine users (n = 25) compared to non-users (n = 20) (Bonferroni adjusted P = .007 and P = .003, respectively). There was no significant effect of methamphetamine on carious teeth and surfaces (Bonferroni adjusted P = .216 and P = .221, respectively) among those who brushed their teeth at least once a day when on drugs (Table IV). Other significant covariates for dental caries were reason for last dental visit (carious teeth: P = .025; surfaces: P = .011) and soda (carious teeth: P = .026; surfaces: P = .030). Those who visited the dentist for a toothache or other work and those who more frequently consumed soda had more carious teeth and surfaces (Table III).
For missing teeth, regression analyses to assess the effect of methamphetamine use showed a significant methamphetamine and race/ethnicity interaction (P = .028) (Table III). This interaction indicated that the effect of methamphetamine on missing teeth differed within race/ethnicity categories, with significantly more missing teeth in whites who used methamphetamine (n = 89) than in whites who did not (n = 53) (Bonferroni adjusted P = .038). There was no significant association between methamphetamine use on missing teeth among non-whites (Bonferroni adjusted P = .431) (Table IV). Other significant covariates were age (P = .0001) and reason for last dental visit (P = .0001). Being older and visiting the dentist for a toothache or other work resulted in more missing teeth (Table III).
Discussion
Previous studies reported a lower percentage of methamphetamine users who brushed their teeth at least daily when on drugs (35.3% to 41%)30-33 than found in this study (72.8%). Only one study reported a significant bivariate relationship between methamphetamine use and tooth brushing when on drugs.32 While this study did not find significant bivariate relationships between methamphetamine use and usual toothbrushing and methamphetamine use and toothbrushing when on drugs, it did find a significant bivariate relationship between toothbrushing when on drugs and dental caries. Additionally, multivariate analysis of this data indicated that methamphetamine use results in statistically more dental caries for those who brush less than once a day when on drugs.
Previous methamphetamine studies did not include reason for dental visit, which this analysis found was related to both dental caries and missing teeth. In this study, subjects who saw the dentist for toothaches or other treatment had poorer oral health than those who saw the dentist for a check-up. In addition to the advanced stage of disease, the large number of missing teeth found in these prisoners may reflect the culture of dental care.39
In three previous studies, consumption of soda varied from 35.3%30 to 94%32 among methamphetamine users. This study found that 92.6% of methamphetamine users consumed soda. Morio et al found a significant difference in the percentage consuming soda between methamphetamine users and non-users, as was found in this study.32 However, Cretzmeyer et al31 and Brown et al30 did not. This analysis found that the frequency of soda consumption correlated with dental caries, as did Ravenel et al,7 but Cretzmeyer et al31 did not. When covariates were controlled, soda consumption remained significantly related to dental caries. None of the other sugar variables studied individually or as a combined frequency correlated with methamphetamine use or with dental caries. Sugar variables, including soda consumption, were not related to missing teeth.
In addition to this study, Cretzmeyer et al were the only ones to investigate the relationship between age and oral health.31 Although they found that methamphetamine users were significantly younger than their other-substance-abuse comparison group, logistic regression indicated that age was not related to oral health. In this study age was not related to methamphetamine use nor to dental caries; however, age was related bivariately and multivariately to missing teeth, with older inmates having more missing teeth.
Although methamphetamine users commonly use other illicit drugs,40 previous researchers7,30-33 did not investigate them. In this study, while use of tobacco, marijuana, cocaine, and heroin were significantly correlated with methamphetamine use, none of these drugs correlated with dental caries and missing teeth. Additionally, multivariate analyses controlled for these four drugs and none were found to be related to the oral health variables. However, polydrug use was high and this sample of 174 subjects was not adequate to consider all the interaction effects of the drugs with methamphetamine.
The findings that methamphetamine’s effects on dental caries are moderated by toothbrushing when on drugs, and that the reason for dental visit influences both caries and missing teeth, suggest intervention points. One intervention would focus on preventive behaviors. For persons with few dental caries, secondary preventive measures would comprise appropriate traditional home care and routine dental visits. However, many of the prisoners in this study are at the tertiary level and may require prescription strength fluoride toothpaste, frequent professional cleanings, and elimination of soda. Because methamphetamine use may alter saliva so that it is more acidic and has less buffering capacity, saliva testing and appropriate neutralizing and remineralizing agents should be considered.7 Drugs used to treat drug abuse should not have high sugar content.
Researchers have found that habituated oral health behaviors can withstand changes in a person’s social environment, and this underscores the importance of primary prevention.41 Had the methamphetamine users in this study had well-established oral care habits they would have maintained their usual higher toothbrushing frequency and regular dental visits when on drugs. This would have reduced the number and size of carious lesions for the prisoners who used methamphetamine. Given what is known about developing dental health habits, primary prevention should start at birth.42-45
Changing adults’ health behavior is not easy, nor is altering dental procedures in institutions. Research on dental hygienists’ role in providing preventive services to drug users has not been reported. However, given administrative support for establishing policies and funding, these interventions are within the scope of dental hygiene practice and thus could be provided cost-effectively by dental hygienists. It is likely that dental hygienists, especially those employed in rehabilitation or correctional facilities, could advocate for restrictions on access to sodas and other sugar intake similar to those for diabetic prisoners, for shorter intervals for prophylaxes and closer supervision of personal oral hygiene.
Another intervention to consider would be dental screenings for high school seniors, especially in states where methamphetamine use is prevalent. In the newly admitted prisoners in this study, by age 18, 63% of this high-risk group had tried methamphetamine. Thus, such a dental screening program may not only lead to early detection of dental caries and the prevention of destructive caries but may also lead to early identification of drug use.
While these interventions are primarily directed at dental caries, they also would address missing teeth. Osborn found that approximately 86% of prisoners aged 25 to 40 needed teeth extracted due to dental caries; for those younger than 25 and those older than 40, 65% needed extraction.46
A limitation of this study that may have influenced the results was that the number of missing teeth attributed to dental disease may have been overestimated because the reason for teeth being absent was not ascertained. In addition to dental disease, teeth could have been missing due to trauma and orthodontic care. Salive suggested that the higher mean number of missing teeth in the prisoners he studied, as compared to a national sample, may have been due to trauma.47
Additionally, there were three variables that were not captured completely: the upper limit of soda consumption, the lower limit of toothbrushing when on drugs, and a complete history of dental caries (because filled teeth were not charted as part of the oral examination at the IMCC). However, it is unlikely that these limitations on completeness altered the findings of this study.
Because the data were collected 16 years ago, this raises the question: Are the data still pertinent today? The authors believe they are for a number of reasons. Methamphetamine use still creates a meaningful and growing burden on healthcare facilities and penal institutions in Iowa.2,3 Methamphetamine used in 2014 in Iowa is purer than that which was used in 1998.3 Whether more pure methamphetamine would result in higher levels of decay is unknown. If it did, methamphetamine users would be further differentiated from non-users. The research methodology used in this study is consistent with current approaches and the Substance Abuse and Mental Health Services Administration’s measurement of methamphetamine use.40 The dental evaluations are conducted in the same manner at the IMCC, and dental caries and missing teeth are still common measures of oral health status. Dental caries preventive and treatment procedures have changed little since 1998.
The prison population was selected because the authors expected that prisoners would have more oral disease and more use of illicit drugs than the general population. Additionally, this population was accessible and was not expected to be affected by socially correct answers. Conducting the study within the confines of this particular penal institution restricted data collection to inmates evaluated by the staff dental hygienist and precluded using more than one examiner as well as conducting intra-examiner reliability tests.
The setting did allow for non-threatening, confidential, and routine implementation of the personal interviews. The structure of the interview and sequencing of items were done to be consistent, clear, and easy to answer, to enhance recall and unbiased responses, and to give equal attention to all drugs. While self-reported information is often considered suspect, it is the most common methodology to obtain personal information and it is the most practical in terms of privacy and expense. Donovan concluded that self-reported drug use can be accurate if the foregoing techniques of interview design and implementation are utilized.48
Future studies are needed to elucidate the role of methamphetamine use on oral health status. Large sample sizes are needed to study main effects regarding use of other drugs and to test the interaction effect regarding race/ethnicity found in this study among the small number (n = 6) of non-white users. Additional research using users and nonusers could test the validity of anecdotal information regarding the unique location and appearance of methamphetamine-associated caries. In addition to comparing users and nonusers, quantity and frequency of methamphetamine use and oral health should also be investigated. Another area of research would be to develop and test the effectiveness of interventions regarding oral hygiene, professional care, and soda consumption for methamphetamine users.
Conclusion
The effect of methamphetamine use on missing teeth was moderated by race/ethnicity, whereas the effect of methamphetamine use on dental caries was moderated by race/ethnicity and toothbrushing when on drugs. Methamphetamine use together with poor oral hygiene resulted in significantly more dental caries. As is evident from this study the relationship between methamphetamine use and oral health is complex. The findings from this study suggest that it may be possible to mitigate oral health problems associated with methamphetamine use through preventive oral hygiene programs. The avenues for further research stated above would add to the limited body of work on the relationship of methamphetamine use and oral health and would elucidate the role dental hygienists could play in reducing dental disease in methamphetamine users.
About the Authors
E. Marcia Boyer, PhD, is a former adjunct assistant professor in the Department of Preventive & Community Dentistry, College of Dentistry, The University of Iowa.
Nancy Jean Thompson, PhD, is an associate professor, Department of Community and Behavioral Health, College of Public Health, The University of Iowa.
Tracy J. Hill, RDH, BS, BA, is a dental hygienist at the Iowa Medical Classification Center, and an adjunct instructor at both Kirkwood Community College and The University of Iowa College of Dentistry.
M. Bridget Zimmerman, PhD, is a clinical professor and associate director, Biostatistics Core, Institute for Clinical & Transla-tional Science, Department of Biostatistics, College of Public Health, The University of Iowa.
Acknowledgments
The authors wish to thank: R.D. Axelson, PhD, associate professor, Department of Sociology, Director, Center for Social Research, North Dakota State University; K. Kelly, PhD, associate research scientist, Department of Occupational and Environmental Health, College of Public Health, the University of Iowa; J. Yang, PhD, associate professor, Department of Pediatrics, College of Medicine, The Ohio State University; and secretarial and research assistant support from the Department of Community and Behavioral Health.
References
1. Kraemer T, Maurer HH. Toxicokinetics of amphetamines: metabolism and toxicokinetic data of designer drugs, amphetamine, methamphetamine, and their N-alkyl derivatives. Ther Drug Monit. 2002;24(2):277-289.
2. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Treatment Episode Data Set (TEDS). In: Thompson N, ed. email ed. 2012: p. 1.
3. Governor’s Office of Drug Control Policy. Iowa Drug Control Strategy. Des Moines, Iowa: Governor’s Office of Drug Control Policy; 2013:58.
4. American Dental Association Division of Communications, Journal of the American Dental Association, American Dental Association Division of Scientific Affairs. For the dental patient ... methamphetamine use and oral health. J Am Dent Assoc. 2005;136(10):1491.
5. Mallat M. Meth mouth: a national scourge. J Indiana Dent Assoc. 2005;84(3):28-29.
6. Garcia-Godoy F, Hicks MJ. Maintaining the integrity of the enamel surface: the role of dental biofilm, saliva and preventive agents in enamel demineralization and remineralization. J Am Dent Assoc. 2008;139 Suppl:25s-34s.
7. Ravenel MC, Salinas CF, Marlow NM, et al. Methamphetamine abuse and oral health: a pilot study of “meth mouth.” Quintessence Int. 2012;43(3):229-237.
8. Saini T, Edwards PC, Kimmes NS, et al. Etiology of xerostomia and dental caries among meth¬amphetamine abusers. Oral Health Prev Dent. 2005;3(3):189-195.
9. Williams N, Covington JS, 3rd. Methamphetamine and meth mouth: an overview. J Tenn Dent Assoc. 2006;86(4):32-35.
10. Howe AM. Methamphetamine and childhood and adolescent caries. Aust Dent J. 1995;40(5):340.
11. Venker D. Crystal methamphetamine and the dental patient. Iowa Dent J. 1999;85(4):34.
12. Curtis EK. Meth mouth: a review of methamphetamine abuse and its oral manifestations. Gen Dent. 2006;54(2):125-129.
13. Donaldson M, Goodchild JH. Oral health of the methamphetamine abuser. Am J Health Syst Pharm. 2006;63(21):2078-2082.
14. Goodchild JH, Donaldson M. Methamphetamine abuse and dentistry: a review of the literature and presentation of a clinical case. Quintessence Int. 2007;38(7):583-590.
15. Goodchild JH, Donaldson M, Mangini DJ. Methamphetamine abuse and the impact on dental health. Dent Today. 2007;26(5):124,126,128-131.
16. Hamamoto DT, Rhodus NL. Methamphetamine abuse and dentistry. Oral Dis. 2009;15(1):27-37.
17. Heng CK, Badner VM, Schiop LA. Meth mouth. N York State Dent J. 2008;74(5):50-51.
18. Kessler B, Dinneen M. Methamphetamine: oral effects and treatment. Inside Dent. 2010;6(2):40-48.
19. Klasser GD, Epstein JB. The methamphetamine epidemic and dentistry. Gen Dent. 2006;54(6):431-439.
20. Naidoo S, Smit D. Methamphetamine abuse: a review of the literature and case report in a young male. SADJ. 2011;66(3):124-127.
21. Padilla R, Ritter AV. Meth mouth: methamphetamine and oral health. J Esthetic Restor Dent. 2008;20(2):148-149.
22. Rhodus NL, Little JW. Methamphetamine abuse and “meth mouth.” Northwest Dent. 2005;84(5):29-37.
23. Shaner J. Caries associated with methamphetamine abuse. J Mich Dent Assoc. 2002;84(9):42-47.
24. Shaner JW, Kimmes N, Saini T, Edwards P. “Meth mouth”: rampant caries in metham-phetamine abusers. AIDS Patient Care STDS. 2006;20(3):146-150.
25. Turkyllmaz I. Oral manifestations of “meth mouth”: a case report. J Contemp Contemp Dent Pract. 2010;11(1):E073-E080.
26. Chi D, Milgrom P. The oral health of homeless adolescents and young adults and determinants of oral health: preliminary findings. Spec Care Dentist. 2008;28(6):237-242.
27. Laslett AM, Dietze P, Dwyer R. The oral health of street-recruited injecting drug users: prevalence and correlates of problems. Addiction. 2008;103(11):1821-1825.
28. McGrath C, Chan B. Oral health sensations associated with illicit drug abuse. Br Dent J. 2005;198(3):159-162.
29. Walter A, Bachman SS, Reznik DA, et al. Methamphetamine use and dental problems among adults enrolled in a program to increase access to oral health services for people living with HIV/AIDS. Public Health Rep. 2012;127(Suppl 2):25-35.
30. Brown C, Krishnan S, Hursh K, et al. Dental disease prevalence among methamphetamine and heroin users in an urban setting: a pilot study. J Am Dent Assoc. 2012;143(9):992-1001.
31. Cretzmeyer M, Walker J, Hall JA, Arndt S. Methamphetamine use and dental disease: results of a pilot study. J Dent Child (Chic). 2007;74(2):85-92.
32. Morio KA, Marshall TA, Qian F, Morgan TA. Comparing diet, oral hygiene and caries status of adult methamphetamine users and nonusers: a pilot study. J Am Dent Assoc. 2008;139(2):171-176.
33. Shetty V, Mooney LJ, Zigler CM, et al. The relationship between methamphetamine use and increased dental disease. J Am Dent Assoc. 2010;141(3):307-318.
34. Marshall BD, Werb D. Health outcomes associated with methamphetamine use among young people: a systematic review. Addiction. 2010;105(6):991-1002.
35. Klugh H. Statistics: the essentials for research. Hillsdale, NJ. Erlbaum Associates Inc. 1986: p. 257.
36. Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. San Francicso, CA: Pearson: Allyn & Bacon. 2007.
37. Akaike H. A new look at the statistical model identification. IEEE Trans Automatic Contr. 1974;19(6):716-723.
38. Kleinbaum D. Applied Regressive Analysis and other multivariate variable methods. 1st ed. New York: Duxbury Press; 1998.
39. Bailit HL, Braun R, Maryniuk GA, Camp P. Is periodontal disease the primary cause of tooth extraction in adults? J Am Dent Assoc. 1987;114(1):40-45.
40. Department of Health and Human Services. 2005 National Survey on Drug Use and Health: National Findings. In: SAMSHA, ed: DHHS; 2006.
41. Astrom AN, Jakobsen R. Stability of dental health behavior: a 3-year prospective cohort study of 15-, 16- and 18-year-old Norwegian adolescents. Community Dent Oral Epidemiol. 1998;26(2):129-138.
42. Blinkhorn AS. Dental preventive advice for pregnant and nursing mothers—sociological implications. Int Dent J. 1981;31(1):14-22.
43. Honkala E. Oral health. In: Schou L, Blinkhorn AS, ed. Oral Health Promotion. Oxford, NY. Oxford University Press. 1993.
44. Tolvanen M, Lahti S, Poutanen R, et al. Children’s oral health-related behaviors: individual stability and stage transitions. Community Dent Oral Epidemiol. 2010;38(5):445-452.
45. Traeen B, Rise J. Dental health behaviours in a Norwegian population. Community Dent Health. 1990;7(1):59-68.
46. Osborn M, Butler T, Barnard PD. Oral health status of prison inmates—New South Wales, Australia. Aust Dent J. 2003;48(1):34-38.
47. Salive ME, Carolla JM, Brewer TF. Dental health of male inmates in a state prison system. J Public Health Dent. 1989;49(2):83-86.
48. Donovan DM, Bigelow GE, Brigham GS, et al. Primary outcome indices in illicit drug dependence treatment research: systematic approach to selection and measurement of drug use end-points in clinical trials. Addiction. 2012;107(4):694-708.