You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
A number of dental procedures cause acute post-procedural pain, making effective pain management for all patients an essential component of dental practice.1 Achieving adequate and safe pain relief may be more challenging in some patient populations, such as those with substance abuse or chronic pain disorders.2,3 However, pain following certain dental procedures can be anticipated, which provides dentists an opportunity to thoughtfully plan and optimize the management of acute pain.4
Overview of Evidence for Analgesic Use in Dental Pain
Postoperative pain following the surgical removal of impacted third molars is a frequently used analgesic model because of the consistency and intensity of the postoperative pain.4-6 This common procedure is performed under local anesthesia, usually with concomitant intravenous-conscious sedation or short-acting general anesthesia.7 The trauma to soft tissue and the maxillary and mandibular alveolar bone results in release of inflammatory and algesic mediators at the peripheral surgical sites. Predictably, 3 to 4 hours after surgery, 95% or more of individuals have moderate to severe pain that in clinical trials can be used to distinguish active drugs from placebo, and also detect differences between moderately effective and highly effective analgesics.4 In addition, these are relatively healthy patients who are not on confounding medications, with an average age of 20 years.8 Therefore, this model is common in pivotal double-blind, randomized, placebo-controlled trials for US Food and Drug Administration (FDA) approval of analgesics.
Several early oral surgery analgesic studies have assessed peripherally acting analgesics. Both aspirin 650 mg and acetaminophen (APAP) 650 mg produced significantly better pain-relief scores than placebo, with approximate equal analgesia.5 APAP and aspirin have linear dose-response curves with a ceiling effect thought to be in the neighborhood of 1,000 mg.4,5,9 The maximum daily doses of APAP and aspirin should not exceed 4,000 mg, and lower doses might often deliver adequate analgesia with a lower risk of rare but serious adverse events.9 When calculating total daily doses, it is important to appreciate that opioid combination products and over-the-counter (OTC) medications may contain APAP or aspirin.4,10 To go beyond the analgesic effects of maximum doses of aspirin or APAP, an optimal or near-optimal dose of aspirin or APAP can be combined with a centrally acting opioid (such as oxycodone 5 mg, hydrocodone 10 mg, codeine 60 mg, or tramadol 75 mg).11 In several studies, an opioid alone produced similar or inferior postoperative pain relief to aspirin or APAP alone.4,6,11-13 However, combining an opioid with aspirin or APAP produced an additive analgesic effect, which is consistent with opioids producing analgesia by a mechanism different from the peripherally acting agents.4,6,11-13 Because many combination formulations contain less than optimal doses of the peripherally acting component, under-dosing of these agents is common.1 For example, a single tablet of one of the strengths of Percocet® (APAP 325 mg/oxycodone 5 mg tablets) contains only 325 mg of APAP. The optimal doses of aspirin or APAP to prescribe when using these combination products has been reported to be 600 mg to 1,000 mg.14 Increasing the number of doses of combination products to achieve higher aspirin or APAP doses also increases the opioid dose. So while the increased doses tend to be more efficacious, they also induce a higher incidence of opioid-related side effects.12,14,15 In addition, on January 13, 2011, the FDA mandated that manufacturers of APAP/opioid combination drugs limit the amount of APAP to no more than 325 mg in each tablet or capsule in an effort to reduce the incidence of APAP-associated overdose and accompanying hepatotoxicity.16
The newer nonsteroidal anti-inflammatory drugs (NSAIDs) at the upper end of their dose-response curve appear significantly more efficacious than APAP or aspirin 650 mg to 1,000 mg.4 In the United States, the current gold-standard analgesic in moderate to severe postoperative dental pain is ibuprofen 400 mg,17,18 which is as effective as codeine 60 mg with aspirin 650 mg.13 There are too few studies to demonstrate a definitive advantage of ibuprofen 600 mg or 800 mg over 400 mg in acute postoperative dental pain, and one study found no difference in analgesic effectiveness between ibuprofen 400 mg and 800 mg.19,20 Similarly to the early studies of APAP and aspirin in postoperative dental pain, ibuprofen 400 mg alone is a more effective analgesic than single-entity morphine 60 mg, oxycodone 5 mg, and the novel, centrally acting analgesic tapentadol at 50-mg, 75-mg, and 100-mg dosage strengths.21,22 It is thought that the anti-inflammatory and analgesic properties of NSAIDs (and most of their side effects) result from their inhibition of cyclooxygenase (COX)—a key enzyme in the production of postoperative pain and inflammation due to its ability to convert arachidonic acid to prostaglandins.4 Aspirin is unique in inactivating COX by irreversible acetylation, whereas the newer NSAIDs are reversible competitive inhibitors of COX.4 A number of NSAIDs are available in the United States, which do differ in terms of potential for gastrointestinal (GI) toxicity (ibuprofen demonstrates the lowest relative risk) and platelet inactivation.4
Ibuprofen 400 mg combined with an opioid has a faster onset of effect and greater peak effects than ibuprofen 400 mg alone.22 Pain relief with oxycodone 5 mg/ibuprofen 400 mg is superior to that achieved with oxycodone 5 mg/APAP 325 mg or hydrocodone 7.5 mg/APAP 500 mg.23 Due to their different mechanisms of action, there is also an emerging compilation of study data which supports the strategy of combining an NSAID with APAP to provide analgesia greater than either APAP or the NSAID alone.24-27 It was reported in a systematic review that the combination of an NSAID plus APAP provided pain relief greater than the NSAID alone in 9 of 14 postoperative pain studies.25 With respect to postoperative dental pain, five of six studies showed reduced pain intensity and increased pain relief with the combination compared with the NSAID alone.24-29 In the dental pain studies that displayed analgesic enhancement, APAP 500 mg to 1,000 mg was combined with the NSAID.24,26-29
Other Therapeutic Approaches
Preemptive NSAIDs
Studies have demonstrated that preoperative administration of ibuprofen delays the onset of pain (by more than 100 minutes compared with placebo) and lessened the severity of postoperative dental pain as the effect of the local anesthetic dissipated, without increased side effects.30,31 The beneficial effects of preemptive NSAID use is further illustrated by a study that showed that preoperative and postoperative administration of flurbiprofen achieved superior pain relief to APAP alone or in combination with oxycodone.32 This data supports the clinical strategy of administering an NSAID an hour before or immediately after the surgical procedure, and then dosing the NSAID on a fixed around-the-clock schedule for the first 24 to 48 hours. Preoperative dosing of NSAIDs is often avoided by dentists because of concerns that increased bleeding will result. While the amount of bleeding was not directly measured, the preoperative administration of a single dose of ibuprofen 400 mg or flurbiprofen 50 mg to 100 mg did not result in any significant increase in intraoperative or postoperative bleeding.30-32 Short-term use of ibuprofen in particular has been shown to only marginally reduce platelet aggregation compared to other NSAIDs such as ketoprofen or aspirin.33,34
Postoperative Long-Acting Local Anesthetic
Another therapeutic approach to attenuate postoperative pain is the administration of the long-acting local anesthetic, bupivacaine 0.5% with 1:200,000 epinephrine, during the immediate postoperative period.35,36 Patients who had third molar extractions under general anesthesia were randomized to one of four groups: preoperative lidocaine 2% with 1:100,000 epinephrine, postoperative bupivacaine 0.5% with 1:200,000 epinephrine, both, or placebo injections.36 In the bupivacaine groups, pain was not only diminished in the immediate postoperative period (0 to 4 hours), but also 48 hours after surgery compared with placebo and lidocaine alone.36 This strategy is most effective if combined with preemptive and around-the-clock NSAIDs during the immediate postoperative period.
Relative Efficacy of Oral Analgesics: Synthesis of Evidence
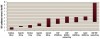
A meta-analysis of randomized, double-blind studies of analgesics for acute pain after third molar extraction compared the relative efficacy of a single dose of several oral analgesics.37 The number of patients with moderate or severe pain achieving at least 50% maximum pain relief over 4 to 6 hours was used to calculate the number needed to treat (NNT) with active drug to get one additional patient with at least 50% pain relief compared with placebo (Figure 1) (the lower the NNT, the more effective the analgesic).37 Single-dose diclofenac 100 mg had the lowest NNT, followed closely by ibuprofen 400 mg.37 It is important to note that the administration of diclofenac 100 mg will make it difficult to stay within maximum recommended daily dose guidelines for this drug, which is 150 mg per day. In contrast, ibuprofen 400 mg represents only one sixth of the maximum recommended daily dose guideline of 2,400 mg. Figure 1 also demonstrates that to the probable surprise of many clinicians, ibuprofen 400 mg displays an NNT that is approximately half that of the combination of APAP 600 mg plus codeine 60 mg (2.2 vs 4.3).
In general postsurgical (non-dental) pain models, the NNT with single-dose ibuprofen 200 mg, 400 mg, and 600 mg were all similar at around 2.5 (Figure 2); although ibuprofen 800 mg had a lower NNT, this was based on only one study.19 Ibuprofen was at least as effective as optimal doses of combination opioid/APAP therapy and was superior to single-entity oxycodone 15 mg or APAP 325 mg combined with oxycodone 5 mg.38
Practice Patterns
A survey of dental prescribing practices among oral surgeons after third molar extraction found that the preferred peripherally acting postoperative analgesic is ibuprofen (73.5%), but 85% of oral surgeons also almost always prescribe a centrally acting opioid analgesic, with the drug of choice being hydrocodone/APAP (64%).1 On average, 20 tablets of hydrocodone/APAP are prescribed, with instructions in 96% of cases to "take as needed for pain."1
Most of the available data on dentists' analgesic prescribing practices focus on oral surgeons. A statewide survey was conducted in West Virginia to evaluate dentists' analgesic prescribing patterns, with an emphasis on opioids, and experiences with patient drug diversion and substance abuse.39 Data from 52% of all dentists in West Virginia (mainly general dental practitioners) showed that the most frequently prescribed analgesic if no opioids were prescribed was NSAIDs (64%), followed by APAP (28%).39 The most prescribed opioid was hydrocodone/APAP (73%).39 The amount of opioids given after third molar extraction varied greatly, but 20 doses and a 3-day supply was most common. The pattern of days of therapy for the most common opioids prescribed was similar following root canal.39
The question raised by these two studies is whether 20 tablets of an opioid/APAP combination agent is an appropriate amount after third molar extraction and what happens to unused opioids, if anything. Addressing the first part of the question, there is not a large amount of data about the number of days that dental patients are in pain after the procedure—but some studies provide an indication. In a study of dental impaction surgery causing moderate to severe pain, patients typically took NSAIDs (ibuprofen or meclofenamate) for between 4 and 6 days.18 After dental implant surgery, the typical dosing period with APAP/hydrocodone was between 2 and 3 days.40 However, there needs to be flexibility in the number of days supply, because some people will legitimately need analgesics for 6 or 7 days, with 24% in one study still taking analgesics on postoperative day 10 after removal of four third molars.8
The second part of the question—what happens to unused opioids—is an important public health problem because opioid analgesics are commonly diverted, misused, or abused in the United States.41 The number of prescriptions dispensed in 2008 for opioid/APAP combination drugs containing hydrocodone, oxycodone, propoxyphene, and codeine were ranked 1st, 25th, 55th, and 70th, respectively, of all prescribed medications in the United States.42 The National Survey on Drug Use and Health (NSDUH) found that among persons aged 12 or older in 2007 to 2008 who used pain relievers non-medically (without a prescription) in the past 12 months, 56% got the pain relievers they most recently used from a friend or relative for free.41 Another 9% bought them from a friend or relative, and 5% took them from a friend or relative without asking.41 Nearly one fifth (18%) indicated that they got the drugs they most recently used through a prescription from one doctor.41 In 82% of the instances where non-medical users of prescription pain relievers obtained the drugs from a friend or relative for free, the individuals indicated that their friend or relative had obtained the drugs from just one doctor.41 Data from Utah showed that 72% of respondents who were prescribed an opioid had leftover medication, and 71% of those with leftover medication kept it.43 This demonstrates the importance that all clinicians—including dentists—prescribe no more than the number of doses needed based on the usual duration of pain severe enough to require opioids for that condition43; further research in this area is warranted in order to better guide dentists. In addition, clinicians must counsel patients to dispose of unused medication once the condition has resolved.43 The Office of National Drug Control Policy guidelines for the disposal of prescription drugs instructs patients not to flush prescription drugs down the toilet or drain unless the label or accompanying patient information specifically instructs them to do so.44 Patients should take advantage of community prescription drug take-back programs.45 If such programs are not available, patients can access an online FDA-maintained list of medicines recommended for flushing.46
Recommendations for Analgesic Prescribing for Acute Dental Pain
After a review of the literature, a flexible analgesic strategy for the management of acute pain developed in 1995 by the American Association of Endodontists was selected by the authors as a template for an updated set of acute dental pain prescribing recommendations.47 Input from other published guidelines was also incorporated into the present recommendations.48-50 The revisions that were made were derived from the review of clinical trial and meta-analysis data in both dental and non-dental acute postoperative pain, together with the FDA mandate concerning prescription APAP dosages.16 The recommendations are based on procedures that are likely to induce mild, moderate, or severe pain (Figure 3). This therapeutic paradigm for pain management considers NSAIDs as the first line drugs in most cases of postoperative dental pain based on evidence that optimal doses of NSAIDs are superior in efficacy to single-entity opioids, and are at least as efficacious as optimal doses of peripheral/opioid combination drugs. NSAIDs also have a more favorable side-effect profile than agents that contain an opioid.
For patients who can tolerate NSAIDs, ibuprofen 200 mg to 400 mg as needed for pain every 4 to 6 hours is the gold standard for mild pain. If this regimen provides inadequate pain relief, or it is anticipated that the patient will have moderate pain, ibuprofen 400 mg to 600 mg around-the-clock every 4 to 6 hours for the first 24 hours is recommended, followed by ibuprofen 400 mg as needed for pain every 4 to 6 hours. If ibuprofen 400 mg to 600 mg provides inadequate pain relief or moderately severe pain is anticipated, ibuprofen 400 mg to 600 mg plus APAP 500 mg every 6 hours is recommended around-the-clock for the first 24 hours. If that is inadequate, or if severe postoperative pain is anticipated, ibuprofen 400 mg to 600 mg plus APAP 650 mg, combined with an opioid equivalent of hydrocodone 10 mg every 6 hours for the first 48 hours is recommended.
For patients in whom NSAID-like drugs are contraindicated, APAP 650 mg to 1,000 mg is the first-line analgesic. If this regimen provides inadequate pain relief, or it is anticipated that the patient will have moderate pain, APAP 650 mg plus hydrocodone 10 mg around-the-clock every 6 hours for 24 hours is suggested; then APAP 650 mg as needed for pain every 6 hours. If the pain relief is inadequate or severe pain is anticipated, APAP 650 mg and an opioid equivalent to oxycodone 10 mg around-the-clock every 6 hours for 48 hours is recommended (nuisance side effects should be anticipated in an opioid-naïve individual); then APAP 650 mg to 1,000 mg as needed for pain every 6 hours.
Additional considerations are the use of the long-acting local anesthetic, bupivacaine, immediately after the completion of the surgical procedure, to reduce postoperative pain in both the immediate and distant postoperative period; and the use of preemptive NSAIDs to delay the onset of postoperative dental pain.
Special Populations
Substance Abuse Disorders
Dentists should routinely at least ask new patients about their history of addiction or substance abuse—however, in the West Virginia survey of dental professionals, 36% of respondents acknowledged not doing so.39 The NSDUH reported that the rate of current (past-month) illicit drug use among persons aged 12 or older in 2008 was 8%41—therefore, it is not unreasonable that dentists should expect to encounter such patients in their practice. Patients with a history of substance abuse include those that are in drug-free recovery, those that are in recovery with adjuvant pharmacotherapy for prevention of relapse, and those that have active disease—these groups each have unique challenges (eg, how to manage acute pain in a patient on buprenorphine or methadone maintenance therapy). In addition, an estimated 6% to 10% of the population has attended Alcoholics Anonymous at some point—because of this prevalence of alcoholism, it is likely that dentists will be faced with the need to manage acute pain in a recovering alcoholic.2 Alcoholics may be at greater risk for the hepatotoxic effects of APAP and the ulcerogenic effects of NSAIDs.51 Dental professionals must learn to recognize these individuals, determine their status in the recovery process, and establish practices to manage their acute pain appropriately.2
It is important to consult with such patients' primary care provider, as well as the addiction treatment provider.2 Dental professionals should also collaborate with patients' family members or support network, particularly if it is established that a controlled substance is necessary for their care (eg, have a "trusted other" dispense each dose of medication rather than giving the patient unsupervised control over the medication).2 It is recommended that patients be encouraged to intensify their involvement in a recovery program before and after dental treatment that may involve surgery or anticipated postoperative pain.2 Informed consent—including the risk of initiating a relapse—and strict parameters for treatment are essential, and around-the-clock rather than PRN administration of opioids is recommended to provide timely and effective pain relief and reduce the likelihood that inadequate pain relief will be misinterpreted as drug-seeking behavior.2
Opioid analgesic tolerance may be problematic in patients enrolled in methadone or buprenorphine maintenance programs. Additional therapy with opioids for anticipated acute pain should always be discussed with their buprenorphine or methadone maintenance therapy prescriber.3 Alternatively, the addition of an NSAID to a buprenorphine or methadone regimen is also a reasonable option because of the proven additive analgesic effects of combined NSAIDs and opioids.13,22,23
Because community dentists see patients frequently and develop long-term relationships with them, they are in a unique position for screening in a public health role. In order to be able to direct patients that they identify as in need of substance abuse treatment, they should become familiar with the American Society of Addiction Medicine's Patient Placement Criteria, and begin to investigate what addiction resources are available in their community.52
Renal and Hepatic Disease
Because toxicities associated with peripherally acting analgesics include renal and hepatic disease, caution is indicated when using these agents in patients with a history of such disorders.4,51,53,54 Hepatotoxicity is extremely rare with proper use of the currently available analgesics and is most often associated with APAP overdose.4 However, because APAP is so commonly included in OTC and prescription combination formulations, unintentional overdose is often reported.53,54 It has been reported that patients older than 65 years are at greater risk for acute liver toxicity with prolonged APAP therapy, although this finding may relate primarily to concomitant drug use in this population.4
Future Research Agendas in Acute Dental Pain
Research is needed in a number of areas related to the management of acute postoperative pain in the dental setting. Gaps in current pharmacologic knowledge include the efficacy of prescribing analgesics at fixed intervals versus as needed; demographic, behavioral, and genetic factors that potentially predict pain relief efficacy, adverse outcomes, and abuse; the utility of NSAID/APAP combinations in limiting the need for opioid analgesics; and the utility of long-acting local anesthetics to manage postoperative pain. It is also necessary to better understand practice patterns for pain management and analgesic use (both opioid and non-opioid) among general dentists and dental specialists, their perceptions of risk and safety of opioid analgesics, and their awareness about the increasing problem of prescription drug misuse and abuse; and guide these practitioners in optimal and safe prescribing of analgesics for acute pain in all patients.
Acknowledgment
The authors of this article are extremely grateful for the editorial assistance that Angela T. Casey provided throughout the development of this manuscript.
References
1. Moore PA, Nahouraii HS, Zovko JG, Wisniewski SR. Dental therapeutic practice patterns in the U.S. II. Analgesics, corticosteroids, and antibiotics. Gen Dent. 2006;54(3):201-207.
2. Lindroth JE, Herren MC, Falace DA. The management of acute dental pain in the recovering alcoholic. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95(4):432-436.
3. Heit HA, Gourlay DL. Buprenorphine: new tricks with an old molecule for pain management. Clin J Pain. 2008;24(2):93-97.
4. Hersh EV, Moore PA, Ross GL. Over-the-counter analgesics and antipyretics: a critical assessment. Clin Ther. 2000;22(5):500-548.
5. Cooper SA. Comparative analgesic efficacies of aspirin and acetaminophen. Arch Intern Med. 1981;141(3):282-285.
6. Cooper SA. Models for clinical assessment of oral analgesics. Am J Med. 1983;75(5A):24-29.
7. Moore PA, Nahouraii HS, Zovko JG, Wisniewski SR. Dental therapeutic practice patterns in the U.S. I. Anesthesia and sedation. Gen Dent. 2006;54(2):92-98.
8. Snyder M, Shugars DA, White RP, Phillips C. Pain medication as an indicator of interference with lifestyle and oral function during recovery after third molar surgery. J Oral Maxillofac Surg. 2005;63(8):1130-1137.
9. McQuay HJ, Moore RA. Dose-response in direct comparisons of different doses of aspirin, ibuprofen and paracetamol (acetaminophen) in analgesic studies. Br J Clin Pharmacol. 2007;63(3):271-278.
10. Schilling A, Corey R, Leonard M, Eghtesad B. Acetaminophen: old drug, new warnings. Cleve Clin J Med. 2010;77(1):19-27.
11. Beaver WT. Aspirin and acetaminophen as constituents of analgesic combinations. Arch Intern Med. 1981;141(3):293-300.
12. Cooper SA, Precheur H, Rauch D, et al. Evaluation of oxycodone and acetaminophen in treatment of postoperative dental pain. Oral Surg Oral Med Oral Pathol. 1980;50(6):496-501.
13. Cooper SA, Engel J, Ladov M, et al. Analgesic efficacy of an ibuprofen-codeine combination. Pharmacotherapy. 1982;2(3):162-167.
14. Cooper SA. Treating acute pain: do's and don'ts, pros and cons. J Endod. 1990;16(2):85-91.
15. Hersh EV, Desjardins PJ, Trummel CL, Cooper SA. Nonopioid analgesics, nonsteroidal antiinflammatory drugs, and antirheumatic and antigout drugs. In: Yagiela JA, Dowd FJ, Johnson B, et al, eds. Pharmacology and Therapeutics for Dentistry. 6th ed. St. Louis, MO: Elsevier Mosby Saunders; 2010.
16. FDA Limits acetaminophen in prescription combination products; requires liver toxicity warning. 2011. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm239894.htm. Accessed March 8, 2011.
17. Cooper SA. Five studies on ibuprofen for postsurgical dental pain. Am J Med. 1984;77(1A):70-77.
18. Hersh EV, Cooper S, Betts N, et al. Single dose and multidose analgesic study of ibuprofen and meclofenamate sodium after third molar surgery. Oral Surg Oral Med Oral Pathol. 1993;76(6):680-687.
19. Derry C, Derry S, Moore RA, McQuay HJ. Single dose oral ibuprofen for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009;(3):CD001548.
20. Winter L, Jr., Bass E, Recant B, Cahaly JF. Analgesic activity of ibuprofen (Motrin) in postoperative oral surgical pain. Oral Surg Oral Med Oral Pathol. 1978;45(2):159-166.
21. Kleinert R, Lange C, Steup A, et al. Single dose analgesic efficacy of tapentadol in postsurgical dental pain: the results of a randomized, double-blind, placebo-controlled study. Anesth Analg. 2008;107(6):2048-2055.
22. Van Dyke T, Litkowski LJ, Kiersch TA, et al. Combination oxycodone 5 mg/ibuprofen 400 mg for the treatment of postoperative pain: a double-blind, placebo- and active-controlled parallel-group study. Clin Ther. 2004;26(12):2003-2014.
23. Litkowski LJ, Christensen SE, Adamson DN, et al. Analgesic efficacy and tolerability of oxycodone 5 mg/ibuprofen 400 mg compared with those of oxycodone 5 mg/acetaminophen 325 mg and hydrocodone 7.5 mg/acetaminophen 500 mg in patients with moderate to severe postoperative pain: a randomized, double-blind, placebo-controlled, single-dose, parallel-group study in a dental pain model. Clin Ther. 2005;27(4):418-429.
24. Breivik EK, Barkvoll P, Skovlund E. Combining diclofenac with acetaminophen or acetaminophen-codeine after oral surgery: a randomized, double-blind single-dose study. Clin Pharmacol Ther. 1999;66(6):625-635.
25. Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110(4):1170-1179.
26. Mehlisch DR, Aspley S, Daniels SE, Bandy DP. Comparison of the analgesic efficacy of concurrent ibuprofen and paracetamol with ibuprofen or paracetamol alone in the management of moderate to severe acute postoperative dental pain in adolescents and adults: a randomized, double-blind, placebo-controlled, parallel-group, single-dose, two-center, modified factorial study. Clin Ther. 2010;32(5):882-895.
27. Mehlisch DR, Aspley S, Daniels SE, et al. A single-tablet fixed-dose combination of racemic ibuprofen/paracetamol in the management of moderate to severe postoperative dental pain in adult and adolescent patients: a multicenter, two-stage, randomized, double-blind, parallel-group, placebo-controlled, factorial study. Clin Ther. 2010;32(6):1033-1049.
28. Haglund B, von Bültzingslöwen I. Combining paracetamol with a selective cyclooxygenase-2 inhibitor for acute pain relief after third molar surgery: a randomized, double-blind, placebo-controlled study. Eur J Oral Sci. 2006;114(4):293-301.
29. Menhinick KA, Gutmann JL, Regan JD, et al. The efficacy of pain control following nonsurgical root canal treatment using ibuprofen or a combination of ibuprofen and acetaminophen in a randomized, double-blind, placebo-controlled study. Int Endod J. 2004;37(8):531-541.
30. Dionne RA, Cooper SA. Evaluation of preoperative ibuprofen for postoperative pain after removal of third molars. Oral Surg Oral Med Oral Pathol. 1978;45(6):851-856.
31. Dionne RA, Campbell RA, Cooper SA, et al. Suppression of postoperative pain by preoperative administration of ibuprofen in comparison to placebo, acetaminophen, and acetaminophen plus codeine. J Clin Pharmacol. 1983;23(1):37-43.
32. Dionne RA. Suppression of dental pain by the preoperative administration of flurbiprofen. Am J Med. 1986;80(3A):41-49.
33. Stichtenoth DO, Tsikas D, Gutzki FM, Frolich JC. Effects of ketoprofen and ibuprofen on platelet aggregation and prostanoid formation in man. Eur J Clin Pharmacol. 1996;51(3-4):231-234.
34. Jackson DL, Moore PA, Hargreaves KM. Preoperative nonsteroidal anti-inflammatory medication for the prevention of postoperative dental pain. J Am Dent Assoc. 1989;119(5):641-647.
35. Moore PA. Long-acting local anesthetics: a review of clinical efficacy in dentistry. Compendium. 1990;11(1):22-30.
36. Gordon SM, Brahim JS, Dubner R, et al. Attenuation of pain in a randomized trial by suppression of peripheral nociceptive activity in the immediate postoperative period. Anesth Analg. 2002;95(5):1351-1357.
37. Barden J, Edwards JE, McQuay HJ, et al. Relative efficacy of oral analgesics after third molar extraction. Br Dent J. 2004;197(7):407-411.
38. Gaskell H, Derry S, Moore RA, McQuay HJ. Single dose oral oxycodone and oxycodone plus paracetamol (acetaminophen) for acute postoperative pain in adults. Cochrane Database Syst Rev 2009;(3):CD002763.
39. Tufts Health Care Institute Program on Opioid Risk Management. Executive summary. The role of dentists in preventing opioid abuse. Tufts Health Care Institute Program on Opioid Risk Management 12th Summit Meeting. March 11-12, 2010. www.thci.org/opioid/mar10docs/executivesummary.pdf. Accessed May 9, 2010.
40. Biron RT, Hersh EV, Barber HD, Seckinger RJ. A pilot investigation: post-surgical analgesic consumption by dental implant patients. Dentistry. 1996;16(3):12-13.
41. Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health. National Findings. Rockville, MD. Office of Applied Studies, NSDUH Series: H-36; 2009. DHHS Publication No. SMA 09-4443.
42. Top 200 drugs for 2008 by number of U.S. prescriptions dispensed. www.rxlist.com/script/main/hp.asp. Accessed May 9, 2010.
43. Centers for Disease Control and Prevention (CDC). Adult use of prescription opioid pain medications—Utah, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(6):153-157.
44. The White House, Office of National Drug Control Policy. Proper disposal of prescription drugs. Federal guidelines. 2009. www.whitehousedrugpolicy.gov/publications/pdf/prescrip_disposal.pdf. Accessed May 9, 2010.
45. The White House, Office of National Drug Control Policy. National drug control strategy. 2010. www.whitehousedrugpolicy.gov/publications/policy/ndcs10/ndcs2010.pdf. Accessed May 9, 2010.
46. US Food and Drug Administration. Information for consumers (drugs). Disposal by flushing of certain unused medicines: what you should know. 2009. www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/EnsuringSafeUseofMedicine/SafeDisposalofMedicines/ucm186187.htm. Accessed May 9, 2010.
47. American Association of Endodontists. Management of acute pain. Endodontics Colleagues for Excellence. 1995;Spring/Summer:1-4.
48. Troullos ES, Freeman RD, Dionne RA. The scientific basis for analgesic use in dentistry. Anesth Prog. 1986;33(3):123-138.
49. Hargreaves KM, Troullos ES, Dionne RA. Pharmacologic rationale for the treatment of acute pain. Dent Clin North Am. 1987;31(4):675-694.
50. Phero JC, Becker D. Rational use of analgesic combinations. Dent Clin North Am. 2002;46(4):691-705.
51. Hersh EV, Pinto A, Moore PA. Adverse drug interactions involving common prescription and over-the-counter analgesic agents. Clin Ther. 2007;29(suppl):2477-2497.
52. American Society of Addiction Medicine. American Society of Addiction Medicine's (ASAM) Second Edition-Revised of Patient Placement Criteria (ASAM PPC-2R). 2007.
53. Larson AM, Polson J, Fontana RJ, et al. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology. 2005;42(6):1364-1372.
54. Guggenheimer J, Moore PA. The therapeutic applications of and risks associated with acetaminophen use: a review and update. J Am Dent Assoc. 2011;142(1):38-44.
About the Authors
Elliot V. Hersh, DMD, MS, PhD
Professor and Division Director of Pharmacology
Oral and Maxillofacial Surgery and Pharmacology, School of Dental Medicine
University of Pennsylvania
Philadelphia, Pennsylvania
William T. Kane, DDS, MBA
Private Practice
Dexter, Missouri
Michael G. O'Neil, PharmD
Associate Professor of Pharmacy Practice
Director for the Center of Excellence for the Education and Prevention of Drug Diversion and Substance Abuse
University of Charleston School of Pharmacy
Charleston, West Virginia
George A. Kenna, PhD, RPh
Assistant Professor of Psychiatry
Center for Alcohol and Addiction Studies, Brown University
Providence, Rhode Island
Nathaniel P. Katz, MD
Adjunct Assistant Professor of Anesthesia
Tufts University School of Medicine
Boston, Massachusetts
Stephanie Golubic, DMD, MBE
Orthodontic Resident
University of North Carolina School of Dentistry
Chapel Hill, North Carolina
Paul A. Moore, DMD, PhD, MPH
Professor of Pharmacology and Chair
Department of Dental Anesthesiology, School of Dental Medicine
University of Pittsburgh
Pittsburgh, Pennsylvania